AcidBase - PowerPoint PPT Presentation
1 / 37
Title: AcidBase
1
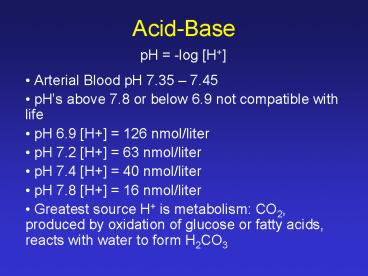
Acid-Base
pH -log H
- Arterial Blood pH 7.35 7.45
- pHs above 7.8 or below 6.9 not compatible with
life - pH 6.9 H 126 nmol/liter
- pH 7.2 H 63 nmol/liter
- pH 7.4 H 40 nmol/liter
- pH 7.8 H 16 nmol/liter
- Greatest source H is metabolism CO2, produced
by oxidation of glucose or fatty acids, reacts
with water to form H2CO3
2
- H2CO3 is a volatile acid
- Large amounts removed at the lungs (15,000-25,000
mmol CO2/day) - Fixed acids only represent 0.2 of the bodies
acid production, removal mainly by kidneys, some
by the GI tract. - Bicarbonate system able to buffer the fixed acids
because the CO2 can be removed at the lungs
3
Respiratory Acidosis
- Alteration of alveolar ventilation that results
in an increase in Pco2 (gt 45 mm Hg in alveoli)
and hence also arterial Pco2, decreases the
arterial pH and results in respiratory acidosis. - Ratio of HCO3-/CO2 is decreased
4
Respiratory Alkalosis
- Excess ventilation, Pco2 in alveoli lt 35 mm Hg
- Get increase in pH
- Ratio of HCO3-/CO2 is increased
5
Regulation of Respiration
- The system works to maintain steady levels of O2
and CO2 in the arterial blood. - The respiratory center is located in the pons and
the medulla oblongata.
Pons
4th Ventricle
Medulla Oblongata
CSF
6
Dorsal respiratory group
Pneumotaxic center
Dorsal respiratory group
Apneustic center
Ventral respiratory group
Phrenic nerve
Vagus Glossopharyngeal
- 3 major collections of neurons located
bilaterally - dorsal respiratory group
- ventral respiratory group
- pneumotaxic center
7
Dorsal Respiratory Group
- In the dorsal part of the medulla
- Special neuronal cells discharge spontaneously
and rhythmically resulting in inspiration. Like
a pacemaker. - Impulses travel the phrenic nerve to the
diaphragm and cause it to contract. - Located in the nucleus of tractus solitarius,
this is the end point of the vagus and
glossopharyngeal nerves.
8
Breathing
Strength Inspiratory Signal
IN
OUT
Time
- Signal begins weakly and increases steadily for
2 seconds. - Stops abruptly for 3 seconds. Stops diaphragm
from contracting and elastic recoil of lung
causes expiration. - Results in a steady increase of lung volume
9
Pneumotaxic Center
- Located in the upper pons
- Works in conjunction with the Apneustic Center
in the lower pons to SWITCH OFF the inspiratory
signal. - If signals are strong the inspiratory ramp signal
will be short. Breathing rate will - Function is to limit inspiration.
10
Ventral Respiratory Group
- Inactive during normal breathing
- When increased pulmonary ventilation is required,
signals from the dorsal respiratory group are
sent to the ventral group. - Signals are then sent to all the muscles of
respiration during the cycle of breathing. - Especially the abdominal muscles for expiration
- Main use Increases inspiration and expiration,
allowing exchange of large volumes of air.
11
Chemical Control of Ventilation
- AIM To maintain a fairly constant level of O2,
CO2 and H in the body fluids. - Direct control, central chemoreceptors CO2 and
H - Stimulates inspiration
- Indirect control through peripheral
chemoreceptors - Low O2, signal to stimulate respiration
- High CO2 or H stimulates respiration, small
compared to direct effect
12
Direct Control by CO2 and H at the central
chemoreceptors
- Chemosensitive area of neurons, 0.2mm below
surface of medulla. - Very sensitive to changes in H in the CSF and
interstitial fluid and CO2 in blood. - CO2 can cross from blood to the CSF. H cannot.
BUT CO2 reacts and produces H in the CSF.
CSF
Chemo- sensitive area
Dorsal R.G.
H HCO3-
H2CO3
CO2 H2O
13
Central chemoreceptors area
- Chemosensitive area responds to changes in the
CSF and the interstitial fluid of the medulla - High PCO2 in blood CO2 diffuses to CSF and
medulla. H are blocked by blood-brain and
blood-CSF barrier. - CO2 reacts with water to form carbonic acid,
which breaks down to form H and HCO3- - Not enough protein in CSF to buffer the H
- Chemosensitive area sends signals to DRG,
respiration increases.
14
Effect of Blood CO2 on basal respiration
- PCO2 has a greater effect on respiration
- Normal blood PCO2 range is 35-60 mmHg. This is
the range at which ventilation rate is most
sensitive to change.
15
Adaptation of central chemoreceptors
- CSF pH 7.32
- Not as much buffering as blood so can have rapid
change of pH. - If pH is low for a long period of time, HCO3- is
transported across the blood-brain barrier. This
will then prevent high stimulation of the
respiration system over a long period of time. - HCO3- is renal compensation, more effective in
the CSF than in the blood, as CSF buffering
lower.
16
Reflex mechanisms of respiratory control
- Pulmonary stretch receptors
- Receptors in the airways and lung
- Pulmonary vascular receptors (J receptors)
- The cardiovascular system (peripheral
chemoreceptors) - Muscles and tendons
17
Pulmonary stretch receptors
- Hering-Breuer inflation reflex
- Stretch receptors situated in the smooth muscle
of the large and small airways - Called slow adapting pulmonary stretch receptors
as activity maintained with sustained stretch - Discharge when lung is distended, travels via the
vagus nerve - Slows respiratory frequency by increasing the
time of expiration - Not initiate until 800-1000ml tidal volume
- Abrupt deflation, leads to an increase in
respiration frequency, maybe stretch receptors as
well as irritant and J receptors.
18
Receptors in the airways and lungs
- Irritant receptors
- Mechanical or chemical irritation of the airways
results in a reflex cough or sneeze,
bronchoconstriction. - Located in the nasal mucosa, upper airways,
tracheobronchial tree and possibly the alveoli. - Those in larger airways respond to stretch also,
but rapidly adapt and activity decreases rapidly
during a sustained stimulus - Except for those in the nasal mucosa, signals
sent via the vagus - Maybe involved in bronchoconstriction in asthma
- Immersion of face in water, results in apnea,
bronchoconstriction, laryngeal constriction,
response of receptors in the nose to water.
19
Reflexes from Pulmonary vascular receptors
- J receptors
- are believed to be in the walls close to the
capillaries (juxta-capillary) - Respond quickly to chemicals in the pulmonary
circulation - Impulses pass up the vagus in slowly conducting
nonmyelinated fibers - Result in rapid, shallow breathing
- Intense stimulation causes apnea
- Increased stimulation caused by pulmonary
vascular congestion (rapid breathing) - Decreased stimulation by decreased flow through
capillaries (decreased ventilation)
20
- Bronchial C-fibers
- Respond quickly to chemicals in the bronchial
circulation - Response to stimulation includes rapid shallow
breathing, bronchoconstriction and mucous
secretion
21
Reflexes from the Cardiovascular system
- Arterial Chemoreceptors
- Largest number are in the carotid bodies
- Also in aortic bodies.
- Special blood supply feeds the bodies. Very high
blood flow through the bodies results in little
alteration of PO2 compared to the artery.
(Hering)
22
Carotid body nerve impulses / second
Arterial PO2 (mm Hg)
- Arterial PO2 low, chemoreceptors send signals to
dorsal respiratory group. - Aortic bodies via the vagus nerve
- Carotid bodies via the glossopharyngeal nerve
- Impulse rate sensitive at PO2 60-30 mm Hg which
is where O2-Hemoglobin dissociates most rapidly.
23
- High CO2 and H also stimulates the
chemoreceptors (7 x less effective than by
direct effect on central chemosensitive area).
Receptors in the carotid respond to pH in humans. - If air has low O2, blood PO2 is low,
chemoreceptors fire to respiration. But
respiration blows off CO2 so blood PCO2 and
H. The respiration rate does not increase
greatly. - Effect of low PO2 can be great if CO2 and H is
not decreased by respiration or breathing low
O2 for days allows time for adaptation. - Responsible for increased ventilation in response
to arterial hypoxemia - Rapid response
24
High CO2 and Low O2
- Combined effects is greater than just adding the
response of low O2 and high CO2.
25
- Arterial Baroreceptors
- Stretch receptors that are responsive to changes
in pressure - Situated in carotid sinuses and aortic arch
- Effects of stimulation by elevated blood pressure
are apnea and bronchodilation.
26
Receptors in muscles and tendons
Total ventilation (L/min)
Heavy
Moderate
O2 consumption (L/min)
- Increased metabolism, increased alveolar
ventilation. - But there is negligible change in arterial PO2,
PCO2 and pH - Proprioceptors at the joints of the limbs are
excited during movement and ? pulmonary
ventilation. - Higher centers in the brain that transmit
impulses to contracting muscles are believed to
also transmit signals to the respiratory center
27
Arterial PCO2
Diffusion into CSF and medulla interstitial
Arterial PO2
Arterial pH
pH
Stimulation of chemosensitive area
Firing Carotid Aortic bodies
Stimulation DRG
Stimulation VRG
Higher centers of brain during exercise
Respiration
Proprioceptors during movement
28
Other Factors Affecting Respiration
- Overdose of anesthetics or narcotics
- Certain anesthetics not used now due to
depression of respiratory center - Periodic breathing - short and deep breath, then
not breathe for an interval of time - e.g. Cheyne-Stokes breathing
29
Pulmonary Abnormalities
- Pulmonary emphysema
- Pneumonia
- Atelectasis
- Asthma
- Tuberculosis
- Dyspnea
30
Pulmonary Emphysema
- Excess air in lungs. Usually means obstructive
and destructive process - Disease Chronic infection, excess mucus and
inflammatory edema chronic obstruction of
smaller airways difficult to expire
entraps air in airways overstretching
destruction - Physiological effects
- airway resistance and diffusing capacity
- Lack of capillaries, vascular resistance,
pressure, results in right heart failure. - Death due to hypoxia and high blood CO2.
31
Pneumonia
Emphysema
Normal
Pneumonia
- Inflammatory condition of lung, usually
infection. - Infection in alveoli pulmonary membrane
inflamed and porous cells and fluid move
into alveoli spread of infection
32
Pulmonary artery 60 sat.
Right vein 60 sat.
Left vein 97 sat.
Aorta 1/2 97 1/2 60 Mean 78
- Two major pulmonary abnormalities
- decreased surface area of respiratory membrane.
- No air flow through infected lung.
- Result
- diffusing capacity low PO2 and high PCO2
33
Atelectasis
- Means collapse of alveoli. Occurs by
- Airway obstruction - air entrapped passed
blockage is absorbed by blood and collapses the
alveoli. If lung not pliable then negative
pressure builds in alveoli and sucks fluid in
from the interstitial. Results in edema and
massive collapse. - Lack of surfactant - respiratory distress
syndrome in premature babies. in surfactant
secreted in alveoli, surface tension too high to
be counteracted by the negative pressure of
pleural cavity. Alveoli collapse.
34
Asthma
- Spastic contraction of smooth muscles in the
bronchioles causes diameter of airways. - Mast cells lie in lung interstitium. IgE
antibodies are bound to these cells. Pollen
(antigen for IgE) is breathed in and binds to IgE
antibodies. Results in mast cells degranulating
or bursting.
35
- Histamine and leukotrienes released
Contraction of smooth muscle thick mucus in
bronchiolar lumen edema in walls of small
bronchiolar. - intrapulmonary pressure compresses outside of
bronchioles during expiratory effort. - Result can inspire but hard to expire
36
Tuberculosius
- Tubercle bacilli cause invasion of macrophages
and walling-off lesion by fibrous tissue to form
tubercle. - Walling-off helps prevent spread of infection.
- 3 untreated patients walling-off fails and
destruction of lung and abscess cavities form. - Results in reduced vital capacity, reduced
surface area of respiratory membrane, increased
thickness of respiratory membrane.
37
Dyspnea
- Means mental anguish associated with inability to
ventilate - air hunger - Factors involved
- abnormality of respiratory gases, especially
excess CO2 - amount of work involved to respire
- state of mind
- Emotional dyspnea - respiratory functions normal
but unable to ventilate properly, e.g. fear of
crowds or small spaces.