ENT teaching 23108 programme PowerPoint PPT Presentation
1 / 114
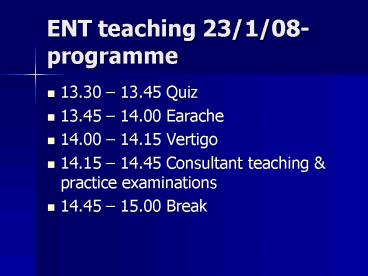
Title: ENT teaching 23108 programme
1
ENT teaching 23/1/08- programme
- 13.30 13.45 Quiz
- 13.45 14.00 Earache
- 14.00 14.15 Vertigo
- 14.15 14.45 Consultant teaching practice
examinations - 14.45 15.00 Break
2
Programme (cont)
- 15.00 15.15 Rhinitis
- 15.15 15.30 Sinusitis
- 15.30 15.45 Sore throat
- 15.45 16.00 Case study
- 16.00 16.30 Quiz answers (with prize!)
feedback
3
Curriculum coverage 1
- Symptoms
- Catarrh
- Discharging ear
- Dizziness
- Facial pain
- Otalgia
- Sore throat
4
Curriculum coverage 2
- Conditions
- Otitis externa
- Pharyngitis, tonsillitis, glandular fever
- Rhinitis (infective and allergic)
- Sinusitis (infective and allergic)
- Vertigo and Ménières Disease
5
Curriculum coverage 3
- Investigation/Psychomotor skills
- Otoscopy
- Tuning fork tests
- Throat and neck examination
- Treatment
- Watchful waiting and use of delayed prescriptions
6
Curriculum coverage 4
- Emergencies
- Tonsilitis with quinsy
- Otitis externa if extremely blocked or painful
mastoiditis - Prevention
- Awareness of iatrogenic causes of ototoxicity
7
Earache
- ENT teaching session
8
Case History
- A 59-year-old female with a 2 week history of
bilateral ear pain and discharge. - Her previous medical history included COPD, a
hysterectomy for menorrhagia, and early OA in her
right hip. - She had no history of diabetes or
immunosuppressed states. - Otoscopy
- Left erythematous, tender, with scant mucoid
discharge and no granulations. Left tympanic
membrane appeared intact and normal - Right erythematous, swollen, and tender with
abundant mucoid discharge, and wax. Right
tympanic membrane was not fully visualised due to
swelling
9
What do you think?
- What else do you want to know?
- Are you going to do anything?
- What features would worry you?
10
Normal TM - ant. plica (AP), post. plica (PP).
pars flaccida (PF)
Umbo (Um), handle of malleus (HM), lateral
process of malleus (Lpm)
Pars tensa (PT), light reflex (LR), fibrous ring
(FR),
11
Acute otitis externa
12
Chronic Otitis Externa
13
Historical features
- Otalgia ranging from mild to severe
- Hearing loss
- Ear fullness or pressure
- Tinnitus
- Fever (occasionally)
- Ear discharge
- Itch (esp. in fungal infections or chronic OE)
- Severe deep pain (If experienced by a patient who
is immunocompromised or diabetic, be alerted to
the possibility of malignant OE.)
14
Hypothesis testing from differentials
- Otitis Externa
- Otitis Media Otitis media with a perforation or
ventilation tube present - Ear canal traumaEar canal foreign bodyEar canal
carcinoma
15
Is it otitis externa?
- Otitis media is very common in children. It is
unusual in adults. - Pain on palpation of the tragus (anterior to ear
canal) or when applying traction to the pinna
(hallmark of OE) - Oedema and redness of the ear canal
- Purulent or serous discharge in the ear canal
- Conductive hearing loss
16
Is it otitis externa?
- More worrying.
- Cellulitis of the face or neck or ipsilateral
cervical lymphadenopathy (in some patients) - Fungal OE
- Fungal infections result in severe itch but less
pain than bacterial OE. - A thick discharge that may be white or gray often
is present. - On close examination, the discharge may have
visible fungal elements or a fuzzy appearance. - Malignant (necrotising) otitis externa
- Characteristic feature of malignant OE is pain
out of proportion to clinical findings. - On close examination, granulation tissue may be
present in the ear canal.
17
Acute Otitis Externa
- Infection of the skin of the cartilaginous
portion of the ear canal. - Contributing factors include moisture, canal
occlusion, local trauma, and allergy - Cause a loss of protective wax layer, causing
oedema of the squamous epithelium with plugging
of the glandular secretory ducts. - Consequent scratching induces local trauma,
allowing bacteria to invade through the skin,
leading to inflammation and production of
exudate. - The pathogens in acute otitis externa are
- pseudomonas (41),
- peptostreptococcus (22),
- Staph. aureus (15),
- Bacteroides (11)
18
What are the effects of empirical treatment for
otitis externa?
- Likely to be beneficial
- Topical aluminium acetate drops (as effective as
topical antibiotics) - Topical antibacterials (with or without steroids)
- Topical steroids
- Unknown effectiveness
- Oral antibiotics
- Specialist aural toilet
- Topical acetic acid (insufficient evidence to
demonstrate effectiveness compared with placebo) - Topical antifungals (with or without steroids)
- Unlikely to be beneficial
- Oral antibiotics plus topical anti-infective
agents (no better than topical anti-infective
agents alone) - BMJ Clinical Evidence Sep 2006
19
Case History
- Acute otitis externa as presumptive diagnosis,
treated with mixed antibiotic drops. Asked to
return if no better in a week, and practice nurse
to perform aural toilet - Returns 2 weeks later
- Treated with NEOMYCIN, POLYMYXIN B, AND
HYDROCORTISONE drops without benefit. Pain
continues, though slightly reduced - Otoscopy - swelling in right ear reduced.
Granulation tissue present at the right
cartilaginous/bony junction posteriorly. - Blood tests are done and a swab of the exudative
region is performed. - Findings - slightly elevated WBC of 12.7, a
greatly elevated ESR of 92, and a normal fasting
blood glucose. - What would you do next?
20
(No Transcript)
21
Case History
- REFER to ENT urgently
- Patient was admitted to hospital
- Diagnosis of malignant otitis externa
- Her ears were debrided and cultures were sent,
which eventually grew Pseudomonas aeruginosa. - A CT scan done on admission showed soft tissue
thickening around the ear canals, but was
otherwise normal. - A technetium bone scan was negative, and a
gallium scan was positive for bilateral temporal
inflammation.
22
Case History
- The patient was placed on ciprofloxacin IV and
gentamicin drops. - Her ear canals were regularly debrided.
- Blood glucose checks were all normal.
- After 10 days, her ear canals had no granulation
tissue or discharge, and she was discharged to
home on ciprofloxacin. - In follow-up, she has been seen in at 2 weeks and
4 weeks post-discharge by ENT and had no
recurrence. She continued to take ciprofloxacin
long term.
23
Malignant otitis externa
- The disease starts in the external auditory canal
and spreads to adjacent soft tissue, cartilage
and bone. - Although there is often a pre-existing otitis
externa, progression to invasive disease is
usually rapid - The pathognomonic sign is the presence of active
granulation tissue in the external auditory canal
at bone junction or cartilaginous portion
24
Malignant otitis externa
- Malignant otitis externa, a potentially lethal
infection, is considered to be a complication of
otitis externa. It can lead to cranial nerve
palsies, and intracranial complications. - It occurs primarily in elderly persons who have
diabetes mellitus or other predisposing factors
such as immunosuppression due to chemotherapy,
steroid administration or HIV
25
Malignant otitis externa
- Look for signs and symptoms indicating that the
process extends beyond the external auditory
canal. - Consider if persistent otitis externa, refractory
to usual management, with severe pain - Microbacterial culture should be performed before
initiating systemic antibiotic therapy, in high
risk patients. This will avoid the growth of
resistant pathogens. - If the ear canal is obstructed, insert a wick or
provide aural toilet - If suspected treat aggressively with oral
antibiotics, review within a week, and if no
improvement refer the patient to ENT.
26
Prevention
- Some patients acquire otitis externa (OE)
multiple times and should use a preventive
strategy. - Earplugs worn for swimming and bathing are
effective. Wipe earplugs with alcohol after use. - Avoid damage to ear canal, and avoid cotton buds
- Keep your ears dry and clean protect ears from
water - Consider drying ears with a hairdryer, on a low
heat - If you swim regularly, wear a swimming hat that
covers your ears, or use ear plugs. - Treat and prevent other skin conditions to
reduce trauma due to itch
27
AAO Acute OE Guidelines 2006
- 1a. Differential Diagnosis distinguish diffuse
acute otitis externa (AOE) from otalgia,
otorrhea, and inflammation of the external ear
canal. (evidence quality C and D) - 1b. Modifying Factors assess the patient with
diffuse AOE for risk factors that modify
management (nonintact tympanic membrane,
tympanostomy tube, diabetes, immunocompromised
state, prior radiotherapy). (evidence quality C) - 2. Pain Management Primary importance (evidence
quality B, 1) - 3. Initial Therapy use topical preparations for
initial therapy of diffuse, uncomplicated AOE.
Systemic antimicrobial therapy should not be used
unless extension outside the ear canal or
specific risk factors (evidence quality B)
28
AAO Acute OE Guidelines 2006
- 4. Topical Therapy consider concordance, side
effects and cost (evidence quality B) - 5. Drug Delivery inform patients how to
administer topical drops. Consider aural toilet
or wick (evidence quality C and D) - 6. Non-Intact Tympanic Membrane prescribe a
non-ototoxic topical preparation if membrane not
intact (evidence quality D) - 7. Outcome Assessment Reassess in 3 days if no
improvement to exclude other causes of
illness.(evidence quality C)
29
References
- Rosenfeld RM, et al American Academy of
Otolaryngology--Head and Neck Surgery Foundation.
Clinical practice guideline acute otitis
externa. Otolaryngol Head Neck Surg 2006
Apr134(4 Suppl)S4-23. - http//www.bris.ac.uk/depts/ENT/otoscopy_tutorial.
htm - Clinical Evidence, BMJ
- Sander, R Otitis Externa A Practical Guide to
Treatment and Prevention Amer. Family Physician
2001 Vol. 63/No. 5 p927-941
30
An Approach to Vertigo
- K Boothroyd
- 2008
31
Definition
- Vertigo is a type of dizziness and involves a
false sensation that one's self or the
surroundings are moving or spinning, usually
accompanied by nausea and loss of balance
32
Differential diagnosis
- Peripheral causes
- Benign positional vertigo
- Vestibular neuritis
- Menieres disease
- Viral labyrinthitis
- Ear infections inc chronic otitis media
- Eustachian tube dysfunction
- Drugs salicylate, quinine, aminoglycosides
- Nasopharyngeal carcinoma
- Central causes
- Cerebrovascular disease
- Migraine
- Multiple sclerosis
- Acoustic neuroma
- Vertebrobasilar ischaemia
- Epilepsy
- Syringobulbia
- Cerebellar tumours / Cerebellar Pontine Angle
tumours - Post head injury
- Ramsay Hunt Syndrome
33
Features of peripheral vertigo
- Usually has a sudden onset
- Hearing loss and tinnitus are more common
- Non-auditory neurological symptoms are rare
- Causes mild to moderate imbalance
- Nystagmus is both horizontal and rotational and
improves with fixing of gaze
34
Features of central vertigo
- Gradual onset (except TIA/CVA)
- Usually accompanied by other neurological signs
and symptoms - Auditory features are uncommon
- Causes severe imbalance
- Nystagmus is unidirectional (vertical/
horizontal/ torsional) not improved by fixing
gaze.
35
Miscellaneous causes
- Anaemia
- Hypotension
- Hypoglycaemia
- Cholesteatoma
- Ototoxic drugs
- Otitis media
36
Duration of symptoms in different causes of
vertigo
37
Vertigo without deafness
- Benign Positional Vertigo
- Vestibular neuronitis
- Acute vestibular dysfunction
- Medication e.g. Aminoglycosides
- Cervical spondylosis
- Whiplash
38
Vertigo with deafness
- Menieres Disease
- Labyrinthitis
- Labyrinthine trauma
- Acoustic neuroma
- Acute cochleo-vestibular dysfunction
- Ramsay Hunt Syndrome
- Perilymphatic fistula
- Syphilis (rare)
39
The history is all important
- Onset sudden or gradual?
- Precipitating event e.g. trauma/flying/diving
- Duration of vertigo?
- Nausea and/or vomiting?
- Hearing loss?
- Tinnitus?
- Imbalance mild/moderate/severe?
- Associated pain?
- Other neurological symptoms?
- Medications? (aminoglycosides, barbiturates,
phenytoin)
40
Can you guess what it is yet?
Formulate a hypothesis from your history
41
Case 1
- 50 yr old woman
- Vertigo associated with nausea
- No hearing loss/tinnitus
- First happened whilst hanging her curtains last
week, since then, when she turns in bed - Each episode lasts less than a minute
42
Benign positional vertigo
- dizziness or vertigo of sudden onset that is
provoked by certain changes in head position
43
Case 2
- 40 yr old blue eyed man, called to see on a home
visit - Sudden onset 3 hrs ago of vertigo, nausea,
vomiting, on off deafness ringing in right
ear - Right ear felt full for past couple of days
- Never happened before, pt starting to feel a bit
better now but very anxious
44
Ménières Disease
- Meniere's disease is classically characterised by
episodic attacks of - vertigo
- hearing loss
- tinnitus
- a feeling of fullness or pressure in the ear
- there may also be
- nystagmus
- nausea and vomiting
- Cause unknown. ? Increased fluid and pressure in
the endolymphatic compartment of the inner ear. - Usually unilateral.
45
Case 3
- 30 yr old woman, fit and well
- Sudden onset severe vertigo, nausea and vomiting
whilst at work - No deafness or tinnitus
- Drove home but felt pretty unsteady
- Relieved by lying still
46
Labyrinthitis/ Vestibular neuritis/ acute
vestibular failure
- Labyrinthitis
- Labyrinthitis is the commonest cause of acute
vertigo associated with sweating, nausea,
vomiting, pallor and occasional diarrhoea. - Clinical features of labyrinthitis include
- nystagmus - towards the side opposite to the
lesion. - there may also be a profound sensorineural
deafness.
47
Labyrinthitis/ Vestibular neuritis/ acute
vestibular failure
- Vestibular neuritis
- inflammation of the vestibular apparatus
- abrupt, onset incapacitating vertigo in a
previously healthy adult. The patient may feel
very unwell and may vomit. They often lie still
in bed. - no tinnitus or deafness.
- Acute attack lasts 2-5 days, followed by a steady
resolution over a period of 6 - 12 weeks.
48
Case 4
- 40 yr old man, arrived back from Egypt this
morning, rough flight - During the flight, sudden onset of vertigo,
nausea and deafness in right ear - No tinnitus
- Unsteady on his feet, symptoms relieved by lying
still now he is at home - Is my ear blocked Doc? Had something like this
before but didnt go deaf that time
49
Perilymphatic Fistula
- Rupture of the oval or round window results in
leakage of perilymph from the inner ear into the
middle ear - Causes flying, diving, sudden physical exertion,
childbirth, stapedectomy - Clinical features incude
- sudden or fluctuating hearing loss
- vertigo
- lightheadedness
- disequilibrium
- motion intolerance
- nystagmus
50
Examination
- BP ( BM if indicated)
- Otoscopy look for vesicles, otitis media,
cholesteatoma - Apply pressure to tragus/external auditory meatus
nystagmus/vertigo indicates perilymph fistula
(Henneberts sign) - Cranial nerves look for palsies, deafness,
nystagmus, dysarthria
51
Examination continued...
- Tuning fork tests if patient has hearing loss
- Tests of cerebellar function DANISH
- Full neurological examination if indicated
- Hallpike manoeuvre
52
Indications for referral
- Neurological symptoms (admit/urgent referral)
- Cranial nerve palsy (2wk wait ?CNS ca.)
- Unilateral sensorineural deafness (2wk wait ?CNS
ca.) - Positive Henneberts sign (urgent)
- Atypical nystagmus e.g. Non-horizontal,
persisting for weeks, changing direction, or
differing in each eye (urgent) - Abnormality of TM/ inadequate visualisation of
entire TM - Recurrent separate episodes
53
Symptomatic treatment
- Acute episode
- Cinnarazine 15-30mg tds, OR
- Prochlorperazine 5-10mg tds, OR
- Prochlorperazine 12.5mg IM bd, OR
- Prochlorperazine 25mg PR
- Recurrent episodes
- Betahistine 16mg tds regularly is useful in
Menieres - Stop smoking, restrict excess caffiene or alcohol
- Restrict salt fluid intake
54
Driving
The applicant or licence holder must notify DVLA
unless stated otherwise in the text. (Excerpt
from the At a glance Guide to the current Medical
Standards of Fitness to Drive, Drivers Medical
group, DVLA September 2007)
55
References
- http//www.aafp.org/afp/20060115/244.html
- Ronald H Labuguen. Initial evaluation of
vertigo. Am Fam Physician 200673 244-251, 254 - www.gpnotebook.co.uk
- www.dvla.gov.uk
56
Rhinitis
57
Definition
- Inflammation of the lining of the nose
- As the lining of the nose and paranasal sinuses
are continuous, it is rare for inflammation to
affect one without the other. As such, the
description rhinosinusitis is often more
appropriate.
58
Classification
59
Allergic Rhinitis
- May be seasonal or perennial
- Rhinorrhoea, nasal blockage and sneezing attacks
for gt 1 hour per day for gt 2 weeks - IgE mediated inflammatory reaction to an antigen
60
Epidemiology
- Estimated minimum prevalence of allergic rhinitis
is 231 - subjects with seasonal rhinitis are more likely
to be atopic and to have eczema and a family
history of hayfever than those without rhinitis. - Those with perennial rhinitis are more likely to
have past or current eczema or migraine, be
wheezy or labelled asthmatic, or have a family
history of nose trouble other than hayfever. 2
61
Aetiology
- Seasonal rhinitis most commonly an allergic
reaction to pollens, usually grasses - Perennial rhinitis dust, mites, feathers,
animals - Many patients are allergic to both seasonal and
perennial allergens
62
Clinical features 1
- nasal blockage - intermittent, alternating
unilateral blockage - a persistent unilateral
blockage may indicate a mechanical cause e.g.
septum deviation, nasal polyp - sneezing - often paroxysmal
- rhinorrhoea - can be anterior resulting in
persistent sniffing and nose-blowing, or
posterior resulting in a postnasal drip
63
Clinical features 2
- epiphora, reddening of conjunctivae, swelling of
eyelids - reduced taste or smell
- headaches - often without sinusitis the pain may
be referred to the forehead, lateral to nose,
around the eyes, or over the cheeks - reduced hearing - due to eustachian tube
dysfunction
64
Clinical features 3
- Signs may include
- Oedematous nasal mucosa, often blue
- Clear nasal discharge
- Nasal crease or salute, esp in children
65
Diagnosis
- History
- Exposure to allergen followed by rhinitis
- Variation in symptoms throughout day (perennial),
season, location gives clues to allergens - Skin prick testing
- RAST
66
Management of allergic rhinitis
- Environmental
- Medical
- Surgical
- Criteria for referral
67
Environmental
- General measures
- Humidity control
- Avoidance of irritants
- Specific measures
- Eg removal of household pets, minimise carpeting,
keep windows closed in pollen season
68
Medical 1
- 1st line non-sedating anti-histamines eg
loratidine - Topical anti-histamines for nasal congestion eg
azelastine - Topical nasal steroids eg budesonide, fluticasone
- Sodium cromoglycate eye drops for allergic
conjunctivitis
69
Medical 2
- In severe cases of hay fever consider low dose
systemic steroids - use of depot injections of triamcinolone is no
longer acceptable
70
Surgical
- Surgical treatment may be contemplated if medical
treatment is unsuccessful - Eg surgical reduction of inferior tubinates or
correction of deviated nasal septum
71
Refferal criteria for perennial rhinitis
- Refractory to treatment eg 6/52 nasal steroids
- Unilateral nasal symptoms esp if
pain/bleeding.obstruction - Nasal perforation, ulceration or
- collapse
- Suspected structural abnormality
72
Classification
73
Non-allergic rhinitis - infective
- Acute
- - common cold!
- Chronic
- Infection with specific organism
- Atrophic
- Immune deficiency
- Mucociliary clearance abnormality
74
Non-allergic rhinitis non-infective
- This includes
- Hyperreactive or vasomotor
- Rhinitis medicamentosa
- Anatomical or mechanical rhinitis
- Tumours benign, malignant, primary or secondary
- non-healing granulomas
75
References
- 1. Bauchau V, Durham SR. Prevalence and rate of
diagnosis of allergic rhinitis in Europe. Eur
Resp J 200424758-64 - 2. Thorax 1991 Dec46(12)895-901
- Prev Med 1998 Jul-Aug 27(4)617-22
76
SINUSITIS
77
Objectives
- What are sinuses?
- Acute and Chronic Sinusitis.
- Red Flags.
- Complications.
78
Sinuses
- Series of air filled sacs w nasal mucosa.
- Cranial cavity and eye closely related.
- Maxillary, ethmoidal, frontal, sphenoidal.
- Failure of drainage can lead to (rhino)
sinusitis. - Infection, allergy, obstruction.
79
ACUTE - upto 4 wks SYSTEMIC UPSET RHINORRHOEA MUC
OPUS WORSE BENDING WORSE W MOVEMENT
CHRONIC - 12 wks / more OTHERWISE WELL POST
NASAL DRIP POOR CONCENTRATION
SYMPTOMS FACIAL PAIN HEADACHE NASAL
OBSTRUCTION ANOSMIA HALITOSIS
80
Acute Sinusitis
- Commonly infective bacterial/viral.
- Stagnation of fluid can lead to........
- 2 Infected Strep pneum, HI, Staph.
- Nasal polyps, deviated septum, dental/tonsil/adeno
id infections, rhinitis all pre-dispose to
sinusitis.
81
Treatment
- Pain relief analgesia / antipyretics
- ?Inflammation ephedrine/oxymetazoline or
systemic - OBSERVATION mild pain low fever can be
observed for 7 days with f/u
82
Treatment contd
- Rx infection (not routinely) Abx if
mucopurulent dx w facial pains, systemic upset,
worsening over 5 to 7 days. - amoxicillin 500 mg tds 7-14/7 or erythromycin
500mg qds or doxycycline 100mg-200mg per day
83
Chronic Sinusitis
- Frequent rhinosinusitis.
- Often combined allergic/ infective.
- Medical Abx, intranasal steroids.
- Surgery if not resolving (FESS) endoscopic
84
COMPLICATIONS
- FACIAL / PERIORBITAL CELLULITIS
- OSTEOMYELITIS
- MENINGITIS
- CEREBRAL ABCESS
- MUCOCOELE
85
RED FLAGS
- UNILATERAL SYMPTOMS
- HEADACHE
- PYREXIA (SWINGING)
- NEUROLOGY
- ORBITAL SWELLING
86
Orbital Cellulitishttp//eyelearn.med.utoronto.ca
/Lectures04-05/Paediatric/images/Paediatric_52.jpg
87
http//www.emedicine.com/oph/images/230_1small.jpg
http//www.entkent.com/images/orbital-cellulitisc
200pxw.jpg
88
(No Transcript)
89
Sore throats in General Practice
- Lucy Cowdrey
- VTS Teaching Jan 2007
90
Why is it important?
- Common each GP sees 120 cases / year
- Antibiotic avoidance / patient education 70 of
cases are viral - Consider complications rare but important
91
When would you treat?
- Various models, none particularly sensitive or
specific - Centor (1981) criteria
- History of fever
- Tonsillar exudate
- Tender and enlarged anterior cervical lymph nodes
- Absence of cough
- If 3-4 signs present, there is a 40-60 chance of
group A strep infection
92
What would you treat with?
- Penicillin V or erythromycin if allergic
- Recommended course is 10 days for Group A Strep
pharyngitis (Dajani et al 1995) - Twice daily dosing (250mg BD in children, 500mg
BD in adults) is as effective as TDS or QDS
(Geber et al 1985)
93
Other management strategies?
- Throat swab
- Delayed prescription
- Always find out exactly what the patient is
concerned about, as most people with sore throats
do not attend - Consider FBC / monospot
94
When would you refer for tonsillectomy?
- NICE guidelines for children lt15yrs
- If gt5 attacks acute sore throat in 12 months
documented by parent or doctor severe enough to
disrupt day-to day activity
95
Complications
- Quinsy
- Retropharyngeal abscess
- Rheumatic fever (antibiotics reduce risk by 70)
- Glomerulonephritis
96
Quinsy
- Severe pain
- Trismus
- Drooling / difficulty swallowing
- Toxic
- O/E displacement of uvula away from quinsy, may
be obvious abscess - Admit for IV abx / ID
97
Figure 1 Left sided quinsy causing uvula
deviation
98
Retropharyngeal abscess
- Toxic, ill
- Usually children
- Dysphagia
- Stridor
- Neck stiffness
- O/E may be unilateral neck swelling
- Admit for IV abx ID
99
When is a sore throat not a sore throat?
100
Glandular fever
- Consider in teenager / young adult with sore
throat lasting gt1 week - Also malaise, fever, lymphadenopathy
- O/E may have HSM, may be tonsillar exudate
- Treat secondary infection, admit for steroids if
airway compromise - Counsel patients may last for months
- Complications hepatitis, splenic rupture,
encephalitis
101
Oropharyngeal cancer
- Rare (3600 cases / year)
- Usually elderly, male smokers
- Painful dysphagia, sore throat, otalgia, lump in
neck - May present with metastatic lymph node
- 40 5 year survival
- Refer any suspicious lesions, also refer red /
white patches in mouth or ulcers lasting gt3/52
102
Figure 2 Left sided tonsillar carcinoma before
(A) and 22 months after surgery (B)
103
Figure 3 leukoplakia of tongue
104
Summary
- Sore throats are common and mostly dont need
treatment - Always address underlying concerns
- Beware of the unwell child and the elderly smoker
105
Questions?
106
Case Study
- A 32 yr old man presents with sudden onset
weakness on the left side of his face. He also
complains he cannot close his left eye. He is
normally fit and well and has nt seen his GP for
the last 5 years. He is anxious and thinks he has
had a stroke. - What else do you want to know and what should you
do?
107
(No Transcript)
108
Bells Palsy- diagnosis of exclusion
- Unilateral facial nerve paralysis
- LMN lesion- part of each facial nucleus supplying
the upper face receives supranuclear fibres from
each hemisphere hence UMN lesion, upper part of
face spared - Function of facial nerve
- Motor muscles of facial expression, lacrimation,
salivation, motor fibres to stapedius muscles in
middle ear - Sensory ant. 2/3 of tongue
109
(No Transcript)
110
cont
- Epidemiology
- -Peak age onset 10-40yrs
- -Malefemale
- -Lifetime incidence 165
- Pathology
- -Inflammation of the facial nerve within the
petrous temporal bone and as it traverses the
stylomastoid foramen in the skull base - Aetiology
- -Unknown
- -Some research implicated HSV type 1
- -Other possibilities post viral infection,
heredity, autoimmune,vascular ischaemia
111
Presentation
- Sudden onset unilateral facial weakness
- Pain in or behind the ear
- Numbness can occur on the affected side
- Loss of taste on the ipsilateral ant 2/3 tongue
- Ask about history of a rash- may indicate herpes
zoster
112
Causes to exclude
- Tumour- parotid, cholesteatoma
- Meningitis
- Stroke
- DM
- Head trauma
- Sarcoid
- Lyme disease- hx of tick exposure
- Ramsay Hunt- vesicles in ext. ear canal
- NB. Other causes do not usually exclusively have
LMN FN palsy
113
Treatment
- Controversial
- If using, ideally needs to be lt72 hrs (7days
max.) - Prednisolone 1mg/kg/day (max 80mg), reducing over
10/7 and aciclovir 800mg x5 per day for 5/7 for
moderate to severe palsies - Protect eye with taping, lacrilube, artificial
tears
114
Prognosis
- Good reassure
- 85 note an improvement within the first 3/52
- 70 complete recovery, 13 insignificant
sequelae, 17 permanent - May take 12mnths to recover competely