Obstetric Emergencies - PowerPoint PPT Presentation
Title:
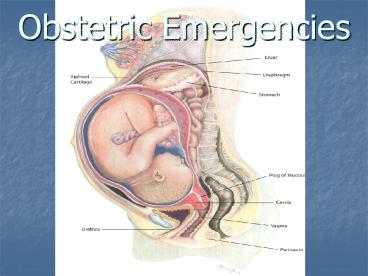
Obstetric Emergencies
Description:
Obstetric Emergencies * * * * * * * * * * * * Complications of Pregnancy: Eclampsia Preeclampsia +seizures or coma May occur without proteinuria, may occur up to 10 ... – PowerPoint PPT presentation
Number of Views:4345
Avg rating:3.0/5.0
Title: Obstetric Emergencies
1
Obstetric Emergencies
2
Obstetric Emergencies We will cover...
- Normal Pregnancy
- Common medical and surgical complications of
pregnancy
3
Normal pregnancy
- All females of childbearing age are presumed to
be pregnant until proven otherwise. - All pregnancy tests detect B-HCG which is
produced at the time of implantation (8-9 days
post conception) - B-HCG should double every day for the first
weeks, peak at week 8 and remain elevated up to
60 days post-partum
4
- False Negatives
- Too early in pregnancy
- Dilute/old urine
- Ectopic
- Incomplete Ab.
- False Positives
- Urine hematuria/proteinuria
- Serum
- T.O.A.
- Thyrotoxicosis
- Molar pregnancy
- Drugs (MJ, ASA, Phenothiazines, anticonvulsants,
antidepressants, methadone
5
Some Important Physiological Changes in Pregnancy
- Cardiac increased heart rate, decreased blood
pressure. CO increases - Respiratory rate increases, TV increases, FRV
decreases, pCO2 decreases - Heme Volume increases, HCT drops, WBC increases
6
Drugs in Pregnancy A, B, C, D, X
- Considered Safe in pregnancy
- PCN
- Cephalosporins
- Azithro/Erythromycin
- Acetaminophen
- Narcotics
- Heparin
- Asthma Drugs
- Reglan (Metoclopramide)
- Immunizations derived from killed viruses
(tetanus, diptheria, Hep. B, Rabies)
7
Radiation in Pregnancy
- lt5-10 rads no significant risk of birth defects
- Beams aimed 10cm away from fetus pose no
additional risk - Initial trauma X-rays each deliver lt1 rad
- One never withholds necessary radiography.
- Use MRI or U/S if available.
8
Transvaginal Ultrasound Images
9
Normal, non-pregnant uterus on T/V U/S
10
The Double-Ring Sign or Double Decidual Sign
of normal early pregnancy
11
Normal Pregnancy T/V Ultrasound Showing
Gestational and Yolk Sac. No fetus is seen. 5w
2d
12
6w 1d T/V U/S showing yolk sac
13
Normal T/V U/S with embryo at 10w 3d
14
Complications of Pregnancy Vaginal Bleeding
- 1st Trimester Causes
- Ectopic
- Abortion
- Molar Pregnancy
- Non-pregnancy Related
- a. Infectious
- b. Trauma
- c. Neoplasm
15
The work-up is the same!
- Pelvic Exam
- Beta HCG
- Transvaginal ultrasound
- Rh
- CBC, CMP
- PT/PTT/INR
- UA
16
(No Transcript)
17
Ectopic Pregnancy A surgical emergency of
pregnancy
- The leading cause of first trimester maternal
death - Usually 5-8 weeks after LMP
- High Risk History of ectopic, tubal surgery or
sterilization procedure, Known tubal scarring or
pathology, Diethylstilbestrol exposure, IUD.
18
Signs/Symptoms
- Symptoms (in decreasing order of frequency)
Abdominal pain, amenorrhea, vaginal bleeding
(50-80), dizziness, pregnancy symptoms, urge to
defecate, passing tissue - Signs Adnexal tenderness, abdominal tenderness,
adnexal mass, enlarged uterus, orthostatic
changes, fever
19
Testing
- Beta gt 6000 mIU/ml empty uterus on
transabdominal ultrasound - OR
- Beta gt 1200 mIU/ml empty uterus on transvaginal
ultrasound - Ectopic Pregnancy Laparoscopy
20
- Beta lt6000 empty uterus on transabdominal
ultrasound - OR
- Beta lt 1200 empty uterus on transvaginal
ultrasound serial outpatient beta measurements
to ensure normal rise. - This only applies to stable patients and should
be done in consult with ob/gyn
21
A heterotopic pregnancy (to compare normal vs.
abnormal)
22
Ectopic Pregnancy
23
2nd Trimester
- Causes are abortion and non-pregnancy causes.
- Work-up is the same
- Management of threatened AB is the same
- If complete, may be DC candidate
- If other types of AB, patient may undergo
oxytocin induced labor as inpatient.
24
3rd Trimester (gt28 weeks)
- Placental Abruption
- Placenta separates from uterine wall
- Painful dark or clotted blood
- Risks HTN, smoking, ETOH, cocaine, multiparity,
previous abruption, trauma, mom gt 40 - Management U/S, Ob consult, cardiac/fetal
monitoring, IV, pre-op labs, delivery if possible
- Placenta Previa
- Placenta implants too low
- Painless bright red bleeding
- Risks prior C-section, grand multiparity,
previous previa, multiple gestations, multiple
induced abortions, mom gt40. - Management U/S, Ob consult, pre-op labs, avoid
pelvic exam, c-section
25
3rd Trimester Bleeding contd
- Uterine Rupture Can be seen in scarred and
unscarred uteri. (uteruses? uterata?)
26
(No Transcript)
27
(No Transcript)
28
Complications of Pregnancy Trauma
- Key Concept Although you have two patients,
maternal circulation is to be maintained at the
expense of the fetus. Without mom, the baby will
surely die. - Mom should be kept in left lateral decubitus
- This is where knowing the physiologic changes of
pregnancy becomes extremely important ! Mom can
lose up to 35 of her blood volume before showing
any signs of shock!
29
Management
- Over 20 weeks Goes to Ob for 4 hours of
cardiotocographic monitoring - All women with abdominal trauma get Rhogam
(fetomaternal hemorrhage present in 30 of these
patients) - Kleihauer-Betke test Used in women gt12w to
determine and quantify the amount of fetomaternal
hemorrhage that occurred
30
Perimortem C-Section
- Fetus greater than 28weeks, maternal death less
than 15 minutes perimortem c-section
31
Complications of Pregnancy Hypertension
- Can be chronic (meaning it began prior to
conception or began during gestation and persists
gt6 weeks post-partum) or gestational. - We care about this because HTN in pregnancy is
associated with pre-eclampsia, abruption,
prematurity, IUGR and stillbirth
32
Pre-eclampsia To be considered in those gt20wks
with HTN
- Mild
- SBP gt 140 (or 20 from baseline. Or DBP gt90 (or
10 from baseline) - Proteinuria .3g/24h
- /- Edema
- No Oliguria
- No Associated symptoms
- Normal labs
- No IUGR
- Severe
- BPgt160/90
- Proteinuria gt5g/24h
- Edema Present
- Oliguric
- Associated symptoms (H/A, visual symptoms,
abdominal pain, pulm. edema - Associated labs (dec. plts, inc. LFT, inc. bili,
inc. creatinine, increased uric acid) - IUGR present
- HELLP syndrome very severe. Above RUQ pain,
n/v
33
Management
- Isolated HTN requires a 24h urine and close Ob
f/u - With other findings, admit, 24h urine, bed rest
and HTN management in consult with ob/gyn. - Hydralazine common though diazoxide, labetalol,
nifedipine and nitroprusside also used - /- Mag to prevent seizures
34
Complications of Pregnancy Eclampsia
- Preeclampsia seizures or coma
- May occur without proteinuria, may occur up to 10
days postpartum - ICH is the major cause of maternal death
- Warning signs H/A, visual changes,
hyperreflexia, Abd. pain - Tx Delivery. Magnesium, Phenytoin or Diazepam,
Hydralazine or Labetalol
35
Complications of Pregnancy UTI/Pyelo
- Pregnant women more prone to UTI secondary to
physiologic changes of pregnancy - Treat both symptomatic and asymptomatic bacturia
(untreated up to 40 risk of progression to
pyelo) - Culture urine, give 7 day course
- We admit pregnant women with pyelonephritis
because of its increased risk of of progressing
to preterm labor or septic shock.
36
Complications of Pregnancy Appendicitis
- Appendicitis is the most frequent surgical
emergency of pregnancy - Incidence is the same as non-pregnant population
but the complications are more frequent secondary
to delayed diagnosis - Again, the physiologic changes of pregnancy
complicate the clinical picture (leukocytosis,
displaced appendix) - Picture mimics pyelo. When patients dont
improve with IV abx, the diagnosis is
reconsidered. - Laparotomy is the preferred diagnostic procedure.
Ultrasound can used
37
(No Transcript)
38
References
- 1. Preparing for the Written Board Exam in
Emergency Medicine. 5th ed. Vol 1. Rivers,
Carol. pp 550-574 - 2. learnobultrasound.com/3trimesterbleed.htm
- 3. www.smbs.buffalo.edu/emed/emed/ultrasound.html
- 4. Harwood Nuss Clinical Practice of Emergency
Medicine 4th ed. Wolfson, Alan B Lippincott,
Williams and Wilkins, Philadelphia, 2005.
pp.496-497 - 5. home.flash.net/drrad/tf/122396.htm
- 6. www.pwc-sii.com/Research/death/ribs.htm
- 7. www.jaapa.com/.../article/130146/
- 8. www.advancedfertility.com/ultraso1.htm
- 9. Ma, John O. Emergency Ultrasound via access
emergency medicine at http//0-www.accessem.com.i
nnopac.lsuhsc.edu/content.aspx?aID100900