Indications for IVOX Insertion PowerPoint PPT Presentation
1 / 38
Title: Indications for IVOX Insertion
1
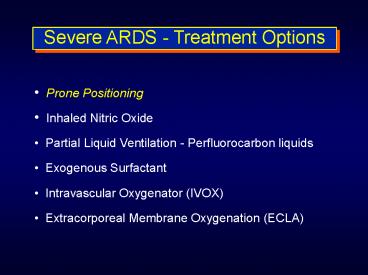
Severe ARDS - Treatment Options
- Prone Positioning
- Inhaled Nitric Oxide
- Partial Liquid Ventilation - Perfluorocarbon
liquids - Exogenous Surfactant
- Intravascular Oxygenator (IVOX)
- Extracorporeal Membrane Oxygenation (ECLA)
2
CT Imaging Prior to Prone Position
3
Prone Positioning
4
Prone Positioning
5
Prone Positioning in ModeratePost-traumatic Lung
Injury
- 22 blunt trauma patients (11 ALI, 11 ARDS)
- Pressure-limited (APRV, Drager), IE 11, PEEP
8-16 - Prone position for 8 hours q day
- Indications for prone positioning
- FiO2 gt 0.5 with PEEP gt 10cm H2O for gt 24 hours
- Pulmonary densities in 2 or more quadrants on CT
that were constant or increasing within 48 hours. - HRCT scan before 1st and after last cycle prone
- ABG q 2 hours Qs/Qt evaluated
Voggenreiter G, et al. Crit Care Med
199927(11)2375-2382
6
Prone Positioning in ModeratePost-traumatic Lung
Injury
- Position change done manually (3-4 staff members)
- Air flow mattresses (not Stryker frame)
- FiO2 and PEEP decreased to target paO2 70-80
- Therapeutic bronchoscopy at end of each prone
position cycle for mobilized secretions - Termination of Prone positioning when
- FiO2 lt 0.3
- PaO2 difference from prone to supine of lt 15 torr
- Decrease in pulmonary densities to lt 10 total
lung volume validated by CT
Voggenreiter G, et al. Crit Care Med
199927(11)2375-2382
7
Prone Positioning in ModeratePost-traumatic Lung
Injury
Voggenreiter G, et al. Crit Care Med
199927(11)2375-2382
8
Prone Positioning in ModeratePost-traumatic Lung
Injury
Voggenreiter G, et al. Crit Care Med
199927(11)2375-2382
9
Prone Positioning in ModeratePost-traumatic Lung
Injury
Conclusion Repeated prone positioning recruits
collapsed lung tissue and improves gas exchange
in trauma patients with blunt chest trauma and
severe ARDS as well as in trauma patients with
acute lung injury.
Voggenreiter G, et al. Crit Care Med
199927(11)2375-2382
10
(No Transcript)
11
FiO2
P/F Ratio
SvO2
PEEP
12
Severe ARDS - Treatment Options
Prone Positioning Inhaled Nitric Oxide
Partial Liquid Ventilation - Perfluorocarbon
liquids Exogenous Surfactant Intravascular
Oxygenator (IVOX) Extracorporeal Membrane
Oxygenation (ECLA)
13
Inhaled Nitric Oxide
Selective pulmonary vasodilator Decreased
mean PAP and PVR Improves intrapulmonary
shunt Improves oxygenation Dosage 5 to
40 ppm continuously Problems Safe delivery
of inhaled NO (monitoring, safety standards)
Interruption for minutes may lead to severe
hypoxemia Inhaled NO is effective in only a
subgroup of ARDS pts Difficulty in withdrawal
of NO in chronic pts Unclear whether inhaled
NO reduces morbidity, mortality
14
Inhaled Nitric Oxide
Effects of inhaled NO in patients with ARDS
results of a randomized phase II trial.
OBJECTIVE To evaluate the safety and
physiologic response of inhaled nitric oxide (NO)
in ARDS. DESIGN Prospective, multicenter,
randomized, double-blind, placebo-controlled
study in ICUs of 30 US hospitals PATIENTS
Patients with ARDS, as defined by the
American-European Consensus Conference, were
enrolled into the study if the onset of disease
was within 72 hrs of randomization.
Inhaled Nitric Oxide in ARDS Study
Group Dellinger RP et al., Crit Care Med 1998
Jan26(1)15-23
15
Inhaled Nitric Oxide
- INTERVENTION Placebo (nitrogen gas) or
inhaled NO at 1.25, 5, 20, 40, or 80 ppm. - 177 patients were enrolled over 14-months.
- Acute response to treatment gas, defined as a
PaO2 increase ? 20 - occurred in 60 of NO patients (no significant
differences between dose groups) - occurred in 24 of placebo patients
- No differences in mortality rate, the number of
days alive and off MV, or the number of days
alive after meeting oxygenation criteria for
extubation.
16
Inhaled Nitric Oxide
In a post-hoc analysis, the percentage of
patients alive and off mechanical ventilation at
day 28 was higher (62 vs. 44) in the NO 5ppm
group than the placebo group. CONCLUSIONS
Inhaled NO is well tolerated in ARDS patients
and is associated with a significant improvement
in oxygenation compared with placebo over the
first 4 hrs of treatment. Larger phase III
studies are needed to ascertain if these acute
physiologic improvements can lead to altered
clinical outcome.
17
Low-dose inhaled nitric oxide in patients with
ALI a randomized controlled trial
- Multicenter, randomized, placebo-controlled study
in 46 ICUs in US (3/96-9/99) - Blinding of patients, caregivers, data
collectors, outcome assessors, and data analysts
(triple blind) - Patients (n 385) with moderately severe ALI, a
modification of the American-European Consensus
Conference definition of ARDS (PaO2/FiO2 ratio
lt250) were enrolled if - the onset was within 72 hours of randomization
- sepsis was not the cause of the lung injury
- the patient had no significant non-pulmonary
organ system dysfunction at randomization.
Taylor RW and Inhaled NO in ARDS Study
Group JAMA. 2004 Apr 7291(13)1603-9.
18
Low-dose inhaled nitric oxide in patients with
ALI a randomized controlled trial
- INTERVENTION placebo (nitrogen gas) or inhaled
NO at 5 ppm until 28 days, discontinuation of
assisted breathing, or death. - RESULTS Inhaled NO did not increase the number
of days alive and off assisted breathing (mean
SD, 10.6 9.8 days placebo and 10.7 9.7 days
NO P .97 - Statistically significant increase in PaO2 -
resolved by 48 hours - Mortality unchanged (20 placebo vs 23 NO P
.54) - Days alive after a successful 2-hr unassisted
ventilation trial mean (SD) 11.9 (9.9) for
placebo and 11.4 (9.8) NO (P .54) - Days alive and meeting criteria for extubation
17.0 placebo vs 16.7 NO (P .89)
Taylor RW and Inhaled NO in ARDS Study
Group JAMA. 2004 Apr 7291(13)1603-9.
19
Low-dose inhaled nitric oxide in patients with
ALI a randomized controlled trial.
- CONCLUSION
- Inhaled nitric oxide at a dose of 5 ppm in
patients with acute lung injury - not due to sepsis and
- without evidence of non-pulmonary organ system
dysfunction - Results in short-term oxygenation improvements
but has no substantial impact on the duration of
ventilatory support or mortality.
Taylor RW and Inhaled NO in ARDS Study
Group JAMA. 2004 Apr 7291(13)1603-9.
20
Inhaled Nitric Oxide
Inability to translate physiologic benefit
(improvement in oxygenation) to clinical
outcome benefit in adult clinical trials.
21
Severe ARDS - Treatment Options
Prone Positioning Inhaled Nitric Oxide
Partial Liquid Ventilation - Perfluorocarbon
liquids Exogenous Surfactant Intravascular
Oxygenator (IVOX) Extracorporeal Membrane
Oxygenation (ECLA)
22
Surfactant Dysfunction in Adult ARDS
While surfactant dysfunction may not be the
primary pathogenic factor in ARDS, surfactant
dysfunction is integral to the pathophysiologic
changes that occur.
23
Pathophysiology of ARDS
Alveolar-capillary Membrane damage
Increased Permeability
Type II cell injury
Surfactant dysfunction
Pulmonary Edema
Intrapulmonary Shunt
Decreased Compliance
Decreased FRC
24
Surfactant Production and Recycling in the Normal
Alveolus
Baudouin, S. V. N Engl J Med 2004351853-855
25
Surfactant Production and Recycling in Acute Lung
Injury
Baudouin, S. V. N Engl J Med 2004351853-855
26
Exogenous Surfactant - Pediatrics
- News 07/26/1989
- Treatment IND for Surfactant P89-35
- FOOD AND DRUG ADMINISTRATION FOR IMMEDIATE
RELEASE - The FDA today authorized wide use of an
experimental drug for the inside of the lungs to
save thousands of premature infants born with a
breathing difficulty called Respiratory Distress
Syndrome. The syndrome is caused when the
immature lungs of a premature infant are not yet
producing a naturally occurring surfactant -- a
foamy substance that coats the inside of the
lungs and keeps them from collapsing when the
infant exhales.
27
Exosurf - Adult Studies
- Protocol 14 evaluated efficacy of Exosurf in
sepsis-induced ARDS at higher doses Exosurf 3X
and Exosurf 6X aerosolized at room temp for 24
hrs/day. - 49 patients evaluated
- Mortality was significantly decreased
- Although shunt fraction was only slightly
improved in the Exosurf groups, the PAO2-PaO2
showed marked improvement in both Exosurf groups.
28
Exosurf - Adult Studies
- Multicenter, double-blind, placebo-controlled
study in patients with ARDS due to sepsis. - 52 patients, comparing Exosurf 12 hours per
day, Exosurf 24 hours per day and 0.1 N saline. - Small decrease in shunt fraction and small
improvement in dynamic and static respiratory
compliance noted in Exosurf group. - Mortality was significantly decreased
29
Exosurf - Adult Studies
- An International Multicenter Randomized,
Placebo-Controlled Study of the Effect of
Continuous Administration of Aerosolized Exosurf
in Patients with Sepsis-Induced ARDS. - Patients will be randomized to aerosolized
placebo (0.45 saline) or aerosolized Exosurf 1X
(13.5 mg colfoxceril palmitate per ml)
continuously for 5 days duration. - Hypothesis treatment of patients with ARDS
due to sepsis with aerosolized Exosurf reduces
mortality at 30 days.
30
(No Transcript)
31
(No Transcript)
32
Exosurf - Adult Studies
725 patients, stratified by APACHE III 364
pts. Exosurf, 361 pts 0.45 saline aerosol
Survival at 30 days was 60 for both groups.
Increased secretions in Exosurf group.
Complications similar for both groups. Conclusion
The continuous administration of aerosolized
synthetic surfactant to patients with
sepsis-induced ARDS had no significant effect on
30-day survival, length of stay in the ICU,
duration of mechanical ventilation, or
physiologic function.
Anzueto et al. NEJM 334(22)1417, May 1996.
33
Surfactant types available
- Modified bovine surfactant
- Berectant, Survanta
- Porcine surfactant
- Curosurf
- Synthetic Surfactants
- Exosurf, includes cetyl alcohol tyloxapol
- Next generation
- DPPC (dipalmitoylphosphatidyl choline) plus
surfactant proteins (A,B,C) from recombinant DNA
technology.
34
North American Study n 221 European and
South African study n 227 Mean PaO2FiO2
Ratio 130-137
35
Protein C-based Surfactant and ARDS
57 were sepsis-associated ARDS patients Among
pts with direct ARDS, Surfactant was associated
with higher survival
36
Protein C-based Surfactant and ARDS
37
Surfactant Therapy in ARDS
- Biologically plausible hypothesis should
work! - Replacement surfactants differ from human
- Lack of important surfactant proteins
- Concentration of surfactant achieved in damaged
alveoli is unknown - Proper delivery method?
- Preferential deposition of surfactant in normal
alveoli - ARDS due to direct lung injury vs. indirect
- Death is the wrong outcome measure
38
VALID Study
- Lung surfactant factor (LSF) Venticute
- Intratracheal instillation
- Phase III P, R, D-B Clinical Trial
- ALI from pneumonia or aspiration
- ARDSNet ventilation protocol
- Outcome 28-day mortality
- N 1200 expected enrollment (n550)
- Study start November 2003
- ALTANA Pharma
- NCT00074906
39
ReviewPharmacologic therapies for adults with
acute lung injury and acute respiratory distress
syndrome
- Randomized controlled trials of pharmacologic
treatment compared to no therapy or placebo in
adults with established ALI or ARDS - Thirty three trials randomizing 3272 adult
patients - PGE1, N-acetylcysteine, pentoxifylline, early or
late corticosteroids, surfactant - Conclusion
- Effective pharmacotherapy for ALI and ARDS is
extremely limited, with insufficient evidence to
support any specific intervention
N Adhikari, KEA Burns, MO Meade The Cochrane
Database of Systematic Reviews 2005, Issue 3