Transplantation of tissues and organs (Chapter 15) - PowerPoint PPT Presentation
1 / 51
Title:
Transplantation of tissues and organs (Chapter 15)
Description:
Title: PowerPoint Presentation Subject: The Immune System Author: Parham Last modified by: student Created Date: 12/16/2002 8:36:41 PM Document presentation format – PowerPoint PPT presentation
Number of Views:501
Avg rating:3.0/5.0
Title: Transplantation of tissues and organs (Chapter 15)
1
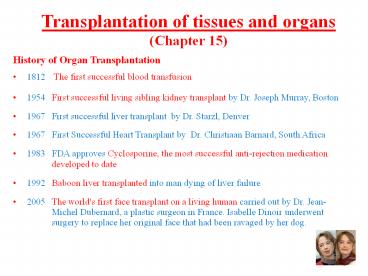
Transplantation of tissues and organs(Chapter 15)
- History of Organ Transplantation
- 1812 The first successful blood transfusion
- 1954 First successful living sibling kidney
transplant by Dr. Joseph Murray, Boston - 1967 First successful liver transplant by Dr.
Starzl, Denver - 1967 First Successful Heart Transplant by Dr.
Christiaan Barnard, South Africa - 1983 FDA approves Cyclosporine, the most
successful anti-rejection medication developed
to date - 1992 Baboon liver transplanted into man dying
of liver failure - 2005 The world's first face transplant on a
living human carried out by Dr. Jean- Michel
Dubernard, a plastic surgeon in France. Isabelle
Dinoir underwent surgery to replace her
original face that had been ravaged by her dog.
2
Immune responses against transplanted tissues
- Immune responses against transplanted tissue or
organs are caused by genetic differences between
donor and recipient, most often in the HLA
molecules. - During transplantations, the HLA molecules
represent antigens against which the immune
response is directed. - These antigens that vary between members of the
same species are called alloantigens, and the
immune responses they induce are called
alloreactions. - Immunogenetics studies genetics of alloantigens.
- Blood transfusion is the most widespread kind of
transplantation in clinical medicine - Graft the transplanted organ
3
Matching donor and recipient for HLA class I and
II molecules improves the outcome of
transplantation
- The major cause of graft rejections are the
differences in the HLA class I and II molecules
within the populations. - Only in the case of identical twins, the HLA
class I and II molecules are identical, and there
is no risk of alloreactivity during
transplantations. - During transplantations, the donor and recipients
are analyzed for HLA class I and II compatibility
(by serological assays based on monoclonal
antibodies). - The immunogenetic differences (in the HLA class I
and II molecules) are much smaller within a
family than within the whole populations ?
clinical outcomes are better between relatives
(siblings) than between unrelated people.
4
Alloreactions during transplantations
Transplant rejection and graft-versus-host
reaction are immune responses caused by genetic
differences between transplant donors and
recipients
5
Sources of transplanted organs (grafts)
- Autografts Tissues transplanted from one site to
another on the same person (skin transplantations
in burn patients). - Isografts Transplantation between genetically
identical individuals (twins). - Allografts Transplantations between two
genetically different individuals. - Xenografts Transplantations between two
different species (humans and monkeys or pigs
not routinely used raise many scientific and
ethical issues).
6
In blood transfusions, donors and recipients are
matched for the A, B, O system of blood group
antigens
- The first blood transfusion was performed in
1812. - Today, the blood transfusion is the most common
clinical transplantation procedure. - There are no HLA molecules on erythrocytes
- However, the major immunogenetic barrier to
transfusion with red blood cells arises from
structural variety in the carbohydrates present
on the erythrocyte surface. - The resulting differences in these carbohydrates
are the molecular basis for the A, B, O blood
group system. - The antigens in the ABO system are glycoproteins
with their sugar residues exposed at the
erythrocyte surface. The terminal sugar
determines whether the antigen is A or B. - The critical principle is that people usually
have antibodies against those erythrocyte
antigens that they lack. - Why do we have antibodies against erythrocyte
antigens that we lack? Bacteria living in our
intestine express antigens similar to those on A
and B. We synthesize antibodies against these if
we do not have the corresponding antigens that
is, if our immune system sees them as "foreign"
rather than "self".
7
Structure of the A, B, O blood group antigens
8
ABO blood grouping system
- Blood group AIf you belong to the blood group A,
you have A antigens on the surface of your red
blood cells and B antibodies in your blood
plasma. - Blood group BIf you belong to the blood group B,
you have B antigens on the surface of your red
blood cells and A antibodies in your blood
plasma. - Blood group ABIf you belong to the blood group
AB, you have both A and B antigens on the surface
of your red blood cells and no A or B antibodies
at all in your blood plasma.People with type AB
blood are called universal recipients. This means
they can get any type of blood. - Blood group 0If you belong to the blood group 0
(null), you have neither A or B antigens on the
surface of your red blood cells but you have both
A and B antibodies in your blood plasma. About
40 the population has type O blood. People with
this blood type are called universal donors. Type
O blood is used for emergencies when there's no
time to test a person's blood type.
9
Donors and recipients for blood transfusions must
be matched for the A, B, 0 system of blood group
antigens
YES
NO
NO
NO
NO
NO
YES
YES
YES
YES
NO
NO
YES
YES
YES
YES
10
10
11
Ethnic Distribution of ABO Blood Types
PEOPLE GROUP O () A () B () AB ()
Asian 40 28 27 5
Austrians 36 44 13 6
Blackfoot (N. Am. Indian) 17 82 0 1
Bororo (Brazil) 100 0 0 0
Brazilians 47 41 9 3
Czechs 30 44 18 9
Danes 41 44 11 4
Egyptians 33 36 24 8
English 47 42 9 3
French 43 47 7 3
Germans 41 43 11 5
Japanese 30 38 22 10
Malaysians 62 18 20 0
Mayas 98 1 1 1
Norwegians 39 50 8 4
Persians 38 33 22 7
Peru (Indians) 100 0 0 0
Russians 33 36 23 8
Spanish 38 47 10 5
USA 45 30 20 5
Vietnamese 42 22 30 5
Mean 43.91 34.80 16.55 5.14
11
12
Types of graft rejections
- Hyper-acute Caused by presence of pre-existing
antibodies that bind to the cells/tissues of the
transplanted organ comparable to type III
hyper-sensitivity reactions, in which complement
is activated within blood vessel walls, causing
blood clotting and hemorrhage. Occurs
immediately, before the patient leaves the
operating room. Can be prevented by careful
cross-matching between the donor and the
recipient. Example Blood group antibodies A, B,
O reactions against the graft. - Acute Caused by alloreactive T cells that
recognize the donors HLA-derived antigens,
migrate to the transplanted organ and destroy it.
Occurs days after transplantation. Can be
prevented by matching the donor and recipient for
HLA class I and II molecules, and by
immunosuppressive drugs. - Chronic Mediated by alloreactive T cells that
induce production of anti-HLA alloantibodies by
activated naive B cells. Occurs months or years
after transplantation.
13
Hyperacute Rejections Antibodies against A, B, O
or HLA antigens can cause hyper-acute rejection
of transplanted organs
- A, B, O antigens are expressed also on the
endothelial cells of blood vessels this is an
important factor during transplantations of solid
organs, such as kidneys. - For example, if a recipient of group O were to
receive a kidney from a donor type A, the anti-A
antibodies in the recipient would quickly bind to
the blood vessel walls in the donated kidney.
This would result in an immediate activation of
the complement and rejection of the graft
(donated organ). - This type of reaction is called hyper-acute
rejection, and occurs immediately before the
patient leaves the operating room. It is directly
comparable to type III hypersensitivity
reactions. - To avoid the hyper-acute rejections, patients and
donors are carefully cross-matched.
14
Hyper-acute rejection is caused by preexisting
antibodies binding to the graft
15
Acute Rejections Caused by effector T cells
responding to HLA differences between donor and
recipient
- Most transplantations are made across some HLA
class I and II differences. - In this situation, the recipient T cells react
against the donors HLA class I and II molecules
that are not shared by the recipient. - CD8 cells respond to HLA class I differences,
while CD4 cells respond to HLA class II
differences. - These alloreactive T cells can attack the donated
organ and destroy it, causing acute rejection. - This acute rejection occurs days after the
transplantation and can be prevented by
immunosuppressive drugs or anti-T cell
antibodies. - The acute rejection mediated by T cells is
directly comparable to type IV hyper-sensitivity
reactions.
16
Chronic Rejections Mediated by alloreactive T
cells that induce production of antibodies
- Chronic rejections occur months or years after
the transplantation. - They are caused by alloreactive T cells that
induce activation of naive B cells specific for
the allergenic HLA antigens, and production of
anti-HLA alloantibodies. - This type of rejection is responsible for more
than half of all kidney and heart transplants
within 10 years after transplantation. - Now that there are treatments for acute
rejection, chronic rejection is the major cause
of graft loss. Most recipients must take
immunosuppressive drugs for the rest of their
lives, and even that may not be enough to combat
chronic rejection.
17
Immunosuppressive drugs
- Used in clinical transplantations to suppress
alloreactions that would otherwise lead to
transplant rejection. - Because of their immunosuppressive properties,
these drugs are associated with increased
susceptibility to infections. - Generally used in combinations so that their
immunosuppressive effects are additive while
their toxic effects are not. - 1. Corticosteroids
- 2. Cytotoxic drugs
- 3. Drugs inhibiting T cell activation
18
- Corticosteroids
- Potent immunosuppressive drugs that inhibit
inflammation and leukocyte activation. - The mechanism consists of inhibiting
transcription factor NFkB that induces synthesis
of many of the pro-inflammatory proteins. - Have many serious side effects such as increased
glucose (diabetes), increased susceptibility to
infections, and adverse neuro-developmental
effects.
19
Cytotoxic drugs
- Interfere with DNA replication, thus killing
proliferating cells. - Azathioprine and cyclophosphamide are the most
commonly used cytotoxic drugs for immune
suppression. Side effects include nausea and
vomiting, hair loss, low blood cell counts, and
fetal damage or death. - Cytotoxic drugs are usually given at high doses
with a transplant to block acute rejection and
then at lower doses with corticosteroids for
maintenance.
20
Drugs inhibiting T cell activation
- Selective drugs that specifically inhibit T cell
activation first introduced in 1970s, greatly
improving outcomes of transplantations. - Disrupt signal transduction from the T cell
receptor in activated T cells. - Represented by cyclosporin and tacrolimus, which
inhibits signal transduction in activated T
cells, thus inhibiting IL-2 synthesis that is
essential for T cell proliferation and
differentiation. - Cyclosporin A is derived from the Norwegian soil
fungus Tolypodcladium inflatum. Tacrolimus (FK
506) comes from the Japanese filamentous
bacterium Streptomyces tsukabaensis rapamycin, a
closely related drug also from Streptomyces is
currently in clinical trials as an
immunosuppressant. - Cyclosporin A and tacrolimus are usually
administered in high doses with a transplant to
block acute rejection and then at lower doses for
maintenance.
21
Immunological effects of cyclosporin
A major advantage of this class of drugs is that
they do not target proliferating cells, and
therefore do not interfere with hematopoiesis (do
not cause anemia).
21
22
Patients needing a transplant outnumber the
available organs
- The success rates of transplant surgery have
improved remarkably, but growing shortages exist
in the supply of organs and tissues available for
transplantation. Many Americans who need
transplants cannot get them because of these
shortages. - 18 people die awaiting an organ transplant in the
United States every day. - The number of people in the U.S. waiting for an
organ transplant is over 100,000. - An estimated 14,000 people who die each year meet
the criteria for organ donation, but less than
half of that number become actual organ donors. - By signing a Uniform Donor Card, an individual
indicates his or her wish to be a donor.
23
Manipulations of the Immune Response(Chapter 16)
- Insufficient or misdirected and exaggerated
immune responses result in different
immunodeficiency and autoimmune diseases. - Immune system can be manipulated to the benefit
of patients - The main types of manipulations of the immune
system involve - 1. Vaccination
- 2. Inhibition of inflammation
- 3. Immuno-suppression during organ
transplantation - 4. Manipulations during cancer
24
Cancer and its interaction with the immune system
- Cancer is a diverse collection of
life-threatening diseases that are caused by
abnormal and invasive cell proliferation. - Cancer cells are very similar to normal cells,
and the immune system is unable to attack them
early and effectively. - Cancer results from mutations (changes in DNA)
that control cell growth. - The branch of medicine that deals with cancer is
called oncology.
25
Cancer Cells are Different
- Escape normal intercellular communication
- Allow for rapid growth
- Increased mobility of cells
- Invade tissues
- Metastasis
- Evade the immune system
26
During oncogenesis, some of the antigens on the
cancer cell surface change tumor antigens. Some
of these tumor antigens are shed from the cancer
cells. These shed antigens prompt action from
cytotoxic T cells, NK cells, and macrophages.
According to the theory of immune surveillance,
patrolling cells of the immune system provide
continuous surveillance, catching and eliminating
cells that undergo malignant transformation.
Tumors develop when this immune surveillance
breaks down or is overwhelmed.
26
27
Evidence for Tumor Immunity
- The high frequency of cancers in immunosuppressed
patients - Extremes of age
- Primary and secondary immunodeficiency
- Immunosuppressive drugs
- Tumors that are infiltrated by T cells and
monocytes have an improved prognosis - Spontaneous regression occurs
- Melanoma, breast, lung cancers
- Human tumors are immunogenic
- Tumors antigens have been defined
- Tumor specific T cells and antibodies are found
in cancer patients
28
Experimental Evidence for Tumor Antigens and
Immune Response
4. No tumor growth
2. Excise tumor
3. Re-challenge with same tumor
1. Inject Tumor
1. Inject Tumor
2. Excise tumor
3. Re-challenge with different tumor
4. Tumor grows
29
Nude mice cannot reject tumors and have been thus
used to test new anti-cancer therapies
- The nude mice have a dysfunctional immune system,
and can only live in a sterile environment. - They cannot reject any transplanted tissue,
including tumors. - Nude mice are very useful in cancer research
because injected human cancer cells can grow into
tumors allowing new ways to test cancer
therapies.
Nude mouse with transplanted rabbit skin
30
Tumors Benign vs. malignant
- Mass of abnormally proliferating cells is called
tumor ( swelling) or neoplasm ( new growth). - Benign Encapsulated tumors, localized and
limited in size - Tumors
- Malignant Invasive tumors, invading adjacent
tissues
Adenoma benign tumor of glandular tissue
31
Classification of tumors
- Tumors Primary the site of cancer origin
- Secondary the new tumors formed by metastasis
(cancer cells are carried by blood or lymph
to distant places) - Solid tumors Carcinomas - cancers of epithelial
cells (stomach, lung, breast prostate) 90
of all cancers - Sarcomas - cancers of all other cell types
(bones, muscles) very rare - Immune system cancers Leukemias cancers of
blood cells - Lymphomas cancers of lymphoid tissues
- Myelomas cancers of bone marrow
8 of all cancers
32
Ten Most Frequent Cancers in the United States
- Breast
- Prostate
- Lung
- Colon/rectum
- Lymphomas
- Bladder
- Uterus
- Skin
- Kidney
- Leukemias
33
A cancer arises from a single cell that has
accumulated multiple mutations
- The proper division of cells is controlled by
many mechanisms and multiple checkpoints ? the
control of cell division is never dependent on
only one protein cell must accumulate multiple
mutations in order to undergo malignant
transformation. - Cell division and malignant transformation are
controlled by two classes of genes
proto-oncogenes and tumor suppressor genes. - Proto-oncogenes are genes that regulate cell
division and proliferation. The mutant forms of
proto-oncogenes that contribute to malignant
transformation are called oncogenes. - Tumor suppressor genes encode proteins that
prevent malignant transformation. Loss of these
proteins results in malignant transformations and
cancer. One of the most important tumor
suppressor genes is p53, loss of which is
responsible for 50 of human cancers.
34
Proto-Oncogenes and Normal Cell Growth
Normal Growth-Control Pathway
Oncogenes are related to normal genes called
proto-oncogenes that encode components of the
cells normal growth-control pathway. Some of
these components are growth factors, receptors,
signaling enzymes, and transcription factors.
Growth factors bind to receptors on the cell
surface, which activate signaling enzymes inside
the cell that, in turn, activate transcription
factors inside the cells nucleus. The activated
transcription factors turn on the genes
required for cell growth and proliferation.
Growth factor
Receptor
Signaling enzymes
Transcriptionfactors
DNA
Cell nucleus
Cell proliferation
35
p53 Tumor Suppressor Protein Triggers Cell Suicide
p53 protein
Cell suicide (Apoptosis)
Normal cell
Excessive DNA damage
Normal cell
Cell suicide (Apoptosis)
Excessive DNA damage
One particular tumor suppressor gene codes for a
protein called p53 that can trigger apoptosis.
In cells that have undergone DNA damage, the p53
protein acts like a brake pedal to halt cell
growth and division. If the damage cannot be
repaired, the p53 protein eventually initiates
cell suicide, thereby preventing the genetically
damaged cell from growing out of control.
36
NFkB-dependent genes are involved in different
aspects of oncogenesis
- Recent evidence has accumulated from a large
variety of human malignancies indicating a role
for NFkB in promoting oncogenic conversion and in
facilitating later stage tumor properties such as
metastasis.
Oncogene 25 6817, 2006
37
Constitutive NFkB activation in human cancers
Oncogene 25 6817, 2006
38
Exposure to chemicals, radiation, and viruses can
facilitate the progression to cancer
- The number of mutations in the body can be
increased by mutagens, chemical and physical
agents that damage DNA. Mutagens that are known
to increase the risk of cancer are called
carcinogens. - Physical carcinogens (UV light, radiation)
usually induce extensive DNA mutations DNA
breaks and chromosome translocations. - Chemical carcinogens (asbestos, benzene, estrogen
therapy, tobacco products) usually induce single
nucleotide substitution in the proto-oncogenes
and tumor suppressor genes. - Oncogenic viruses and bacteria Certain viruses
and bacteria can also induce malignant
transformation viruses are associated with 15
of all human cancers. Some oncogenic viruses -
Papilloma virus, Epstein-Barr virus - bind to
p53, thus inactivating it and enabling the
virus-infected cell to proliferate. Bacterium
Helicobacter pylori is associated with
pathogenesis of stomach inflammation, ulcers, and
cancer.
39
Vaccine against HPV now available in the US
40
Cancer therapies
- Surgery
- Chemotherapy
- Radiation therapy
- Immunotherapy
- Types of immunotherapies include
- Cancer vaccines (active specific immunotherapies)
- Monoclonal antibody therapy (passive specific
immunotherapies) - Nonspecific immunotherapies (cytokines)
Classical New, emerging
41
Immunotherapies
- Cancer vaccines (Active Specific Immunotherapy)
- Contain cancer cells, parts of the cancer cells,
or pure tumor-associated antigens (antigens
expressed only on tumor cells but not on healthy
cells). - Induce production of tumor-specific antibodies
and stimulate killer CD8 T cells to attack the
cancer cells. - So far used only in clinical trials not approved
for general use. - Monoclonal Antibody Therapy (Passive Specific
Immunotherapy) - Monoclonal antibody therapy is a passive
immunotherapy because the antibodies against the
tumor-associated antigens are produced outside
the body (in the lab) rather than by the immune
system. This type of therapy can be effective
even if the immune system is weakened. - Approved for treatment of certain cancers (breast
cancer, leukemias). - Nonspecific Immunotherapies (Cytokines)
- Stimulate the immune system in a very general
way. - Interleukin-2 (IL-2) Stimulates the ability of
NK cells to kill the cancer cells. Used to treat
melanomas and kidney cancers. - Interferons Slow the growth of cancer cells
stimulate the cancer killing ability of NK cells.
Used to treat leukemias, lymphomas and melanoma.
42
Monoclonal antibodies (MAbs)
- Monoclonal antibodies are the most widely used
immunotherapy. - The first MAbs were made entirely from mouse
cells. One problem with this is that the human
immune system will see these antibodies as
foreign and then will mount a response against
them. This can cause allergic-type reactions. - Over time, researchers have learned how to
replace some parts of these mouse antibody
proteins with human parts. Depending on how much
of the MAb is human, these are called chimeric or
humanized antibodies they are likely to be safer
and more effective than older MAbs.
Chimeric Antibodies The variable regions of a
mouse antibody are expressed along with human
constant regions. This provides the antibody with
human effector functions. Humanized Antibodies
Only the HVR (CDR) regions from the rodent
antibody V-regions are combined with framework
regions from human V-regions. The idea is that
these antibodies should be more human-like than
chimeric and thus have fewer allergic responses.
42
43
Monoclonal antibodies used to treat cancer
MAb name Trade name Used to treat Approved in
rituximab Rituxan chronic lymphocytic leukemia 1997
trastuzumab Herceptin Breast, stomach cancer 1998
gemtuzumab Mylotarg acute myelogenous leukemia 2000
alemtuzumab Campath chronic lymphocytic leukemia 2001
ibritumomab tiuxetan Zevalin non-Hodgkin lymphoma 2002
tositumomab Bexxar non-Hodgkin lymphoma 2003
cetuximab Erbitux Colorectal, head neck cancers 2004
bevacizumab Avastin colorectal, lung, breast cancer 2004
panitumumab Vectibix colorectal cancer 2006
ofatumumab Arzerra chronic lymphocytic leukemia (CLL) 2009
denosumab Xgeva cancer spread to bone 2010
ipilimumab Yervoy melanoma 2011
43
44
Immunotherapy
Radioisotope
Herceptin
Growth factor
Herceptin blocks receptor
Antibody
Antigen
Breast cancer cell
Lymphoma cell
Lymphoma cell destroyed
Growth slows
A new approach to cancer therapy uses antibodies
that have been specially made to recognize
specific cancers. When coupled with natural
toxins, drugs, or radioactive substances, the
antibodies seek out their target cancer cells and
deliver their lethal load.
44
45
HPV Antibodies (Vaccines) Prevent Infection and
Cervical Cancer
- Human papillomavirus (HPV) is the most common
sexually transmitted virus in the United States.
At least 70 percent of sexually active persons
will be infected with HPV at some time in their
lives. HPV infects both men and women. - Over 99 percent of cervical cancer cases are
linked to long-term infections with high-risk
HPV. - The vaccination protects a person from future
infection by the high-risk HPV - After the vaccination, if an exposure occurs,
the vaccinated persons antibodies against the
HPV opsonize the virus and prevent it from
attachment to the host epithelial cells..
Papillomavirus
Antibodies
45
46
Cellular immunotherapy
46
47
Cancer Immunotherapy Dendritic Cells That
Attack Cancer
By modifying dendritic cells, researchers are
able to activate T cells that attack the cancer
cells. Because a tumor antigen alone is not
enough to result in a strong immune response,
cytokines are first fused to a tumor antigen with
the hope that this will send a strong antigenic
signal. Next, the patient's dendritic cells are
isolated and grown in the incubator to let them
take up this fused cytokine-tumor antigen. This
enables the dendritic cells to mature and
eventually display the same tumor antigens as
appear on the patient's cancer cells. When these
special mature dendritic cells are given back to
the patient, they present their newly acquired
tumor antigens to the T cells that can respond
and attack the patient's cancer cells.
Dendrion FDA approval for prostate cancer
treatment
47
48
Cancer and diet
- Almost 25 centuries ago, Hippocrates remarked
Let food be the medicine and medicine be the
food. - About 1/3 of the cancer deaths in the US each
year are due to nutrition factors, including
obesity. (ACS) - For most Americans who do not smoke, dietary
choices and physical activity become the most
important determinants of cancer risk. (ACS) - Populations with higher consumptions of fruits
and vegetables have lower incidence of
gastrointestinal and respiratory tract cancers. - Consumption of meat, especially red meat, has
been associated with increased cancer risk at
several sites, most notably colon and prostate.
(ACS)
49
Cancer and diet Broccoli
- Broccoli contains certain chemicals that may
reduce the risk of colorectal, breast, prostate
and other cancers. Broccoli belongs to the
cabbage and mustard families, which also includes
cauliflower, radishes, and brussels sprouts. - Broccoli is a good source of many phytochemicals
(chemicals from plants) that may have anti-cancer
properties. For example, broccoli contains
several compounds called isothiocyanates,
including sulforaphane and indole-3-carbinol
(I3C), which have been suggested as possible
anti-cancer agents in recent years. Early studies
have shown these substances may act as
antioxidants and may boost detoxifying enzymes in
the body. Some studies have also suggested they
may alter body estrogen levels, which might
affect breast cancer risk.
50
Cancer and spices
- Most agents derived from spices have antioxidant
and anti-inflammatory activities. The antioxidant
activities of these dietary spices suggest that,
besides imparting flavor to foods, they possess
potential health benefits. - Recent research has also shown that many spices
(curcumin - curry, garlic, capsaicin - hot chili
pepper) inhibit activation of the transcription
factor NFkB, which regulates transcription of
anti-apoptotic ( pro-survival) genes. Thus,
these spices can induce apoptosis, and have
anti-tumor properties.
51
Mechanism of NFkB inhibition in cancer
- Curcumin (curry)
- Capsaicin (hot chili peppers)
- Garlic
Anti-apoptotic (pro-survival) genes, cell growth
regulating genes