Scleroderma - PowerPoint PPT Presentation
Title:
Scleroderma
Description:
Title: Chest Pain, SOB, Tachycardia Author: net_serv Last modified by: Blair Holbein Created Date: 10/20/1998 1:46:58 PM Document presentation format – PowerPoint PPT presentation
Number of Views:259
Avg rating:3.0/5.0
Title: Scleroderma
1
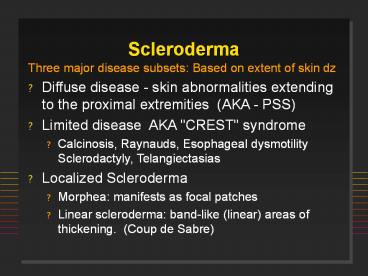
Scleroderma
- Three major disease subsets Based on extent of
skin dz - Diffuse disease - skin abnormalities extending to
the proximal extremities (AKA - PSS) - Limited disease AKA "CREST" syndrome
- Calcinosis, Raynauds, Esophageal dysmotility
Sclerodactyly, Telangiectasias - Localized Scleroderma
- Morphea manifests as focal patches
- Linear scleroderma band-like (linear) areas of
thickening. (Coup de Sabre)
2
(No Transcript)
3
Other causes of Tight Skin
- Pseudosclerodactyly
- IDDM, Hypothyroidism
- Drugs Tryptophan, bleomycin, pentazocine, vinyl
chloride, solvents - Eosinophilic fasciitis
- Overlap Conditions
- Scleroderma-like conditions
- Eosinophil myalgia syndrome (tryptophan)
- Porphyria cutanea tarda
4
ACR Systemic Sclerosis Preliminary Classification
Criteria
- Major Criterion
- Proximal Scleroderma
- Minor Criteria
- Sclerodactyly
- Digital pitting or scars or loss of finger pad
- Bibasilar pulmonary fibrosis
One major and two minor required for diagnosis
5
Scleroderma Onset
- 80 females
- Age 50 are lt 40 yrs _at_ onset (20-50)
- Incidence 20/million/year
- Raynauds
- Swollen or puffy digits
- Loss of skin folds, no hair growth
- Digital pulp sores/scars
- Arthralgias gtgt Arthritis
6
SclerodermaA disorder of Collagen, Vessels
- Etiology unknown?
- Autoimmune disorder suggested by the presence of
characteristic autoantibodies such as ANA,
anti-centromere and anti-SCL-70 antibodies. - Pathology
- Early dermal changes lymphocytic infiltrates
primarily of T cells - Major abnormality is collagen accumulation with
fibrosis. - Small to medium-sized blood vessels, which show
bland fibrotic change. - Small thrombi may form on the altered intimal
surfaces. - Microvascular disease
Cold
Normal
Cold
PSS
7
PSS - Clinical
- Skin
- Skin thickening is most noticeable in the hands,
looking swollen, puffy, waxy. - Thickening extends to proximal extremity, truncal
and facial skin thickening is seen. - Raynaud's phenomenon is present.
- Digital pits or scarring of the distal digital
pulp - Musculoskeletal Arthralgias and joint stiffness
are common. - Palpable tendon friction rubs associated with an
increased incidence of organ involvement. - Muscle weakness or frank myositis can be seen.
8
(No Transcript)
9
(No Transcript)
10
(No Transcript)
11
(No Transcript)
12
(No Transcript)
13
(No Transcript)
14
(No Transcript)
15
(No Transcript)
16
PSS - Clinical
- Gastrointestinal Esophageal dysmotility,
dysphagia, malabsorptive or blind loop syndrome,
constipation. - Renal Kidney involvement is an ominous finding
and important cause of death in diffuse
scleroderma. A hypertensive crisis (AKA renal
crisis) may herald the onset of rapidly
progressive renal failure.
17
(No Transcript)
18
(No Transcript)
19
(No Transcript)
20
Pulmonary Manifestations of PSS
- Dyspnea
- Pulmonary HTN only in CREST
- Interstitial fibrosis (fibrosing alveolitis)
- High resolution CT vs Galium Scan
- Major cause of death
- RARE
- Pulmonary embolism
- Pulmonary vasculitis
21
Cardiac Findings in PSS
- Myocardial fibrosis
- Dilated cardiomyopathy
- Cor pulmonale
- Arrhythmias
- Pericarditis
- Myocarditis
- Congestive heart failure
22
(No Transcript)
23
Comparison CREST v. PSS
Ab antibody Relative percentages
81-100 61-80 41-60 21-40
1-20
24
Treatment of Scleroderma
- Localized none
- Raynauds warmth, skin protection, vasodilator
therapy - CREST none
- PSS none proven
- Penicillamine controversy
- Cytoxan for lung disease?
- Steroids have no value
25
PolymyositisDermatomyositis
- FM 21
- Acute onset
- Weakness ( myalgia) Proximal gt Distal
- Skeletal muscle dysphagia, dysphonia
- Sx Rash, Raynauds, dyspnea
- 65 elevated CPK, aldolase
- 50 ANA ()
- 90 EMG 85 muscle biopsy
26
Proposed Criteria for Myositis
- Symmetric proximal muscle weakness
- Elevated Muscle Enzymes (CPK, aldolase, AST, ALT,
LDH) - Myopathic EMG abnormalities
- Typical changes on muscle biopsy
- Typical rash of dermatomyositis
- PM Dx is Definite w/ 4/5 criteria and Probable
w/3/5 criteria - DM Dx Definite w/ rash and 3/4 criteria and
Probable w/ rash and 2/4 criteria
27
Polymyositis ClassificationBohan Peter
- Primary idiopathic dermatomyositis
- Primary idiopathic polymyositis
- Adult PM/DM associated with neoplasia
- Childhood Dermatomyositis (or PM)
- often associated with vasculitis
- Myositis associated with collagen vascular disease
28
(No Transcript)
29
MYOPATHY HISTORICAL CONSIDERATIONS
- Age/Sex/Race
- Acute vs. Insidious Onset
- Distribution Proximal vs. Distal
- Pain?
- Drugs/Pre-existing Conditions
- Neuropathy
- Systemic Features
30
(No Transcript)
31
MYOPATHIIES
- Toxic/Drugs
- Etoh, Cocaine, Steroids, Plaquenil,
Penicilamine, Colchicine, AZT, Lovastatin,
Clofibrate, Tryptophan, Taxol, Emetine - Infectious
- Coxackie A9, HBV, HIV, Stept., Staph,
Clostridial, Toxoplasma, Trichinella - Inflammatory Myopathies
- Congenital
- Neuropathic/Motor Neuron Disorders
- Endocrine/Metabolic
32
NONMYOPATHIC CONSIDERATIONS
- Fibromyalgia/Fibrositis/Myofascial Pain Disorder
- Polymyalgia Rheumatica
- Caucasians, gt 55 yrs, MF
- ESR gt 100, normal strength, no synovitis
- RA
- SLE
- Adult Still's Disease
33
INFLAMMATORY MYOSITISImmunopathogenesis
- Infiltrates - T cells (HLA-DR) monocytes
- Muscle fibers express class I II MHC Ags
- T cells are cytotoxic to muscle fibers
- t-RNA antibodies role? FOUND IN lt50 OF PTS
- Infectious etiology? Viral implicated
- HLA-B8/DR3 in childhood DM
- DR3 and DRW52 with t-RNA synthetase Ab
34
DERMATOMYOSITIS5 Skin Features
- Heliotrope Rash over eyelids
- Seldom seen in adults
- Gottrons Papules MCPs, PIPs, MTPs, knees, elbows
- V-Neck Rash violaceous/erythema anterior chest
w/ telangiectasias - Periungual erythema, digital ulcerations
- Calcinosis
35
(No Transcript)
36
(No Transcript)
37
(No Transcript)
38
(No Transcript)
39
(No Transcript)
40
(No Transcript)
41
Calcinosis
42
(No Transcript)
43
DIAGNOSTIC TESTING
- Physical Examiniation Motor Strength (Gowers
sign), Neurologic Exam - Acute phase reactants unreliable
- Muscle Enzymes
- CPK elevated gt65 gt10 MB fraction is possible
- Muscle specific- Aldolase, Troponin, Carb.
anhydraseIII - AST gt LDH gt ALT
- Beware of incr. creatinine (ATN) and
myoglobinuria - Electromyogram increased insertional activity,
amplitude, polyphasics, associated neuropathic
changes, incremental/decremental MU changes
44
DIAGNOSTIC TESTING
- Muscle Biopsy (an URGENT not elective procedure)
- Call the neuropathologist! 85 Sensitive.
- Biopsy involved muscle (MRI guided)
- Avoid EMG/injection sites or sites of trauma
- Magnetic Resonance Imaging - detects incr. water
signal, fibrous tissue, infiltration,
calcification - Investigational Tc-99m Scans, PET Scans
- Serologic Tests ANA () 60, Abs against
t-RNA synthetases
45
INFLAMMATORY MYOSITISBiopsy Findings
- Inflammatory cells
- Edema and/or fibrosis
- Atrophy/ necrosis/ degeneration
- Centralization of nuclei
- Variation in muscle fiber size
- Rarely, calcification
46
(No Transcript)
47
(No Transcript)
48
Anti-synthetase syndrome ILD, fever, arthritis,
Raynauds, Mechanics hands
49
Autoantibodies in PM/DM
Ab Freq () Clinical Syndrome
ANA 50 Myositis
U1-RNP 15 SLE myositis
Ku lt5 PSS myositis
Mi2 30 Dermatomyositis
PM1 15 PSS PM overlap
Jo-1 25 Arthritis ILD arthritis
SS-B (La) lt5 SLE,Sjogrens, ILD, PM
PL-12,7 lt5 ILD PM
50
(No Transcript)
51
(No Transcript)
52
INFLAMMATORY MYOSITIS
- NORMAL/NOT INVOLVED
- Face Uncommon
- Renal
- RES LN, spleen, liver (enzymes from muscle)
- NOT UNCOMMON
- RA-like arthritis
- Fever/chills/night sweats
- Myalgias
53
MALIGNANCY MYOSITIS
- Controversial
- Reports range from 10-25
- If real, men over age 50 yrs at greatest risk
- Common tumors Breast, lung, ovary, stomach,
uterus, colon - 60 the myositis appears 1st, 30 neoplasm 1st,
and 10 contemporaneously - Avoid invasive, expensive searches for occult
neoplasia
54
PM/DM Complications
- PULMONARY
- Aspiration pneumonitis
- Infectious pneumonitis
- Drug induced pneumonitis
- Intercostal, diagphragm involvement
- Fibrosing alveolitis
- RARE
- Pulmonary vasculitis
- Pulmonary neoplasia
- CARDIAC
- Elev. CPK-MB
- Mitral Valve prolapse
- AV conduction disturbances
- Cardiomyopathy
- Myocarditis
55
PM/DM Diagnosis
- Symmetric progressive proximal weakness
- Elevated muscle enzymes (CPK, LFTs)
- Muscle biopsy evidence of myositis
- EMG inflammatory myositis
- Characteristic dermatologic findings
56
INFLAMMATORY MYOSITISTreatment
- Early Dx, physical therapy, respiratory Rx
- Corticosteroids 60-80 mg/day
- 80 respond within 12 weeks
- Steroid resistant
- Methotrexate
- Azathioprine
- IVIG, Cyclosporin, Chlorambucil unproven
- No response to apheresis
57
PROGNOSIS
- Poor in pts. with delayed Dx, low CPK, early
lung or cardiac findings, malignancy - Neoplasia in 10 of adults
- PT for muscle atrophy, contractures, disability
- Kids50 remission, 35 chr active disease
- Adult lt 20 yrs. do better than gt55 yrs.
- Adults Mortality rates betw. 28-47 _at_ 7 yrs.
- Relapses functional disability are common
- Death due to malignancy, sepsis, pulm. or
cardiac failure, and complications of therapy
58
RHABDOMYOLYSIS
- Injury to the sarcolemma of skeletal muscle with
systemic release of muscle macromolecules such as
CPK, aldolase, actin, myoglobin, etc - Maybe LIFE-THREATENING from hyperkalemia, met.
acidosis, ATN from myoglobinuria - Common causes EtOH, Cocaine, K deficiency,
infection, PM/DM, infection (clostridial, staph,
strept), exertion/exercise, cytokines
59
INCLUSION BODY MYOSITIS
- Bimodal age distribution, maybe hereditary
- Slow onset, progressive weakness
- Painless, distal and proximal weakness
- Normal or mildly elevated CPK
- Poor response to corticosteroids
- Dx light microscopy may be normal or show CD8
lymphs. Tubulofilamentous inclusion bodies on
electron microscopy - Role for amyloid?
60
Inflammatory Myositis
- Polymyositis (PM) and dermatomyositis (DM) are
types of idiopathic inflammatory myopathy (IIM).
IIM are characterized clinically by proximal
muscle weakness - Etiology There is now known etiology.
- Demographics PM is more common than DM in
adults. Peak incidence occurs between 40 and 60
yrs. FM 21 - Muscles Proximal muscle weakness, dysphagia,
aspiration. respiratory failure or death. - Skin Gottron's papules, heliotrope rash, "V"
neck rash, periungual erythema, "Mechanic's
hands", calcinosis - Dx Muscle enzymes (CPK, aldolase), EMG, Biopsy
- Rx Steroids, MTX, Azathioprine, IVIG