The Reproductive System PowerPoint PPT Presentation
1 / 44
Title: The Reproductive System
1
The Reproductive System
2
What is the primary function of the reproductive
system?
- To produce gametes
- To produce reproductive hormones
- To promote growth
- To promote maturation
3
Male Anatomy
- Sex organs consist of gonads,internal accessory
ducts and glands and external reproductive
structures known as genetalia. - Male Gonads - produce gametes and hormones
- Testes (means witness in latin, men in ancient
Rome placed on hand on genitals) -sperm producing - From the testes - sperm go to epididymis gt ductus
deferens gturethra - Accessory sex glands are seminal vesicles,
prostate, and bulbourethral which empty
secretions into the ducts during ejaculation
4
The ______ is (are) responsible for producing
semen.
- testes
- seminal vesicles
- prostate gland
- b and c
5
Seminiferous tubules
- Coiled tubes in 250-300 compartments
- Leave the testis and join the epididymis, a
single duct that forms a coiled cord - Seminiferous tubules (sperm factory) have 2 types
of cells - Spermatocytes
- Sertoli cells
6
(No Transcript)
7
- Scrotum -viable sperm cannot be produced at core
body temperature so the scrotum provide a
temperature 3 degrees C lower. - The scrotum also responds to temperature to
maintain a fairly constant temperature. - Testes each contain seminiferous tubules that act
as sperm factories - The tubules converge to form a straight tubule
that conveys sperm to the rete testis, and then
they leave through the efferent ductules and
enter the epididymis
8
Duct system
- Epididymis - immature sperm are moved through the
duct. - Takes 20 days - sperm gain the ability to swim
- When smooth muscle of epididymis contracts,
expelling sperm to the ductus deferens - Sperm can be stored for many months - if longer
they are phagocytized.
9
Ductus deferens
- Propels sperm from storage site in the epididymis
into the urethra - Vasectomy cutting the vas in the scrotal sac.
Sperm no longer reach exterior
10
Accessory glands
- Seminal vesicles, bulbourethral glands, prostate
gland - 1. Seminal vesicles lie on the posterior wall of
the bladder - Secretion is 60 of volume of sperm an alkaline
fluid of fructose sugar, ascorbic acid, a
coagulating enzyme, and prostaglandins. - Sperm and seminal fluid mix in a duct and enter
the urethra
11
Prostate gland
- Encircles urethra inferior to the bladder
- Made of tubular alveolar glands in smooth muscle
- Secretion is 1/3 of semen volume
- Contains citrate, a nutrient, enzymes, and an
antigen that activates sperm - Empties directly into urethra
12
Bulbourethral gland
- Produce mucus prior to ejaculation of sperm
- Empties secretions into the urethra through a
duct
13
Spermatogenesis and meiosis
- Spermatagonia in the seminiferous tubules enlarge
to form a primary spermatocyte -gtsecondary
spermatocyte -gtspermatids -gtsperm - During the change from spermatocyte to spermatid,
the 46 chromosomes (23 pairs) of the spermatocyte
divide, so that 23 go to one spermatid and the
other 23 to the second. - During meiotic division, the male Y chromosome
goes to one spermatid and becomes the male sperm,
and the female X goes to another and becomes a
female sperm. The sex is determined by which of
these fertilizes the ovum.
14
Spermiogenesis - streamlining
- 1. Undergoes a streamlining process called
spermiogenesis. Sheds its excess cytoplasm and
forms a tail - 3. Result sperm has
- head - genetic
- midpiece - metabolic (mitochondria ATP)
- tail - locomotor region
- 4. Sustentacular cells form the blood-testis
barrier, nourishing spermatogenic cells, move
them to lumen of tubules, and secrete fluid for
sperm transport
15
As many as _______ sperm are made each day.
- 300
- 3000
- 400 million
- 750 trillion
16
Sperm
- Semen ejaculated is 3.5 ml or 120 million sperm
- So about 400 million sperm are present in several
ml - When falls below 20 million infertility
- Majority of abnormal sperm infertility
17
Male hormonal regulation
- GnRH, from hypothalamus, stimulates the ant.
pituitary to release FSH and LH into the blood. - Testosterone is secreted by the interstitial
cells of Leydig in the testes when stimulated by
LH. This provides negative feedback - To initiate spermatogenesis, both FSH and
testosterone are needed
18
Male hormonal function
- Testosterone is secreted in the 7 week old embryo
and continues for 10 weeks, then is turned off
until puberty. Remains high until about age 50
and then decreases by 50 - Testosterone involved in
- muscle development
- Increases bone matirx
- Changes the pelvis by making it longer
- Increases BMR by up to 15
- Voice, baldness, skin
19
If testosterone were ineffective during
development of a males rain, what might be the
outcome?
- The brain would develop without any noticeable
difference from other males. - The brain might have a female orientation.
- Gender identity may be ambiguous.
- Both b and c are possible.
20
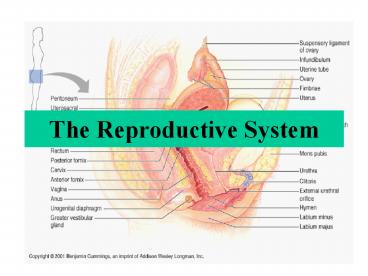
Female system
- Ovaries - female gonads are the primary
reproductive organ - Dual purpose
- 1. Female sex hormones - estrogens and
progesterone - 2. Forms gametes
21
Ovaries
- Paired ovaries flank uterus
- Each ovary held in place by ligaments
- Every 28 days, gonadotropic hormones from the
ant. pituitary cause - - 8-12 follicles to grow in the ovaries
- 1 matures and ovulates on the 14th day
- Ovulation a ripening follicle ejects its oocyte
22
Female duct system
23
- Falopian tube extends from ovary to the uterus
- Distal end expands and forms ampulla where
fertilization occurs - Ends in infundibulum, a funnel with fimbriae that
drape over ovary - Cilia propels oocyte into the falopian tube and
toward the uterus
24
Uterus
- Hollow, thick-walled organ that receives and
retains a fertilized ovum - Body major portion
- Fundus rounded superior region
- Cervix narrow neck/outlet that projects into
vagina - Supported by mesentary and ligaments
25
Uterine wall
- 3 layers perimetrium, myometrium, endometrium
- Perimetrium - outer serous layer
- Myometrium - mid layer of smooth muscle
- Endometrium - mucosal lining
26
Endometrium
- Straight artery that serve basalis and spiral
arteries - Thin walled veins
- 2 strata
- Functionalis -undergoes cyclic changes in
response to blood levels of ovarian hormones and
is shed during menstration - Basalis - forms a new layer after menstration
functionalis
basalis
27
Female Physiology-Oogenesis
- Oogenesis - the beginning of the egg. 1 year to
complete - Before birth -oogonia or diploid stem cells of
ovaries multiply by mitosis, then enter a growth
phase. - This creates 500,000 primary oocytes
28
- By birth, a females lifetime supply of primary
oocytes - 2 million of them- are in cortex of the
immature ovary. - Remain suspended through childhood until age
10-14 - Puberty, 400,000 oocytes remain.
- 1st and 2nd meiotic divisions occur in ovary
after puberty - Some are activated monthy by hormones and 1 is
selected to continue meiosis I
29
- Each month 1 primary ooctye completes meiosis I,
producing a large secondary oocyte - Meiosis II of the secondary oocyte produces a
functional ovum, but meiosis II does not occur
unless the secondary oocyte is penetrated by
sperm
30
Ovarian cycle
- Rhythmical changes leading to the maturation of a
single ovum - 28 days - 2 phases
- 1. Follicular growth- follicle growth of ovary.
Day 1-14 - 2. Luteal phase - corpus luteum activity. Day
14-28
31
Follicular phase
- Follicular growth - several primary follicles
mature to - 2. Secondary or mature follicle
- Growing follicle produces estrogen
- The growth of this follicle is stimulated by FSH
that is stimulated by estrogen - 4. Fluid-filled cavity forms called the antrum.
32
Luteal phase
- After expulsion of the ovum from the follicle,
(day 15-28), the follicle enlarges and fills with
a fluid or luteinizes to form a corpus luteum - that secretes progesterone and estrogen, but
mainly progesterone - Dependent upon LH secreted by the ant.pit.
- If fertilization does not occur, the luteum
degenerates in about 10 -12 days
33
Ovulation
- Ovary wall ruptures and expels the oocyte
- lt2 of ovulations, more than 1 oocyte is
ovulated can result in multiple births - Fraternal twins nonidentical twins are
different oocytes - Identical twins fertilization of a single
oocyte by a single sperm followed by separation
of the fertilized eggs daughter cells
34
Hormonal regulation of the ovarian cycle
- Hormonal controls at puberty
- A hypothalmic releasing hormone
gonadodtropin-releasing hormone (GnRH), - The anterior pituitary sex hormones FHS, LH
that are released in response to GnRH - The ovarian hormones, estrogen and progesterone,
secreted by the ovaries in response to the female
sex hormones from the anterior pituitary - These hormones are not secreted constantly, but
at differing rates during different times of the
cycle
35
Hormonal interactions during ovarian cycle
36
- A. Pituitary gonadotropins - LH and FSH
regulate the events of the ovarian cycle - B. Estrogens and progesterone cause changes in
the uterus - High estrogen levels are responsible for a surge
in LH/FSH
37
Menstrual cycle
- 1. Days 1-5 Menstrual phase uterus sheds all
but the deepest endometrium - Gonadotropins are rising and ovarian hormones are
low. FSH begins to rise - 2. Days 6-14 Proliferative phase
- Endometrium rebuilds with rising estrogen.
Glands enlarge, spiral arteries increase
endometrium becomes thick and well-vascularized. - Estrogens induce synthesis of progesterone
receptors - Rising estrogen causes cervical mucus to thin and
form channels that will facilitate sperm passage - Ovulation at end of this stage in response to gt LH
38
- Days 15-28 Secretory phase endometrium prepares
for inplantation. - Rising levels of progesterone cause spiral
arteries to coil. Uterine glands enlarge and
secrete glycoproteins that sustain the embryo
until it has implanted. - Increasing progesterone cause mucus to form a
plug that blocks sperm - If no ferttilization, corpus luteum degenerates,
LH declines, progesterone declines - With no hormonal support, spiral arteries kink,
dont get oxygen setting the stage for
menestration
39
The menstrual and proliferative phases overlap
the follicular phase and ovulation in ovarian
cycle.
Uterine secretory phase corresponds to the
ovarian luteal phase.
40
Effects of estrogen and progesterone
- 1. Estrogen promotes ovulation.
- 2. At puberty, it stimulates the growth of
reproductive organs and the growth spurt that
promotes appearance of secondary sex
characteristics (breasts, fat, pubic hair,
calcium uptake). - 3. Progesterone cooperates with estrogen in
breast maturation and regulation of the uterine
cycle. In pregnancy - prepares breast for
lactation
41
Estrogen
- Increased osteoblastic activity
- Increased protein deposition
- Increased metabolic rate
- Skin texture
42
The pill
- Estrogen or progesterone given during the first
half of the monthly cycle inhibit ovulation
43
Menopause
- After about 400 of the primordial follicles grow
to mature follicles and ovulate - Ovulation stops
- Estrogen levels fall
44
Progesterone
- Promotes secretory changes in the uterine
endometrium - Breast swelling and development of the alveoli