Case Presentation - PowerPoint PPT Presentation
1 / 39
Title:
Case Presentation
Description:
Case Presentation ... Treated initially at that time with prednisone ... sagittal sinus in particular. Abdominal veins. Dermal veins. Pulmonary embolism unusual ... – PowerPoint PPT presentation
Number of Views:76
Avg rating:3.0/5.0
Title: Case Presentation
1
Case Presentation
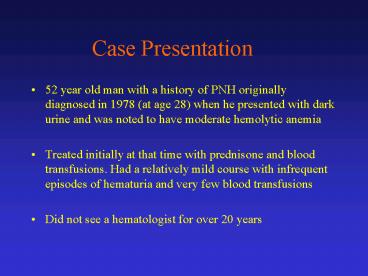
- 52 year old man with a history of PNH originally
diagnosed in 1978 (at age 28) when he presented
with dark urine and was noted to have moderate
hemolytic anemia - Treated initially at that time with prednisone
and blood transfusions. Had a relatively mild
course with infrequent episodes of hematuria and
very few blood transfusions - Did not see a hematologist for over 20 years
2
Case Presentation
- Presented in April 2002 with abdominal pain and
distension and was noted to be jaundiced - Hepatitis workup was negative but an MRI of the
abdomen revealed hepatic vein thrombosis
(Budd-Chiari syndrome) - Underwent a transjugular liver biopsy on 4/23/02
which revealed extensive fibrosis, no cirrhosis,
sinusoidal dilatation and central vein fibrosis
consistent with Budd-Chiari syndrome - Despite anticoagulation and numerous
paracenteses, refractory ascites was present and
he underwent a TIPS procedure in 7/02
3
Case Presentation
- Patient subsequently developed hepatic
encephalopathy, requiring multiple hospital
admissions over 2 months following TIPS placement - Ultrasounds confirmed patency of shunt
- Referred to Dr Bessler in 9/02. Evaluation
revealed a jaundiced, mildly encephalopathic man
with normal abdomen - CBC revealed Hgb 11.9 with MCV 97.2, plt cnt
90,000, ANC 2,700, INR 1.7, creatinine 0.8, and
bilirubin 6
4
Case Presentation
- Flow Cytometry
- erthrocytes 17 CD59 deficient
- granulocytes 99.8 CD59/CD24 deficient
- monocytes 82 CD59 deficient
- lymphocytes 24 CD59 deficient
- Anticoagulation increased, folic acid started,
and referred for consideration of hematopoietic
stem cell transplantation
5
Paroxysmal Nocturnal Hemoglobinuria
- PNH is an acquired disorder of hematopoiesis
characterized by intravascular hemolysis and
manifested by episodes of hemoglobinuria and
life-threatening venous thromboses - Caused by a somatic mutation in PIG-A gene of a
hematopoietic stem cell - Cells derived from the abnormal clone are
deficient in all surface proteins normally
attached to the cell membrane by a
glycoslphoshpatidylinositol (GPI) anchor
6
Paroxysmal Nocturnal Hemoglobinuria
- First described as a clinical entity in 1882
- Cardinal diagnostic test, introduced in late
1930s by Ham, is based on the increased
sensitivity of PNH erythrocytes to lysis via
complement - Deficiency of a surface antigen acting as a
complement defense protein (CD59), is largely
responsible for the hemolysis and implicated in
the thrombotic tendency
7
GPI Linked Proteins
Rosti, Haematologica, 2000
8
GPI anchored Proteins
Johnson and Hillmen,Mol Pathol, 2002
9
PNH Defect
Hillmen and Richards, Br J Haematol, 2000
10
Diagnostic Tests
- Acid hemolysis (Ham test) specific but not very
sensitive - Flow cytometry
- evaluate for presence/absence of GPI-linked
proteins on hematopoietic cells - CD55 and CD59
11
Flow Cytometric Analysis
Hillmen et al, NEJM, 1995
12
Clinical manifestations of PNH
- Highly variable and dependent upon the size of
the abnormal clonal population in any individual - Hemolysis
- mild to very brisk
- dependent upon
- size of abnormal clone (1-gt90)
- content of complement defense proteins
(PNHII/III) - presence of concomitant infection or other factor
activating complement
13
Clinical manifestations of PNH
- Thrombosis
- Hepatic vein most common
- common cause of fatality
- Cerebral vein thrombosis
- sagittal sinus in particular
- Abdominal veins
- Dermal veins
- Pulmonary embolism unusual
14
Clinical manifestations of PNH
- Relative/absolute bone marrow failure
- present to some degree in all patients
- relative granulocytopenia/thrombocytopenia
- decreased capacity to form myeloid colonies
- Two stage model
- somatic mutation in PIG-A gene
- some cause for bone marrow failure
- Is damage directed at a GPI linked molecule?
15
Dual Pathogenesis Hypothesis
Hillmen and Richards, Br J Haematol, 2000
16
Natural History of PNH
Hillmen et al, NEJM, 1995
- Long term study of 80 patients with PNH seen at
one institution between 1940 and 1970 - Results
- median age at diagnosis 42 (16-75)
- median survival 10 years
- 28 survived more than 25 years
- 39 had one or more episodes of venous thrombosis
- 12 experienced spontaneous clinical recovery
- leukemia did not develop in any of the patients
17
Sites of Thrombosis in PNH
Hillmen et al, NEJM, 1995
18
Natural History of PNH
Hillmen et al, NEJM, 1995
19
Natural History of PNH
Hillmen et al, NEJM, 1995
20
Treatment
- Supportive, prevent complement activation
- prednisone
- Therapy for/prevention of thrombosis
- thrombolytics acutely
- anticoagulation
- Stimulate hematopoiesis
- G-CSF
- Immunosuppression
- ATG
- Cyclosporine
21
Treatment
- Stem Cell Transplantation
- syngeneic
- autologous
- Allogeneic
- related
- unrelated
- Ablative
- Non-myeloablative
- Gene Therapy?
22
Circulating Stem Cells in PNH
Johnson et al, Blood, 1998
23
Stem Cell Transplantation in PNH
- Summary of single institution trials
- Approximately 12 reported
- Number of patients ranges from 1-16
- Survival rates typically higher (58-100)
- Likely high degree of reporting bias, based on
outcomes seen using registry data
24
Stem Cell Transplantation in PNH
IBMTR Data Saso et al, Br J Haematol, 1999
25
Results
- Sustained engraftment 77
- Graft failure 17
- Grade 2-4 acute GVHD 34
- Chronic GVHD 33
- Causes of death
- graft failure (7), int. pneumonitis (4), GVHD
(3), infection (3), ARDS (2), hemorrhage (1)
IBMTR Data Saso et al, Br J Haematol, 1999
26
Stem Cell Transplantation in PNH
Matched siblings
IBMTR Data Saso et al, Br J Haematol, 1999
27
Stem Cell Transplantation in PNH
Matched siblings
IBMTR Data Saso et al, Br J Haematol, 1999
28
Stem Cell Transplantation in PNH
- EBMT Database (unpublished)
- 46 transplants using HLA-ID sibs reported from
1979 to 1997 - Median age at diagnosis 29 (10-46)
- Median interval from diagnosis to BMT 794 days
(30-8680) - Actuarial 5 yr survival 52
- Main cause of death acute GVHD
29
Stem Cell Transplantation in PNH
Patient Characteristics
Transplant Outcomes
Raiola et al, Haematologica, 2001
30
Stem Cell Transplantation in PNH
Raiola et al, Haematologica, 2001
31
Stem Cell Transplantation in PNH
Flotho et al, Br J Haematol, 2002
32
Stem Cell Transplantation in PNH
- Conclusions from reported series
- BMT may cure 50-60 of selected patients with
HLA-identical siblings - Most patients transplanted have been lt 30 years
of age - Regimen related toxicity and GVHD remain
significant hurdles - Role of alternative donor transplants unclear,
though initial reports are not encouraging except
in pediatric population
33
Stem Cell Transplantation in PNH
- Open questions
- What degree of conditioning is necessary to fully
eradicate PNH clone? - Is immunosuppression sufficient?
- What is the role of non-myeloablative
conditioning? - What is the role of T-cell depletion?
- What if patient has advanced PNH but lacks an
HLA-identical sibling donor?
34
Non-myeloablative Transplantation in PNH
- Rationale
- Decrease toxicity and potentially lower risk of
GVHD associated with standard regimens - Provide immunosuppression sufficient for
engraftment of donor hematopoietic cells and
potentially for eradication of PNH clone via
cytotoxic T-cells - Allow transplantation in patients with more
advanced PNH - Case report from Japan demonstrated feasibility
- Suenaga et al, Exp Hematol, 2001
35
Low Intensity Conditioning
- Low dose TBI/CSA/MMF
- Flu/Cy
- Flu/Bu/ATG
- Cy/Low dose TBI
- Flu/Melphalan
36
Non-Ablative Stem Cell Transplantation
Barrett and Childs, Br J Haematol, 2000
37
Non-myeloablative Transplantation in PNH
Takahashi et al, ASH, 2002
- Transplanted 5 patients with hemolytic PNH and
RBC transfusion dependence - Less toxic fludarabine (125mg/m2) and
cyclophosphamide (120mg/kg) conditioning regimen
used - GPI-negative neutrophils eradicated in all 5 by
day 115 - Demonstrated generation of miHa specific CTL
capable of lysing both GPI-negative and positive
B-cells no eveidence of decreased sensitivity to
T-cell mediated lysis in PNH cells could be
identified - All 5 survive without PNH from 5-39 months post
transplant
38
Prognosis Based on Management
Luzzatto, Haematologica, 2001
39
PNH Management Guidelines
Luzzato, ASH, 2001