Maxillofacial trauma - PowerPoint PPT Presentation
1 / 33
Title:
Maxillofacial trauma
Description:
Third peak. Occurs some days or weeks after injury as a ... Assessment of head injury (behavioral responses 'motor and verbal responses' and eye opening) ... – PowerPoint PPT presentation
Number of Views:3510
Avg rating:3.0/5.0
Title: Maxillofacial trauma
1
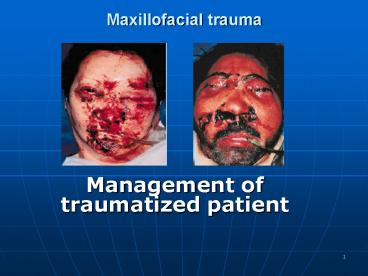
Maxillofacial trauma
- Management of traumatized patient
2
Causes
- ? Road traffic accident (RTA)
- 35-60
- Rowe and Killey 1968
- Vincent-Towned and Shepherd 1994
- ? Fight and assault (interpersonal violence)
- Most in economically prosperous countries
- Beek and Merkx 1999
- ? Sport and athletic injuries
- ? Industrial accidents
- ? Domestic injuries and falls
3
Incidence
- Literatures reported different incidence in
different parts of the WORLD and at different
TIMES - v 11 in RTA (Oikarinen and Lindqvist 1975)
- Mandible (61)
- Maxilla (46)
- Zygoma (27)
- Nasal (19.5)
4
Factors affecting the high/low incidence of
maxillofacial trauma
- Geography
- Fight, gunshot and RTA in developed and
developing countries respectively (Papavassiliou
1990, Champion et al 1997) - Social factors
- Violence in urban states (Telfer et al 1991
Hussain et al 1994 Simpson McLean 1995) - Alcohol and drugs
- Yong men involved in RTA wile they are under
alcohol or drug effects (Shepherd 1994) - Road traffic legislation
- Seat belts have resulted in dramatic decrease
in injury (Thomas 1990, as reflected in reduction
in facial injury (Sabey et al 1977) - Season
- Seasonal variation in temperature zones
(summer and snow and ice in midwinter) of RTA,
violence and sporting injuries (Hill et al 1998)
5
Assessment of traumatized patient
- This should not concentrate on the most obvious
injury but involve a rapid survey of the vital
function to allow management priorities
5 of all deaths world wide are caused by
trauma This might be much higher in this country
6
Peaks of mortality
- First peak
- Occurs within seconds of injury as a result of
irreversible brain or major vascular damage - Second peak
- Occurs between a few minutes after injury and
about one hour later (golden hour) - Third peak
- Occurs some days or weeks after injury as a
result of multi-organ failure
7
Organization of trauma services
triage decisions are crucial in determining
individual patients survival
- Pre-hospital care (field triage)
- Care delivered by fully trained paramedic in
maintaining airway, controlling cervical spine,
securing intravenous and initiating fluid
resuscitation - Hospital care (inter-hospital triage)
- Senior medical staff organized team to ensure
that medical resources are deployed to maximum
overall benefit - Mass casualty triage
8
Primary survey
- ? Airway maintenance with cervical spine
control - ? Breathing and ventilation
- ? Circulation with hemorrhage control
- ? Disability assessment of neurological status
- ? Exposure and complete examination of the patient
9
Airway
- Satisfactory airway signifies the implication of
breathing and ventilation and cerebral function - Management of maxillofacial trauma is an integral
part in securing an unobstructed airway - Immobilization in a natural position by a
semi-rigid collar until damaged spine is excluded
10
Sequel of facial injury
Obstruction of airway
asphyxia
Cerebral hypoxia
Brain damage/ death
Is the patient fully conscious? And able to
maintain adequate airway?
Semiconscious or unconscious patient rapidly
suffocate because of inability to cough and adopt
a posture that held tongue forward
11
Immediate treatment of airway obstruction in
facial injured patient
- ?Clearing of blood clot and mucous of the mouth
and nares and head position that lead to escape
of secretions (sit-up or side position) - ? Removal of foreign bodies as a broken denture
or avulsed teeth which can be inhaled and
ensuring the patency of the mouth and oropharynex - ? Controlling the tongue position in case of
symphesial bilateral fracture of mandible and
when voluntary control of intrinsic musculature
is lost - ? Maintaining airway using artificial airway in
unconscious patient with maxillary fracture or by
nasophryngeal tube with periodic aspiration - ? Lubrication of patients lips and continuous
supervision
12
Additional methods in preservation of the airway
in patient with severe facial injuries
- Endotracheal intubation
- Needed with multiple injuries, extensive soft
tissue destruction and for serious injury that
require artificial ventilation - Tracheostomy
- Surgical establishment of an opening into the
trachea - Indications 1. when prolonged artificial
ventilation is necessary - 2. to facilitate
anesthesia for surgical repair in certain cases - 3. to ensure a
safe postoperative recovery after extensive
surgery - 4. following
obstruction of the airway from laryngeal edema - 5. in case of
serious hemorrhage in the airway - Circothyroidectomy
- An old technique associated with the risk of
subglottic stenosis development particularly in
children. The use of percutaneous dilational
treachestomy (PDT) in MFS is advocated by Ward
Booth et al (1989) but it can be replaced with
PDT. - Control of hemorrhage and Soft tissue laceration
- Repair, ligation, reduction of fracture and
Postnasal pack
13
Cervical spine injury
- Can be deadly if it involved the odontoid
process of the axis bone of the axis vertebra - If the injury above the clavicle bone, clavicle
collar should minimize the risk of any
deterioration
14
Breathing and ventilation
- Chest injuries
- Pneumothorax, haemopneumothorax, flail
segments, reputure daiphram, cardiac tamponade - signs
Clinical Deviated trachea Absence of breath
sounds Dullness to percussion Paradoxical
movements Hyper-response with a large
pneumothorax Muffled heart sounds
Radiographical Loss of lung marking Deviation of
trachea Raised hemi-diaphragm Fluid
levels Fracture of ribs
15
Emergency treatment in case of chest injury
- Occluding of open chest wounds
- Endotreacheal intubation for unstable flail chest
- Intermittent positive pressure ventilation
- Needle decompression of the pericardium
- Decompression of gastric dilation and aspiration
of stomach content
16
Circulation
- Circulatory collapse leads to low blood
pressure, increasing pulse rate and diminished
capillary filling at the periphery
Patient resuscitation Restoration of
cardio-respiratory function Shock
management Replacement of lost fluid
17
- Fluid for resuscitation
- ?Adequate venous access at two points
- ? Hypotension assumed to be due to hypovolaemia
- ? Resuscitation fluid can be crystalloid, colloid
or blood ringer lactate - ? Surgical shock requires blood transfusion,
preferably with cross matching or group O - ? Urine output must be monitored as an indicator
of cardiac out put
18
- Reduction and fixation will often arrest bleeding
of long duration - Pulse and blood pressure should be monitored and
appropriate replacement therapy is to be started
19
Neurological deficient
- Rapid assessment of neurological disability is
made by noting the patient response on four
points scale - A Response appropriately, is Aware
- V Response to verbal stimuli
- P Response to painful stimuli
- U Does not responds, Unconscious
20
Glasgow coma scale (GCS)(Teasdale and Jennett,
1974)
Score 8 or less indicates poor prognosis,
moderate head injury between 9-12 and mild
refereed to 13-15
21
Exposure
- All trauma patient must be fully exposed in a
warm environment to disclose any other hidden
injuries - When the airway is adequately secured the
second survey of the whole body is to be carried
out for - Accurate diagnosis
- Maintenance of a stable state
- Determination of priorities in treatment
- Appropriate specialist referral
22
Secondary surveyAlthough maxillofacial injuries
is part of the secondary survey, OMFS might be
involved at early stage if the airway is
compromised by direct facial trauma
- Head injury
- Abdominal injury
- Injury to extremities
23
Head injuryMany of facial injury patients
sustain head injury in particular the mid face
injuries
- Open
- Closed
- it is ranged from Mild concussion to brain death
24
Signs and symptoms of head injury
- Loss of conscious
- OR
- History of loss of conscious
- History of vomiting
- Change in pulse rate, blood pressure and pupil
reaction to light in association with increased
intracranial pressure - Assessment of head injury (behavioral responses
motor and verbal responses and eye opening) - Skull fracture
- Skull base fracture (battles sign)
- Temporal/ frontal bone fracture
- Naso-orbital ethmoidal fracture
25
- slow reaction and fixation of dilated pupil
denotes a rise in intra-cranial pressure - Rise in intercranial pressure as a result of
acute subdural or extradural hemorrhage
deteriorate the patients neurological status - Apparently stable patient with suspicion of head
injury must be monitored at intervals up to one
hour for 24 hour after the trauma
26
Hemorrhage
- Acute bleeding may lead to hemorrhagic shock
and circulatory collapse - Abdominal and pelvis injury liver and internal
organs injury (peritonism) - Fracture of the extremities (femur)
27
Abdomen and pelvis
- In addition to direct injuries, loss of
circulating blood into peritoneal cavity or
retroperitonial space is life threatening,
indicated by physical signs and palpation,
percussion and auscultation - Management
- Diagnostic peritoneal lavage (DPL) to detect
blood, bowel content, urine - Emergency laprotomy
28
Extremity trauma
- Fracture of extremities in particular the
femur can be a significant cause of occult blood
loss. Straightening and reduction of gross
deformity is part of circulation control - Cardinal features of extremities injury
- Impaired distal perfusion (risk of ischemia)
- Compartment syndrome (limb loss)
- Traumatic amputation
29
Patient hospitalization and determination of
prioritiesFacial bone fracture is hardly ever
an urgent procedure,simple and minor injury of
ambulant patient may occasionally mask a serious
injury that eventually ended the patients life
- ? emergency cases require instant admission
- ? conditions that may progress to emergency
- ? cases with no urgency
30
Preliminary treatment in complex facial injury
- Soft tissue laceration (8 hours of injury with no
delay beyond 24 hours) - Support of the bone fragments
- Injury to the eye
- As a result of trauma, 1.6 million are blind,
2.3 million are suffering serious bilateral
visual impairment and 19 million with unilateral
loss of sight (Macewen 1999) - Ocular damage
- Reduction in visual acuity
- Eyelid injury
31
Prevention of infectionFractures of jaw
involving teeth bearing areas are compound in
nature and midface fracture may go high, leading
to CSF leaks (rhinorrhoea, otorrhoea) and risk of
meningitis,and in case of perforation of
cartilaginous auditory canal
- Diagnosis
- Laboratory investigation, CT and MRI scan
- Management
- Dressing of external wounds
- Closure of open wounds
- Reposition and immobilization of the fractures
- Repair of the dura matter
- Antibacterial prophylaxis (as part of the general
management (Eljamal, 1993)
32
Control of pain Displaced fracture may cause
severe pain but strong analgesic ( Morphine and
its derivatives) must be avoided as they depress
cough reflex, constrict pupils as they may mask
the signs of increasing intracranial pressure
- Management
- ? Non-steroidal anti-inflammatory drugs can be
prescribed (Diclofenac acid) - ? Reduction of fracture
- ? sedation
33
In patient care
- Necessary medications
- Diet (fluid, semi-fluid and solid food) intake
and output (fluid balance chart) - Hygiene and physiotherapy
- Proper timing for surgical intervention




![[PDF] Oral and Maxillofacial Trauma 4th Edition Free PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10084203.th0.jpg?_=202407230910)




![[PDF] Principles of Oral and Maxillofacial Surgery 6th Edition Ipad PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10087823.th0.jpg?_=20240729071)



![❤[PDF]⚡ Oral and Maxillofacial Surgery 3rd Edition PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10095500.th0.jpg?_=20240810026)
















