Cognitive%20Decline - PowerPoint PPT Presentation
Title:
Cognitive%20Decline
Description:
Histology: Amyloid plaques & neurofibrillary tangles ... Amyloid angiopathy ... on GRE/SWI MRI for amyloid angiopathy. Clinical Diagnosis. Mixed dementia ... – PowerPoint PPT presentation
Number of Views:99
Avg rating:3.0/5.0
Title: Cognitive%20Decline
1
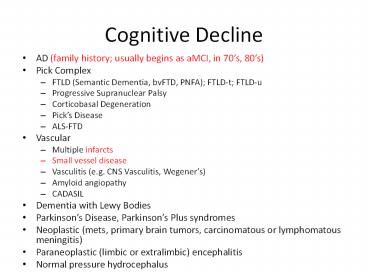
Cognitive Decline
- AD (family history usually begins as aMCI, in
70s, 80s) - Pick Complex
- FTLD (Semantic Dementia, bvFTD, PNFA) FTLD-t
FTLD-u - Progressive Supranuclear Palsy
- Corticobasal Degeneration
- Picks Disease
- ALS-FTD
- Vascular
- Multiple infarcts
- Small vessel disease
- Vasculitis (e.g. CNS Vasculitis, Wegeners)
- Amyloid angiopathy
- CADASIL
- Dementia with Lewy Bodies
- Parkinsons Disease, Parkinsons Plus syndromes
- Neoplastic (mets, primary brain tumors,
carcinomatous or lymphomatous meningitis) - Paraneoplastic (limbic or extralimbic)
encephalitis - Normal pressure hydrocephalus
2
Shortness of Breath
- CHF
- Cardiomyopathy
- Acute MI
- Neurogenic (e.g. SAH, stroke)
- Atrial fibrillation
- Pneumonia
- Aspiration (Dysphagia)
- Infectious
- Interstitial
- Idiopathic Pulmonary Fibrosis
- Neuromuscular Disease
- ALS
- MG
- Polymyositis, dermatomyositis
3
Dysphagia
- Obstructive
- Neurogenic
- Brain
- Neurodegenerative (e.g. PSP)
- Vascular (usually brainstem when chronic)
- Tumor
- Infection
- Motor Neuron (e.g. ALS)
- NM junction (e.g. MG)
- Lower motor neuron (e.g. GBS)
- Muscle (e.g. Polymyositis oculopharyngeal
muscular dystrophy)
4
Renal Failure
- Dehydration
- Poor intake secondary to dysphagia
- Vomiting (hyponatremia, hyperkalemia)
- Dye
- Medications
- Infections
- Amyloidosis
- Wegeners (affects brain, lung, as well as kidney)
5
AD
- Progressive decline in memory 1 other domain
of cognition - family history (but not especially important
unless there is family history of early onset AD,
in 40s or 50s usually APP or presenilin I or
II mutation) - usually begins as amnestic MCI
- Usually begins in 70s or 80s
- Histology Amyloid plaques neurofibrillary
tangles - Cant account for dysphagia, SOB, gait
impairment, or renal failure. AD patients have
poor p.o. intake because they forget to eat.
6
Pick Complex Clinical Subtypes
- FTLD (Semantic Dementia, bvFTD, PNFA)
- Primary Progressive Aphasia /or
- Change in personality, comportment, behavior
- Progressive Supranuclear Palsy syndrome
- Dysphagia, Dysarthria (UMN, spastic),
pseudobulbar lability - Falls, Gait Disorder
- Impaired eye movements
- Dementia
- Usually begins in 50s or 60s
- Corticobasal Syndrome (spastic hemiparesis,
apraxia) - ALS-FTD
- Dysphagia, Dysarthria (UMN LMN)
- Falls, Gait Disorder, Weakness, Spasticity
- Usually begins in 40s, 50s, or 60s
- All can be associated with Parkinsonism,
Rigidity, Tremor
7
Pathological Classification of FTLD/Pick Complex
- Tau-opathies
- Picks Disease (Pick bodies)
- PSP
- Corticobasal degeneration
- ALS-Parkinsonism-Dementia Complex of Guam
- Tangle dominant dementia
- Diffuse neurofibrillary tangle demenia with
calcifications - Agyrophilic grain disease
- Sporadic multisystem tauopathy
8
Pathological Classification of FTLD/Pick Complex
- Ubiquitinopathies
- TDP 43 FTLD-U types 1-4 (ALS-FTD, FTD, ALS)
- FTLD-PLS
- FTLD-non-TDP (many have hippocampal sclerosis)
- Other
- DLDH Dementia Lacking Distinctive Histology
- Basophilic inclusion body disease
- FTLD CHMP2B
- Neurofilament inclusion body disease
9
Vascular Cognitive Decline
- Multiple infarcts
- Just has one lacune
- Small vessel disease
- Mild to moderate
- Vasculitis
- No large vessel strokes
- No headaches
- Amyloid angiopathy
- No hemorrhage on CT (but dx requires gradient
echo/susceptability/ hemosiderin MRI - CADASIL
- Too old, no family history, no headache
10
Dementia with Lewy Bodies
- Parkinsonism (tremor, rigidity, gait disorder)
- Hallucinations
- Marked fluctuations in mental state
- Marked visuospatial deficits
- Autonomic dysfunction
- Orthostatic hypotention
- Sensitivity to neuroleptics
Cant account for dysphagia, SOB, gait
impairment, or renal failure
11
Parkinsons
- Parkinsons Disease
- Unilateral onset
- Bradykinesia, bradyphrenia
- Tremor
- Rigidity
- Gait disorder, falls
- Subcortical cognitive decline
- Can have dysphagia and dementia, but usually not
so prominent - Parkinsons Plus syndromes
- Multisystem Atrophy
- Shy-Drager
12
Neoplastic
- Brain mets
- primary brain tumors
- carcinomatous or lymphomatous meningitis
- Gliomatosis cerebrii
- Paraneoplastic encephalitis
- CT negative for tumor
- Too chronic for neoplastic meningitis or
gliomatosis cerebrii
13
Infectious
- HIV
- Subcortical cognitive decline
- Slow, poor recall, poor executive dysfunction
- Lyme
- Sero-positive, CSF
- Can cause arrhythmia
- No fever
- Too chronic
- West Nile
- No fever
- Too chronic
14
What can account for cognitive decline SOB
Dysphagia?
- Proteinopathies protein misfolding disorders
- ALS-FTD
- Usually ubiquitin-opathy
- usually TDP-43 transactivation response (TAR)
DNA binding protein, molecular weight 43 kDa - Nuclear protein involved in transcription,
alternative splicing - Cytoplasmic inclusions
- 4 subtypes distinct distributions cause SD,
ALS-FTD or bvFTD, bvFTD - Many have progranulin mutation 17q21 (PRGN)
- Others have mutations in 9q21-12 (VCP) or 9p21-13
or CHMP2B - Family history in 7.7 (ALS) to 62. (FTD
FTLD-U) - Geser et al., 2009 Archives of Neurology
- Bulbar onset with dysphagia and respiratory
difficulty in 32-38 - Onset is usually in 40s-60s, disease duration
1-4 years
15
What can account for cognitive decline SOB
Dysphagia?
- Progressive Supranuclear Palsy
- Dysphagia dysarthria, Falls, Parkinsonism/Rigidi
ty, Vertical Eye Movement Impairment, Dementia or
Aphasia - Tau-opathy (another protein misfolding disorder),
specific isoform often causes PSP - Many have mutations in Chr 3 or 17q21 (MAPT)
associated with variable isoforms of tau - Same mutation can cause PSP in 1 family member,
corticobasal syndrome in another, and progressive
nonfluent aphasia or bvFTD (types of FTLD-t) in
another - Usually starts in 50s or 60s with duration of
6-12 years.
16
Does Exam Help?
- AD should have normal neurological exam except
dementia - ALS-FTD should have
- Fasciculations (LMN)
- Hyperreflexia (reflexes appeared symmetric)
- Babinski /or Hoffman signs (UMN)
- Weakness (limb or bulbar) 3 limbs but poor
effort - Dysarthria (usually present if neurogenic
dysphagia is present) - Dementia
- PSP should have
- Impaired eye movements, dysphagia/dysarthria,
rigidity or tremor, gait impairment, dementia
17
Does Imaging Help?
- AD
- Bilateral temporoparietal atrophy on CT, MRI
- Bilateral temporoparietal hypoperfusion on SPECT
- Bilateral temporoparietal hypometabolism on PET
- (PIB in amyloid PET)
- ALS-FTD
- Asymmetric fronto/temporal atrophy on CT, MRI
- Asymmetric fronto/temporal abnormalities on PET
or SPECT or MRS - PSP (and other tau-opathies)
- May see frontal /or parietal atrophy on CT, MRI
- midbrain superior cerebellar peduncle atrophy
for PSP - Vascular Dementia
- Strokes and/or white matter disease on CT, MRI
- Microhemorrhages on GRE/SWI MRI for amyloid
angiopathy
18
Clinical Diagnosis
- Mixed dementia
- Protein-opathy (with some evidence of vascular
disease /- AD) - Most likely tau-opathy unless fasciculations or
hyperreflexia were missed on exam - May have presented late due to his cognitive
reserve - Physicists and other highly educated people often
compensate well for substantial cognitive decline - This mans obvious onset was about age 75, but
decline might well have started in his 60s