Types of Diabetes - PowerPoint PPT Presentation
1 / 14
Title:
Types of Diabetes
Description:
Slow in offset (up to 6h) - risk post-prandial hypo. Problems with subcutaneous Insulin ... Modifiers of Post-Prandial Hyperglycaemia (PPHG) ... – PowerPoint PPT presentation
Number of Views:297
Avg rating:3.0/5.0
Title: Types of Diabetes
1
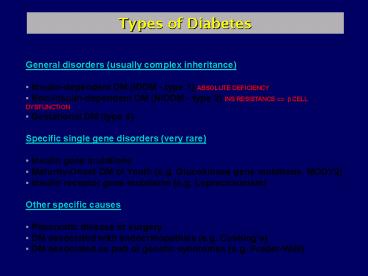
Types of Diabetes
- General disorders (usually complex inheritance)
- Insulin-dependent DM (IDDM - type 1) ABSOLUTE
DEFICIENCY - Non-Insulin-dependent DM (NIDDM - type 2) INS
RESISTANCE ? ? CELL DYSFUNCTION - Gestational DM (type 4)
- Specific single gene disorders (very rare)
- Insulin gene mutations
- Maturity-Onset DM of Youth (e.g. Glucokinase
gene mutations, MODY2) - Insulin receptor gene mutations (e.g.
Leprechaunism) - Other specific causes
- Pancreatic disease or surgery
- DM associated with endocrinopathies (e.g.
Cushings) - DM associated as part of genetic syndromes (e.g.
Prader-Willi)
2
Incidence of Diabetes (/100,000)
43 Finland 17 UK 1 Japan
IDDM
Ethnic variation (USA)
5000 Pimas 540 African 440 White
NIDDM
800 S Europe 100 N Europe
3
Drug Therapy I - Insulin
Human peptide sequence Pig and beef insulin
differ by 1 (AlaB30Thr) and 2 (ThrA8Ala,
ileA10Val) amino acids respectively.
- Typical production by non-diabetic adult is
0.2-0.5 U/kg/day - Approx 5050 split between basal and prandial (in
response to meals) - Short plasma t1/2 of 5-6 mins
- 50 cleared through liver so portal venous gt
systemic
4
Problems with subcutaneous Insulin
- Absorption variable and dependent on
- Short-acting
- Formulation Intermediate-acting (complexed with
protamine) - Long-acting (crystal suspensions with Zn)
- Site Abdomengtbuttockgtant. thighgtdorsal arm
- Depth intramuscular gt subcutaneous
- Absorption from these sites gives unphysiological
INS profiles - Compared to IV administration
- Gives systemic levels gt portal vein.
- Slow in onset (30-120m for peak levels)
- Slow in offset (up to 6h) - risk post-prandial
hypo
5
Common Insulin Regimens
BD regimen using fixed mixture of soluble and
intermediate-acting INS
BD or OD long-acting INS with short-acting
soluble with each meal.
Profile in C provided using a continuous SC pump
6
Drug therapy II Sulphonylureas
- - 1st generation e.g. chlorpropamide, tolbutamide
LARGELY OBSOLETE - - 2nd generation e.g. glibenclamide, gliclazide
- Actions
- Acutely release INS by depolarising ?-islet
cells (block iKATP) - Effect not sustained chronically
- ? Significant extapancreatic effects e.g.
upregulation of INS receptors - 2nd generation v potent (100xgt1st)
- Effective o.d. despite short t1/2 (lt5h)
- Side effects
- Hypoglycaemia (may be prolonged if long t1/2)
- Hyponatraemia (potentiate ADH action)
- Flushing (disulfiram-like)
- Chlorpropamide worst offender
7
Drug therapy III antihyperglycaemics
- BIGUANIDES (metformin)
- No effect on insulin release do not cause
hypoglycaemia even in over dose - Appears to have post-receptor effect on INS
action - Typically used in combination with a
sulphonylurea - Lactic acidosis a rare problem (lt1 in 10,000
patient-years) - Avoid if significant hepatic/renal impairment
- THIAZOLIDINEDIONES (-glitazones)
- Effective in various insulin-resistant states
- Do not cause hypoglycaemia
- Fall in INS and lipid levels 2ary to fall in BG?
- Does not affect INS function in normal tissues
- Act as ligands for PPARG (Peroxisome-Proliferator
-Activated Receptor Gamma) - PPARs are members of nuclear hormone receptor
superfamily - Form heterodimers with retinoid X to regulate
gene transcription
8
Treatment Goals
- The goal is to correct the metabolic
complications of insulin deficiency - ACUTE hyperglycaemia (causing polyuria/thirst)
- ketoacidosis
- macro vascular atherosclerotic e.g.
stroke/AMI - CHRONIC
- micro vascular nephropathy
- retinopathy
- neuropathy
- NB Progression of CHRONIC complications are
directly related - to the degree of hyperglycaemia - long-term
efficacy of tight glycaemic - control demonstrated by UKPDS (type 2) and DCCT
(type 1) trials.
9
Major Therapeutic Trials 1
- DCCT (Diabetes Control Complications Trial)
1983-1993 - 1441 Type 1 patients (726 no retinopathy or
microalbuminuria 715 non-prolif retinopathy and
microalbuminuria) - Randomised to INTENSE or CONVENTIONAL Rx
- Average follow-up 6.5 years
- INTENSE Rx reduced by approx 60 the risk of
retinopathy, nephropathy and neuropathy. - 3-fold increase in risk of severe hypo in INTENSE
group. - INTENSE tds INS or pump frequently adjusted
by at least qds BG - CONVENTIONAL od/bd INS and single daily BG or
urine check
10
Major Therapeutic Trials 2
- UKPDS (UK Prospective Diabetes Study) 1977-1997
- 5102 newly diagnosed Type 2 patients from 23
centres - Median follow up of 11 years
- Randomised to diet or Rx (INS, SU or MF)
- All Rx showed similar efficacy over diet
- Good glycaemic reduced risk of microvasculopathy
- Approx 35 reduction for each 1 fall in HbA1c
- Macrovascular disease risk not affected
- ? function deteriorated steadily during the study
regardless of Rx - Only reduced by anti-hypertensive Rx in a sub
study where the impact of aggressive BP control
mirrored HOT trial.
11
Control Targets in Diabetes
- Tight glycaemic control should be the goal
whenever possible - e.g. ADA targets HbA1c lt7 and fasting BG
4.4-6.7 mmol/l - Are there risks of tight glycaemic control ?
- elderly AMI, stroke, syncope
- YES (hypoglycaemia)
- young (lt7) impaired brain development ?
- What about other cardiovascular risk factors ?
- Cardiovascular risk factors act synergistically ?
- Tight control of BP (lt140/85) and cholesterol (TC
lt5) - Stop smoking
- Aspirin for high-risk patients?
12
BP control in Diabetics BHS guidelines
- Type I
- prevalence of HT similar to non-DM until
nephropathy develops (microalbuminuria or
proteinuria) - ACE-inhibitors 1st-line antihypertensives reduce
rate of decline renal function and progression
microalbuminuria ? proteinuria - Target BP lt140/80 (lt125/75 if proteinuria
present) - ACE-I useful in normotensives?
- Type 2
- High prevalence (gt70 have BP gt140/90)
- No antihypertensive class favoured gt2 agents
often needed to reach target of 140/80
13
Newer drug developments
- True monomer INS
- Lispro (LysB28-ProB29)
- Aspart (AspB28)
- Very long-acting BASAL INS
- HOE 901 (GlyA21, di-arginyl B30)
- New INS Delivery Routes ?
- Nasal
- Oral
- Rapid-acting Insulin secretogogues e.g. non-SU
Repaglitine - (only close KATP channels in the presence of
glucose) - Modifiers of Post-Prandial Hyperglycaemia (PPHG)
- Agents to delay gastric emptying amylin
derivatives
14
Further Information
American Diabetic Association (ADA) web site
http//www.diabetes.org/ Diabetes branch of
NIDDK http//www.niddk.nih.gov/ BHS guidelines
http//www.hyp.ac.uk/bhs PPT Slide show
at http//www-clinpharm.medschl.cam.ac.uk