No Shows - PowerPoint PPT Presentation
1 / 53
Title:
No Shows
Description:
... a participating provider will provide, by CD-ROM, or electronically at the ... and the building up a complete picture of a business model that can help track, ... – PowerPoint PPT presentation
Number of Views:52
Avg rating:3.0/5.0
Title: No Shows
1
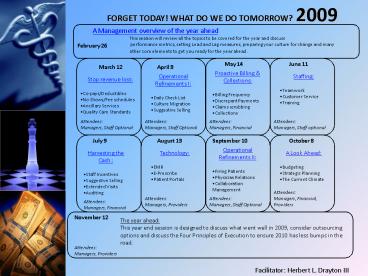
FORGET TODAY! WHAT DO WE DO TOMORROW? 2009
A Management overview of the year ahead This
session will review all the topics to be covered
for the year and discuss performance metrics,
setting Lead and Lag measures, preparing your
culture for change and many other core elements
to get you ready for the year ahead.
February 26
June 11
May 14
March 12
April 9
- Proactive Billing Collections
- Billing Frequency
- Discrepant Payments
- Claims scrubbing
- Collections
- Operational Refinements I
- Daily Check List
- Culture Migration
- Suggestive Selling
- Staffing
- Teamwork
- Customer Service
- Training
- Stop revenue loss
- Co-pays/Deductibles
- No Shows/Fee schedules
- Ancillary Services
- Quality Care Standards
Attendees Managers, Staff Optional
Attendees Managers, Staff Optional
Attendees Managers, Financial
Attendees Managers, Staff optional
September 10
August 13
July 9
October 8
- Operational Refinements II
- Firing Patients
- Physician Relations
- Collaboration Management
- Harvesting the Cash
- Staff Incentives
- Suggestive Selling
- Extended Visits
- Auditing
- Technology
- EMR
- E-Prescribe
- Patient Portals
- A Look Ahead
- Budgeting
- Strategic Planning
- The Current Climate
Attendees Managers, Financial, Providers
Attendees Managers, Providers
Attendees Managers, Staff Optional
Attendees Managers, Financial
November 12
The year ahead This year end session is
designed to discuss what went well in 2009,
consider outsourcing options and discuss the Four
Principles of Execution to ensure 2010 has less
bumps in the road.
Attendees Managers, Providers
Facilitator Herbert L. Drayton III
2
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
February 26
Office Managers Kickoff Meeting
A
Management overview of the year ahead
3
The Management Series Ground Rules
- The facilitator does not know everything
- Neither does the audience
- We are all Leaders
- We are all Managers
- We are open minded
- We do not have a scarcity mentality
- We do have an abundance mentality
- We always hire talent better than our best talent
- We develop our best talent
- No more than five power point slides per session
4
8 Stages of ChangeExcerpt from Leading Change
by John P. Kotter
- Establishing a sense of urgency
- Creating a guiding coalition
- Developing a Vision and Strategy
- Communicating the Change Vision
- Empowering Employees for Broad-Based Action
- Generating Short-Term Wins
- Consolidating Gains and Producing More Change
- Anchoring New Approaches in the Culture
5
"When you can measure what you are speaking about
and express it in numbers you know something
about it, but when you cannot measure it, when
you cannot express it in numbers, your knowledge
is of a meager and unsatisfactory kind." --Lord
Kelvin
6
Lead and Lag Measures
The lag measures are metrics that are obtained
after the event is over- the destination, whereas
the Lead measures are things that have to happen,
things you have to measure or the drivers that
help reach the destination
Lag Measure Revenue, money in the door, all
receipts for a given month
Examples of Lead Measures
- High volume services
- Weekly Receipts
- Daily Receipts
- Accounts Receivables
- Collection Activity
- Visits
- Charges
- Charge per patient
- No shows
- Cancellations
7
(No Transcript)
8
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
March 12 Stop Revenue Loss
9
The Lag measures are metrics that are obtained
after the event is over- the destination, whereas
the Lead measures are things that have to happen,
things you have to measure or the drivers that
help reach the destination
Forget Today!! What Do We Do Tomorrow??
Lag Measure Revenue, money in the door, all
receipts for a given month
Typical Lead Measures
Visits Denial Rates Deductible collections Overtime Mail Returns
Charges High Volume Services Business Unit Revenue Mix Office Supply Expense Denial Types
Charge per patient Daily Receipts Business Unit profitability Medical Supply Expense First AM Patient
No Show rate Weekly Receipts Carrier mix Claims processing First PM Patient
Cancellations Co pay Collections Ancillary Services Patient Wait time Clinical Protocols
10
Co-Pay
Forget Today!! What Do We Do Tomorrow??
- A co-pay is an agreement between the insured and
the insurer - A co-pay is a mechanism used to minimize abuse
- A co-pay must be paid at the time of service by
the insured
Deductibles
- A deductible is an agreement between the insured
and the insurer - A deductible is a mechanism used to minimize
abuse - A deductible can be used to manage the cost of
premiums - A deductible must be satisfied prior to insurer
liability activation
11
Forget Today!! What Do We Do Tomorrow??
- No Shows
- Charge a no show fee
- Utilize staff to call patients and offer to write
off no show fee if patient reschedules - Utilize an appointment reminder system
- 25 patients daily with a 15 no show rate
- (3.75 patients/day) x (260 work days) 975
visits - (975 visits) x (50) 48,750
- 25 patients daily utilizing an appointment
reminder system - (25 patients) x (260 work days) 6,500 annual
visits - 6,500 x .21 (cost of reminder service) 1,365
- Fee Schedule
- Request a fee increase annually in writing
- Be careful with links to Medicare
- Run an analysis to identify high utilization
codes - Always use catch- all language at the end of the
request
12
Ancillary Services Evaluation
Forget Today!! What Do We Do Tomorrow??
- What ancillary services are currently ordered by
the physician group from "outside" providers and
can we identify "new" ancillary services to
order? - What are the costs of the ancillary equipment and
other "hard" assets? - What support will be needed for the ancillary
service? - Does the ancillary service require third-party
approval? - Collect utilization and payer source data for the
ancillary service. - Compare the entire cost of providing the
ancillary service in-house to the anticipated
reimbursement. - Identify any contractual impediments to providing
the ancillary service. - Evaluate the proposal under the Stark Law.
- Evaluate the proposal under the Anti-Kickback
Statute. - Evaluate the proposal under the Medicare Rules.
13
Staff uncover PRACTICE MANAGER secret
14
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
April 9
Operational Refinements I
15
8 Stages of ChangeExcerpt from Leading Change
by John P. Kotter
- Establishing a sense of urgency
- Creating a guiding coalition
- Developing a Vision and Strategy
- Communicating the Change Vision
- Empowering Employees for Broad-Based Action
- Generating Short-Term Wins
- Consolidating Gains and Producing More Change
- Anchoring New Approaches in the Culture
16
- Finding Complacency and false urgency
- Are critical issues delegated to consultants or
task forces with little involvement of key
people? - Do people have trouble scheduling meetings on
important initiatives (Because, well, my agenda
is so full)? - Is candor lacking in confronting the bureaucracy
and politics that are slowing down important
initiatives? - Do meetings on key issues end with no decisions
about what must happen immediately (except the
scheduling of another meeting)? - Are discussions very inwardly focused and not
about markets, emerging technology, competitors,
and the like? - Do people spend long hours developing Power-Point
presentations on almost anything? - Do people run from meeting to meeting, exhausting
themselves and rarely if ever focusing on the
most critical hazards or opportunities? - Are highly selective facts used to shoot down
data that suggests there is a big hazard or
opportunity? - Do people regularly blame others for any
significant problems instead of taking
responsibility and changing?
17
Medicare
Providers
Staff
Our World then and Now
18
Some of the activities associated with filling a
script
Retrieving call from answering machine, transcribing to pad, call pharmacy, handwriting call backs, call to/from patient
What is it costing the practice?
10.00 12.00 14.00 16.00 18.00 20.00
1 0.17 0.20 0.23 0.27 0.30 0.33
3 0.50 0.60 0.70 0.80 0.90 1.00
5 0.83 1.00 1.17 1.33 1.50 1.67
19
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
May 14, 2009
PROACTIVE BILLING
20
18 Steps to Billing
- Initial patient contact (usually by telephone,
when this information should be updated and any
outstanding balance communicated) - Eligibility confirmed prior to appointment
- Patient registration completed or updated
- Co-payment, Deductible, Outstanding balance
collected - Services documented by ancillary staff as per
protocol - Services documented by provider
- Encounter form reviewed, additional payment
collected if applicable - Billing system updated
- Insurance claim filed within 24 hours
- Acknowledgement reports reviewed and claims
corrected - Payment received from insurance carrier
- Inquiry letter received from insurance carrier
- Denial received from insurance carrier
- Patient billed
- Patient pays the bill
- Review accounts receivable
- Collection efforts
- Account closed
21
MEDICAL PRACTICE BILLING
SEVEN DEADLY S INS
SEVEN DEADLY S INS
No Co-pay
No Deductible
OHI
Collections
Secondary claim
Accident Forms
Under-coding
SEVEN DEADLY SINS
22
"South Carolina Health Care Financial Recovery
and Protection Act" http//www.scstatehouse.gov/CO
DE/t38c059.htm SECTION 38-59-220. Requesting fee
schedule from insurer confidentiality. (A)
Within six months of the effective date of this
article, each insurer, upon written request from
a physician who is also a participating provider
will provide, by CD-ROM, or electronically at the
insurer's option, the fee schedule that is
contracted with that physician for up to 100
CPT(r) Codes customarily and routinely used by
the specialty type of such physician. Each
physician may request from an insurer an updated
fee schedule no more than two times annually.
(B) A physician requesting a fee schedule
pursuant to subsection (A) may elect to receive a
hard copy of the fee schedule in lieu of the
foregoing however, the insurer may charge the
physician a reasonable fee to cover the increased
administrative costs of providing the hard copy.
(C) The physician shall keep all fee schedule
information provided pursuant to this section
confidential. The physician shall disclose fee
schedule information only to those employees of
the physician who have a reasonable need to
access this information in order to perform their
duties for the physician and who have been placed
under an obligation to keep this information
confidential. Any failure of a physician's office
to abide by this subsection shall result in the
physician's forfeiture of the right to receive
fee schedules pursuant to this section and at the
option of the insurer may constitute a breach of
contract by the physician. (D) Nothing in this
section prohibits an insurer from basing actual
compensation to the physician on the insurer's
maximum allowable amount or other contract
adjustments, including those stated in the
patient's plan of benefits, or both. SECTION
38-59-230. Time frame for payment of clean
claims acknowledging receipt of claim
processing of electronic claims by billing
service. (A) An insurer shall direct the
issuance of a check or an electronic funds
transfer in payment for a clean claim that is
submitted via paper within forty business days
following the later of the insurer's receipt of
the claim or the date on which the insurer is in
receipt of all information needed and in a format
required for the claim to constitute a clean
claim and is in receipt of all documentation
which may be requested by an insurer which is
reasonably needed by the insurer (1) to
determine that such claim does not contain any
material defect, error, or impropriety or (2)
to make a payment determination. (B) An insurer
shall direct the issuance of a check or an
electronic funds transfer in payment for a clean
claim that is submitted electronically within
twenty business days following the later of the
insurer's receipt of the claim or the date on
which the insurer is in receipt of all
information needed and in a format required for
the claim to constitute a clean claim and is in
receipt of all documentation which may be
requested by an insurer which is reasonably
needed by the insurer (1) to determine that
such claim does not contain any material defect,
error, or impropriety or (2) to make a payment
determination. (C) An insurer shall affix to or
on paper claims, or otherwise maintain a system
for determining, the date claims are received by
the insurer. An insurer shall send an electronic
acknowledgement of claims submitted
electronically either to the provider or the
provider's designated vendor for the exchange of
electronic health care transactions. The
acknowledgement must identify the date claims are
received by the insurer. If an insurer determines
that there is any defect, error, or impropriety
in a claim that prevents the claim from entering
the insurer's adjudication system, the insurer
shall provide notice of the defect or error
either to the provider or the provider's
designated vendor for the exchange of electronic
health care transactions within twenty business
days of the submission of the claim if it was
submitted electronically or within forty business
days of the claim if it was submitted via paper.
Nothing contained in this section is intended or
may be construed to alter an insurer's ability to
request clinical information reasonably necessary
for the proper adjudication of the claim or for
the purpose of investigating fraudulent or
abusive billing practices. (D) A clearinghouse,
billing service, or any other vendor that
contracts with a provider to deliver health care
claims to an insurer on the provider's behalf is
prohibited from converting electronic claims
received from the provider into paper claims for
submission to the insurer. A violation of this
subsection constitutes an unfair trade practice
under Chapter 5, Title 39, and individual
providers and insurers injured by violations of
this subsection have an action for damages as set
forth in Section 39-5-140.
23
Lucky Seven
- Forms
- Carrier Mix
- Coding Matrix
- Billing Frequency
- Carrier Compliance
- Claims Scrubbing
- Collections
24
Scheduler, Receptionist, Clinical Staff,
Physicians (Extenders), Discharge, Insurance
Biller, Collector
25
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
June 11, 2009
Customer Service Teamwork Training
26
(No Transcript)
27
(No Transcript)
28
Hey, I was out last week- why did she say we have
to sit on these things again?
29
Teamwork, Customer Service Training
- Glossary of Terms
- Simple Scenarios
- Dos and Donts
- Telephone etiquette
30
(No Transcript)
31
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
July 9, 2009
HARVESTING THE CASH Staff
Incentives Suggestive Selling Extended
Visits Auditing
32
Success is harder to live through than failure
To make a difference in our world you have to
learn to do it different
33
Incentive Something, such as the fear of
punishment or the expectation of reward, that
induces action or motivates effort.
34
EXTENDED OFFICE VISITS and SUGGESTIVE SELLING
Level 4 Office Visits
35
AUDITING
- Charges
- Surgeries/Procedures
- DME
- Financials
- Carrier AR
- Carrier Compliance
- Patient AR
- EOBs
- Scheduled Ancillary Services
- Global periods
- Incident to Billing
36
The Paradoxical Commandmentsexcerpt from The
8th Commandment by Stephen Covey
- People are illogical, unreasonable, and self
centered. Love them anyway - If you do good, people will accuse you of selfish
ulterior motives. Do good anyway - If you are successful, you will win false
friends and true enemies. Succeed anyway. - The good you do today will be forgotten tomorrow.
Do good anyway. - Honesty and frankness make you vulnerable. Be
honest and frank anyway. - The biggest men and women with the biggest ideas
can be shot down by the smallest men and women
with the smallest mind. Think big anyway. - People favor underdogs but follow only top dogs.
Fight for a few underdogs anyway. - What you spend years building may be destroyed
overnight. Build anyway. - People really need help but may attack you if you
do help them. Help people anyway. - Give the world the best you have and youll get
kicked in the teeth. Give the world the best you
have anyway - KENT KEITH
37
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
August 13, 2009
Technology EMR E-Prescribe
Patient Portals
38
(No Transcript)
39
Do not Implement electronic prescribing or
Electronic Medical Records for the following
reasons
- Safe
- Secure
- Formulary Discipline
- Generic Utilization
- Provider Efficiency
- Drug-Drug Interaction
- Allergy Interaction
- Pharmacy Call backs
- Patient Calls
- Handwriting Errors
- Multiple MDs Share data
- Less Paper work
- Faster Access to Data
- Prevent Medication Errors
- Reduced Insurance Premiums
- Improved Reimbursement Rates
- Increase Patient Satisfaction
- Clinical Trials Revenue
- Increased Patient Safety
40
South Carolina Facts Year End 2008
- of Patient Visits w. a Prescription Benefit
Request 2.59 National Rank 47 - of Total Prescriptions Routed Electronically
- 1.25 National Rank 48
- of Physicians Routing E-Prescriptions at Year
End - 6.71 National Rank 43
- of Patients with Available Rx Benefit
Information 61.13 National Rank 31 - of Total Community Pharmacies E-Prescribing
- 78.80 National Rank 21
41
Some of the activities associated with filling a
script
Retrieving call from answering machine, transcribing to pad, pharmacy calls, handwriting call backs, call to/from patient
What is it costing the practice?
10.00 12.00 14.00 16.00 18.00 20.00
1 0.17 0.20 0.23 0.27 0.30 0.33
3 0.50 0.60 0.70 0.80 0.90 1.00
5 0.83 1.00 1.17 1.33 1.50 1.67
42
Leaders and managers either stand out or out in
front
43
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
September 10, 2009
Operational Refinements Firing
Patients Physician Relations Collaboration
Management
44
Bullying surgeons. Power-pimping attending.
Boorish residents.
Firing Patients
45
"Collaboration Management Framework
Its central concept is the "conversation" which
consists of a series of business
documents/information exchanged under common
subjects among practices. The framework defines
how to define, manage, and implement
conversations. The framework enables integrating
B-to-B (external) processes as well as in B
(internal) processes being executed in multiple
systems, and the building up a complete picture
of a business model that can help track, enhance
and analyze the system behavior.
46
Leadership Necessities
- Positioning and Repositioning Finding a central
idea for business that meets customer demands
and that makes money - Pinpointing External Change Detecting patterns
in a complex world to put the business on the
offensive - Leading the Social System Getting the right
people together with the right behaviors and the
right information to make better, faster
decisions and achieve business results - Judging People Calibrating people based on their
actions, decisions, and behaviors and matching
them to the non-negotiable elements of the job - Molding a Team Getting highly competent,
high-ego leaders to coordinate seamlessly - Setting Goals Determining the set of goals that
balances what the business can become with what
it can realistically achieve - Setting Laser-Sharp Priorities Defining the path
and aligning resources, actions, and energy to
accomplish the goals - Dealing with Forces Beyond the Market
Anticipating and responding to societal pressures
you dont control but that can affect your
business
47
- Ambition
- Drive and Tenacity
- Self Confidence
- Psychological Openness
- Realism
- Appetite for Learning
48
Cognitive Traits that improve the Know-Hows
- A Wide Range of Altitude- to transition from the
conceptual to the specific - A Broad Cognitive Bandwidth- to take in a broad
range of input and see the big picture - Ability to Reframe- to see things
from different perspectives or simply as they are
49
Office Management 2009 Series Forget Today!!
What Do We Do Tomorrow??
October 7
Office Managers Kickoff Meeting
A
Management overview of the year ahead
50
(No Transcript)
51
(No Transcript)
52
- The challenges in implementing performance
measurement arise in the following areas - Technical
- Data quality latency, application usability,
visualization of data - Organizational
- Business culture, leadership, processes,
strategic control and intent - Individual
- Gesturing, biases, framing and decision-making
abilities - Overcoming these challenges are not as simple as
finding the right software or hiring more people,
establishing the set of best practices and
implementing them with precision and consistency
is what need to happen. Issues in each of these
areas are teased out of some of the sessions we
have had throughout the year.
53
- The development of performance measures plays an
important role in formulating and clarifying
plans and strategies and setting targets for
providers, employees, project teams and business
units. - Performance measures should be part of a
consistent performance measurement system which
connects measures from all aspects of the
practice- registration, nursing, provider,
check-out, billing, collections, etc. - A performance measurement system should also
ensure that a limited and manageable number of
measures is chosen and that the measures are
balanced.