Immunodeficiencies - PowerPoint PPT Presentation
1 / 55
Title: Immunodeficiencies
1
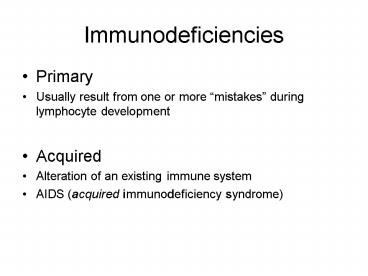
Immunodeficiencies
- Primary
- Usually result from one or more mistakes during
lymphocyte development - Acquired
- Alteration of an existing immune system
- AIDS (acquired immunodeficiency syndrome)
2
Cancers during stages of lymphocyte development
3
Lymphocyte Development
- Where can things go wrong?
- Stem cell replication and differentiation
4
(No Transcript)
5
Lymphocyte Development
- Where can things go wrong?
- Stem cell replication and differentiation
- B-lymphocyte differentiation
6
Somatic recombinationsCell replications
7
(No Transcript)
8
Lymphocyte Development
- Where can things go wrong?
- Stem cell replication and differentiation
- B-lymphocyte differentiation
- T-lymphocyte differentiation
9
- Somatic Recombinations
- Cell replications
10
Positive Selection
11
X-linked agammaglobulenemia
- Sex-linked (X chromosome)
- Inherited (primary) immunodeficiency
- Btk (Brutons tyrosine kinase) deficiency
12
(No Transcript)
13
X-linked agammaglobulenemia
- Sex-linked (X chromosome)
- Inherited immunodeficiency
- Btk (Brutons tyrosine kinase) deficiency
- Reaches pre-B cell receptor stage
14
(No Transcript)
15
Severe Combined Immunodeficiencies
- Will affect BOTH B-cell and T-cell responses
- Dysfunctional RAG genes
16
(No Transcript)
17
Severe Combined Immunodeficiencies
- Will affect BOTH B-cell and T-cell responses
- Dysfunctional RAG genes
- Somatic recombination events never get started
- Essentially NO functional B or T cells
- Adenosine deaminase deficiency
- ADA enzyme NOT produced
- Toxic by-products not broken down
- T-cells are most affected
- T-helper cell deficiency also affects B-cell
responses
18
ADA deficiency gene therapy
- Functional ADA gene inserted into lymphocytes
using a virus vector - Early results were promising
- ADA produced
- T-lymphocyte population increased
- Immune responses started
- Long-term prognosis is NOT good (yet)
19
Bare lymphocyte syndrome
- Dysfunctional MHC Class II peptide presentation
- No T-helper cell development
20
Positive Selection
21
Bare lymphocyte syndrome
- Dysfunctional MHC Class II peptide presentation
- No T-helper cell development
- No T-helper cell mediated responses
22
(No Transcript)
23
Bare lymphocyte syndrome
- Dysfunctional MHC Class II peptide presentation
- Dysfunctional TAP
24
(No Transcript)
25
Bare lymphocyte syndrome
- Dysfunctional MHC Class II peptide presentation
- Dysfunctional TAP
- No initiation of T-cytotoxic cell responses
26
Acquired Immunodeficiency Syndrome (AIDS)
- Caused by a virus (human immunodeficiency virus
HIV)
27
Acquired Immunodeficiency Syndrome (AIDS)
- Caused by a virus (human immunodeficiency virus
HIV) - HIV preferentially infects T-helper cells
- HIV Attaches to CD4 and to CCR5 (a chemokine
receptor)
28
- GP120 binds to CD4, then to CCR5
29
Complete HIV infection cycle
30
The results
- Infected T-helper cell is destroyed
- Released HIV then infect other T-helper cells
31
The results
- Infected T-helper cell is destroyed
- T-helper cell sends a kill me signal using MHC
Class I presented HIV peptides - T-cytotoxic cells destroy virus-infected T-helper
cells
32
Chronic depletion of CD4 T-helper cells
33
What to do about HIV/AIDS?
- Use drugs that interfere with one or more of the
stages of HIV infection, replication, release.
34
Use the immune system
- Antibodies to prevent HIV attachment
35
Use the immune system
- Antibodies to prevent HIV attachment
- Specific for gp120 (or some portion)
36
Use the immune system
- Antibodies to prevent HIV attachment
- T-cytotoxic cell destruction of HIV-infected
cells before viral replication and release
37
Use the immune system
- Expand HIV-peptide specific T-cytotoxic cell
population before HIV infection - MHC Class I presentation of HIV-peptide by
non-infected cells without causing any harm - Hey, what about using the dendritic cell to
present the HIV peptides? - Would prime AND expand the T-cytotoxic cell
population - DCs can also do cross-presentation
- What form of the vaccine material will be
correctly processed and presented by the DC
gp120?, other viral peptide? - How about genetically manipulating the DC to
express MHC Class I HIV peptides? insert HIV
nucleotide sequence and necessary enzymes
38
A solution for primary immunodeficiencies?
- Bone Marrow Transplant
- Why?
- Bone marrow is essentially a complete immune
system
39
(No Transcript)
40
A solution?
- Bone Marrow Transplant
- Why?
- Bone marrow is essentially a complete immune
system - Including fully mature B-cells and T-cells
41
Uses of Bone Marrow Transplants
- Bone Marrow transplants used to replace
non-existent, destroyed or non-functioning immune
system - Immunodeficiency diseases
- No immune system
- Cancers (when irradiation and chemotherapy are
used to kill cancer cells) - Immune system cells are very sensitive to these
treatments (destroys immune system)
42
Bone Marrow transplants
- Outcome is defined by MHC compatability
- IF there are any differences between MHCs in
donor and recipient - Recipient will treat foreign MHCs as non-self
antigens - Donor BM cells will be destroyed (rejected)
43
(No Transcript)
44
Bone Marrow transplants
- Outcome is defined by MHC compatability
- IF there are any differences between MHCs in
donor and recipient - Recipient will treat foreign MHCs as non-self
antigens - Donor BM cells will be destroyed (rejected)
- Result is no effective replacement of immune
system
45
Bone Marrow transplants
- IF there are any differences between MHCs in
donor and recipient AND the recipients immune
system has been destroyed - Donor lymphocytes will consider the foreign
MHCs in the recipient as non-self and will begin
to destroy entire recipient called a
Graft-vs-Host response
46
(No Transcript)
47
Bone Marrow transplants
- Ideal condition NO differences between MHCs in
donor and recipient - How might that condition be obtained?
- Autologous BM transplant
- Donor and recipient are the same person
- Only if cancer is not in the bone marrow
48
Bone Marrow transplants
- Ideal condition NO differences between MHCs in
donor and recipient - How might that condition be obtained?
- Autologous BM transplant
- Syngeneic BM transplant
- Identical twin
- Sibling (25 chance of matching MHCs)
49
(No Transcript)
50
Bone Marrow transplants
- Ideal condition NO differences between MHCs in
donor and recipient - How might that condition be obtained?
- Autologous BM transplant
- Syngeneic BM transplant
- Allogeneic BM transplant
- Donor recipient are NOT matched
51
(No Transcript)
52
Bone Marrow transplants
- Ideal condition NO differences between MHCs in
donor and recipient - How might that condition be obtained?
- Autologous BM transplant
- Syngeneic BM transplant
- Allogeneic BM transplant
- Donor recipient are NOT matched
- Immunosuppressive drugs
- Recipient very susceptible to infections, cancers
- Graft-vs-host response may occur
53
Allogeneic BM transplant - what to do?
- Try to find the perfect MHC match
- Chances are 1 in 20,000 (or higher)
- Community bone marrow drives
- Chance of finding the perfect match is slim
- Number of persons participating is too low
54
Solution
- Expand the number of potential donors
- National Marrow Donor Program
- Volunteer to have your tissue typed
- Determines your set of MHCs
- Worldwide data bank of tissue types
- Can be searched for a compatible donor
- Donor contacted to see if willing to donate
- Outcome can be lifesaving
55
Drive for Diversity
RITs Physician Assistant Class of 2011
- Wednesday, November 5
- 10 am 2 pm
- Clark Gym
2nd annual Marrow Registry Drive in honor of
Nicole Nelson, a PA from New Hampshire whose
Native American background made finding a match
very difficult. (A match was eventually made
with two donor cords from Australia!) Although
there are 7 million donors on the registry, each
day 6,000 people are still actively seeking a
match. Diversity is the most important measure
of a successful registry.
Saving a life is a 30 second mouth swab away
For more information, please visit
http//www.marrow.org/DONOR/When_You_re_Asked_to_D
onate_fo/Donation_FAQs/index.html or e-mail us
at ritmarrowdrive_at_yahoo.com