Spinal Abscess. Why Care - PowerPoint PPT Presentation
1 / 22
Title:
Spinal Abscess. Why Care
Description:
... pain radiating down to the legs, respectively. ... Legs are diffusely weak, 3/5 proximally and 4/5 distally. ... Both legs are very weak diffusely (2/5) ... – PowerPoint PPT presentation
Number of Views:87
Avg rating:3.0/5.0
Title: Spinal Abscess. Why Care
1
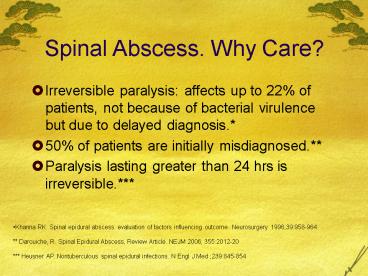
Spinal Abscess. Why Care?
- Irreversible paralysis affects up to 22 of
patients, not because of bacterial virulence but
due to delayed diagnosis. - 50 of patients are initially misdiagnosed.
- Paralysis lasting greater than 24 hrs is
irreversible.
- Khanna RK. Spinal epidural abscess evaluation of
factors influencing outcome. Neurosurgery
199639958-964. - Darouiche, R. Spinal Epidural Abscess, Review
Article. NEJM 2006 3552012-20 - Heusner AP. Nontuberculous spinal epidural
infections. N Engl J Med 239845-854
2
Epidural Abscess
- Classic description is focal vertebral pain,
which becomes radiating pain along involved nerve
roots. - Most commonly involves the thoracic spine (50-80
of cases) lumbar in 17-38 and the cervical
spine in 10-25 of cases. - Spinal epidural abscess most often occurs by
systematic hematogenous spread of the infectious
organism. - A spinal epidural abscess can less commonly occur
by direct infection of the epidural space as with
a catheter or needle. (eg. Lumbar Puncture)
3
Distribution of Spinal Abscess
The larger posterior epidural space contains
more infection-prone fat (than anterior).
Therefore, they are more in posterior space.
Rigamonti D, Liem L, Sampath P, et al. Spinal
epidural abscess contemporary trends in
etiology, evaluation, and management. Surg Neurol
199952189-197.
4
Intramedullary (located within the spinal cord)
Leptomeningeal (subarachnoid space. Hence,
extramedullary and intradural)
Paravertebral
Epidural
Epidural
Byrne T. Spinal cord compression from epidural
metastases. N Engl J Med 1992327614
5
Axial T2-weighted magnetic resonance imaging of
Staphylococcus aureus L2 epidural abscess
impinging the dorsolateral aspect of the spinal
canal. Marx Rosens Emergency Medicine
Concepts and Clinical Practice, 6th ED .
6
Predisposing factors
- Trauma, prior surgery, or spinal procedures.
- Immunocompromised states
- Pregnancy
- Diabetes mellitus (Type I or II)
- Bacteremia (endocarditis, lung or abdominal
abscess, or previous septic episodes) - Osteomyelitis
- IV drug use
- Alcoholism
- Chronic renal failure
7
Epidemiology
- 20 patients per 100,000 hospital admissions.
- Age injection drug users)
- Men Women
8
Buggs
MRSA 15 in 1995, now up to 40 in 2006.
9
Diagnosis
- Classic Triad
Fever
Spine pain
Neurological deficit
10
Diagnosis
- Incontinence of bowel/bladder.
- Weakness / numbness below the level of the lesion.
11
(No Transcript)
12
Diagnosis
- Nuchal rigidity suggesting the presence of
meningeal irritation. - Four clinical stages of spinal epidural abscess
- onset of focal vertebral pain.
- radiation of the pain along regionally involved
nerve roots suggesting a radicular component. - evidence of spinal cord compression with long
tract signs. - paralysis below the level of the spinal cord
lesion.
13
Differential Diagnosis
- Spinal Radiculopathy / polyradiculopathy
- Herniated Disk
- Bacterial meningitis.
- Osteomyelitis
- Spinal tumor / spinal hematoma.
- Multiple Sclerosis
- Spinal cord infraction
14
Pitfalls in diagnosis
- Stage 2 nerve-root pain radiating from involved
spinal area. (no motor weakness or sensory
deficit at this point) - Cervical or lumbar abscess neck pain radiating
to the arms or low back pain radiating down to
the legs, respectively. - Thoracic abscess chest or abdominal pain.
Bremer AA, Darouiche RO. Spinal epidural abscess
presenting as intra-abdominal pathology a case
report and literature review. J Emerg Med
20042651-56
15
Pitfalls in Diagnosis
Reihsaus E, Waldbaur H, Seeling W. Spinal
epidural abscess a meta-analysis of 915
patients. Neurosurg Rev 200023175-204.
16
Treatment
- Neurosurgical consultation for possible
decompression. - Empiric antibiotics Nafcillin or Vancomycin
(both for S. aureus) along with Ceftriaxone
(Gram-negative) and Metronidazole (anaerobic
organisms). - 4 weeks course if osteomyelitis is not present.
- and 8 weeks for osteo is present
17
Darouiche, R. Spinal Epidural Abscess, Review
Article. NEJM 2006 3552012-20
18
(No Transcript)
19
Outcomes
Chao D, Nanda A. Spinal epidural abscess a
diagnostic challenge. Am Fam Physician
2002651341-6
20
- 64yo woman is evaluated in the ED for 4 day hx
of progressive leg weakness and numbness and a 1
day hx of urinary incontinence. She also had
increasingly severe midback pain for the past 2
months. She has a history of breast cancer
diagnosed 2 years ago, treated with surgery and
local radiation therapy. Her only medication is
tamoxifen. - Physical exam shows normal mental status and
cranial nerves. Strength in the arms is normal.
Legs are diffusely weak, 3/5 proximally and 4/5
distally. Sensory exam shows diminished pin
sensation from the nipple downward vibratory
sense is severely diminished in the feet.
Reflexes are 2 in the biceps and triceps and 3
in the knees and ankles. An extensor plantar
response is present bilaterlly. Anal sphincter
tone is deministed. - Which of the following is the most appropriate
diagnostic study at this time? - CT of lumbar spine
- Electromyography and nerve conduction studies
- MRI of brain
- MRI of the entire spine
- Plain radiographs of the entire spine
21
- 32yo woman is evaluated in the ED for 2 day hx
of progressive numbness and weakness in the legs
she has also noted urinary incontinence since
awakening this morning. She has no significant
medical history and has not had recent infections
or vaccinations. - Physical exam shows normal mental status and
cranial nerves. Strength is normal in the arms.
Both legs are very weak diffusely (2/5).
Sensation to pinprick is diminished from the
umbilicus down, and vibratory sensation is
diminished in the toes. Reflexes are 2 in the
biceps and triceps, 3 in the knees and ankles,
with a bilateral extensor plantar response.
Sagittal MRO of the spinal cord shows an
enchancing lesion within the spinal cord, with
edema, extending from the T8 to T10 level. - Which of the following is the most appropriate
initial management of this patient? - Intramuscular interferon-beta
- Intravenous acyclovir
- Intravenous methylprednisolone
- Neurological decompenssion
- Oral prednisone
10
22
- 82yo woman is brought to the ED after the sudden
onset of bilateral leg weakness that occurred
while she was gardening this morning. She has a
hx of hypertension and peripherial vascular
disease. - Physical exam shows mental status and cranial
nerves. Upper extremity strength is normal, but
lower extremities are both severely weak (0/5).
Sensation to pinprick is diminished from the T8
level down vibration and proprioception are
normal. Reflexes are 1 and symmetric in the
upper and lower extremities an extenor plantar
response is present bilaterally. - Which of the following is the most likely
diagnosis? - Cauda equina compression
- Cerebellar hemorhage
- Pontine hemorrhage
- Spinal cord infarction
37