Case 11 PowerPoint PPT Presentation
1 / 19
Title: Case 11
1
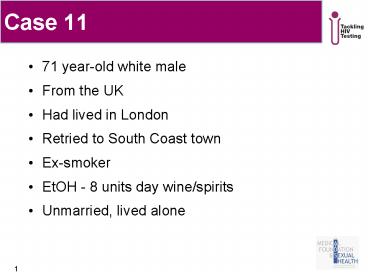
Case 11
- 71 year-old white male
- From the UK
- Had lived in London
- Retried to South Coast town
- Ex-smoker
- EtOH - 8 units day wine/spirits
- Unmarried, lived alone
2
Case 11 June 2006
- Admitted via Ophthalmology with
- Probable HIV-related peripheral neuropathy
- Probable Pneumocystis jirovecii pneumonia
- CMV retinitis
- Sexual history
- Friend long-term male partner
- no UPAI 15 years
- Initial investigations
- BAL confirmed PCP
- CD4 7 VL 200,000
3
Case 11 PMH
- 2000 Seen in Haematology for persisting
lymphopenia - 2000 Admitted with weight loss, watery diarrhoea
- 2001 Admitted with cerebellar infarct
- 2001 Seen in Neurology OPD (3 in London, 1
elsewhere) - for peripheral neuropathy - unknown cause
- 2003 Admitted with weight loss, OGD
oesophaghitis - 2004 Admitted with fractured right neck of femur
- lymphocytes 0.5 (1.3-3.5)
- multiple mouth ulcers
- candida on mouth swab
- 2005 Recurrent LRTIs throughout 2005
4
Case 11 June 2006
- Seen in Ophthalmology OPD
- vitreous detachment in left eye
- 2/12 history of acute onset unilateral cloudy
vision - OE
- retinal necrosis
- features characteristic of CMV retinitis
- SOB
- Refractory to antibiotics from GP
- Admitted to hospital
5
Case 11 June 2006
- Management
- Left vitrectomy and intraocular foscarnet
- D/w Genitourinary Medicine team
- What is the current treatment for
non-HIV-related CMV retinitis? - GUM team
- Could this be HIV-related?
- Investigations
- Rapid strip HIV test reactive
- Confirmatory 4th generation HIV test positive
6
Case 11 June 2006
- Further management
- CMV retinitis
- Intraocular foscarnet
- Initiated on Valgancyclovir 900mg po bd
- 21/7 ?maintenance
- PCP
- treated empirically with Co-trimoxazole, dose
120mg/kg bd - 21/7 ?prophylaxis
- HIV-related neuropathy
- Prednisolone 60mg po od
- Antiretroviral therapy initiated
7
Case 11 June 2006
- 1 day prior to planned discharge
- Septicaemic shock
- Died despite
- vigorous fluid resuscitation
- broad spectrum antibiotic cover
- ITU admission
- ventilatory support
- maximal inotropic support
- Blood cultures grew Klebsiella terrigena
- Cause of death
- 1a gram negative sepsis
- 1b multi organ failure
- 1c immunosupression 2HIV
8
Case 11 summary
- 2000 Haematology OPD, persisting lymphopenia
- 2000 Gen. med. admission, watery diarrhoea,
weight loss - 2001 General medical admission, cerebellar
infarct - 2001 Neurology OPD, peripheral neuropathy -
unknown cause - 2003 Gen. med. admission, weight loss - OGD
oesophagitis - 2004 Fracture NOF, low lymphocytes, oral
candida - recorded in ED notes lives with male
partner - 2005 General medical admission, LRTI low
lymphocytes - 2006 Ophthalmology OPD non-HIV related CMV
retinitis - 2006 HIV diagnosed PCP CD4 7 VL 200,000
9
Q At which of his healthcare interactions could
HIV testing have been undertaken?
- When he was seen with persistent lymphopenia?
(2000) - When he was admitted with watery diarrhoea?
(2000) - When he was admitted with cerebellar infarct?
(2001) - When he was seen for peripheral neuropathy?
(2001) - When he was admitted with weight loss and
oesophagitis? (2003) - When he was admitted with a fracture and
disclosed living with male partner? (2004) - When he was admitted with recurrent LRTI? (2005)
- When he was seen for non-HIV-related CMV
retinitis? (2006)
10
Who can test?
11
Who to test?
12
Rates of HIV-infected persons accessing HIV care
by area of residence, 2007
Source Health Protection Agency, www.hpa.org.uk
13
Who to test?
14
Who to test?
15
Who to test?
16
8 missed opportunities 5 in ED - to diagnose
HIV before terminal presentation! If current
guidelines used, HIV could have been diagnosed 6
years earlier
- 2000 Haematology OPD, persisting lymphopenia
- 2000 Gen. med. admission, watery diarrhoea,
weight loss - 2001 General medical admission, cerebellar
infarct - 2001 Neurology OPD, peripheral neuropathy -
unknown cause - 2003 Gen. med. admission, weight loss - OGD
oesophagitis - 2004 Fracture NOF, low lymphocytes, oral
candida - recorded in ED notes lives with male
partner - 2005 General medical admission, LRTI low
lymphocytes - 2006 Ophthalmology OPD non-HIV related CMV
retinitis - 2006 HIV diagnosed PCP CD4 7 VL 200,000
17
Learning Points
- This patient had numerous investigations and 5
admissions over 6 years, causing him much
distress and costing the NHS thousands of pounds - Some patients might not disclose risk factors for
HIV on routine questioning in Outpatients even if
the right questions are asked - Because of this the otherwise excellent medical
teams looking after him did not think of HIV even
when the diagnosis seems obvious with hindsight - A perceived lack of risk should not deter you
from offering a test when clinically indicated
18
Key messages
- Antiretroviral therapy (ART) has transformed
treatment of HIV infection - The benefits of early diagnosis of HIV are well
recognised - not offering HIV testing represents
a missed opportunity - UK guidelines recommend universal HIV testing for
patients from groups at higher risk of HIV
infection - UK guidelines recommend screening for HIV in
adult populations where undiagnosed prevalence is
gt1/1000 as it has been shown to be cost-effective - HIV screening should become a routine test on
presentation of lymphopenia, PUO, chronic
diarrhoea and weight loss of otherwise unknown
cause
19
Also contains UK National Guidelines for HIV
Testing 2008 from BASHH/BHIVA/BIS
Available from enquiries_at_medfash.bma.org.uk or
020 7383 6345