Ovulation PowerPoint PPT Presentation
Title: Ovulation
1
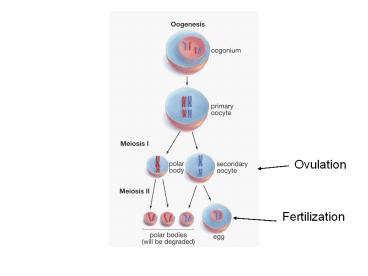
Ovulation
Fertilization
2
Maturation of sperm
- Sperms
- Incapable of fertilizing the oocyte immediately
after being released into the lumen of the
seminefrous tubules - Maturation
- In epidydimus
3
(No Transcript)
4
- Epidydimus
- Fluid reabsorption
- Increase concentrations of sperm by 100 folds
- Estrogen dependent
- Quiescence of sperms
- Slow activity
- Movement depends on musculature
- Addition of chemicals
- Glycoproteins
- Coating of sperm surface
5
- Maturation of sperm
- Ability to move on its own
- Nuclear condensation and loss of cytoplasm
- Metabolism alteration
- External source
- Increased mobility
- Changes in cell membrane
- Increased charge (glycosylation)
- Changes in protein profile
- Changes in lipid composition (fluidity)
6
- Maturation of sperm
- Androgen dependent
- Very high concentrations (ABP)
- Conversion to DHT
- Increased bioactivity
- Entire process will take several months to few
days
7
Movement of sperms
- Entering vas deference from epidydimus
- Muscular contraction rather than fluid movement
- Dense mass
- Serve as reservoir of sperms
- Lost in urine if no ejaculation
8
Sperm in male reproductive tract
- Semen
- Sperm plus seminal plasma
- Seminal plasma
- Derived from accessory sex glands
- Serves as fluid vesicle for transport
- Unnecessary for sperm function
9
- Seminal plasma
- Derived from accessory sex glands
- Serves as fluid vesicle for transport
- Serves as buffer
- Basic in nature
- Neutralizes acids
- Provides nutrients
- Fluctose
- sorbitol
10
(No Transcript)
11
- Semen composition
- Immune cells
- Infectious agents
12
Deposition of semen into the female reproductive
tract
- Coitus
- Physiological changes
- Genitalia
- Other parts of body
- Phases
- Described in humans by Johnson and Masters
- Four phases
- Excitement (sexual arousal)
- Plateau (intense arousal)
- Orgasm (involuntary climax)
- Resolution
- Absolute refractory phase in male
- Immediately after orgasm
13
- Excitement
- Vasocongestion
- Penile erection (engorgement of corpora cavanosa
and corpus spongiosum) - Vaginal lubrication (transudation)
- Enlargement of labia minora and clitorus
- Vaginal expansion
- Tenting effect on uterus
- Upward movement of uterus and cervix
- Fibrilation of uterus (contraction)
- Sex flush
- Myotonia
- Increased muscle tension
14
- Plateau
- Increased testis size
- Elevated from the original position
- Secretion of fluid
- Cowpers gland
- Sex flushes
- Engorgement of vaginal wall
- Orgasmic platform
- Formation of seminal pool
15
- Female orgasm
- Rhythmic contraction
- Vaginal wall
- Uterus
- Involuntary muscle spasm
16
- Male orgasm
- Contraction of accessory sex gland
- Collection of semen into the urethral bulb
- Contraction of bladder muscle
- Emission stage of ejaculation
- Expulsion of semen/ejaculation
- Muscle contraction
- Reproductive tract contraction
17
- Resolution
- Returning of body to nonaroused state
- Size of genitals
- Uptake of sperm by the cervix
- Dipping into the seminal pool as the uterus
returns to the normal position - Opening of cervical canal
18
- Site of semen deposition
- Varies among species
- Humans and cattle
- Near external portion of cervix (cervical os)
- Uterus in other species
- Formation of plug
- Enzymatic reaction
- Prevent backflow of semen
- Buffers
- Prevent sperm from other males to fertilize eggs?
19
Transport of sperm to the oviduct
- Sperm must enter female reproductive tract and
reside there for some time - Maximum fertility
- Sperm
- Viable inside of reproductive tract
- 24 to 48 hours in human
- 30 to 48 hours in cows
- Oocyte
- A finite life span
- 6 to 24 hours after ovulation in human
- Sperm must reach the oviduct at appropriate time
in order to remain viable and fertile
20
Transport of sperm to the oviduct
Preovulatry follicle
Semen pool
- Semen
- Deposited in the anterior part of the vagina near
the cervix - The majority of the sperm
- Lost because of retrograde flow of the mucus out
of the vagina - Killed because of the unfavorable environment for
sperm survival in the vagina.
21
Transport of sperm to the oviduct
- Some of the sperm
- Transported through cervical canal into the
uterus within minutes after sperm deposition - Rapid transport
- Rapid transport of sperm is caused by the
contraction of myometrium (muscle layer of the
uterus) and not by active movement of sperm - Sperm that enter the oviduct by rapid transport
- Often non-viable and unlikely to participate in
fertilization.
22
Transport of sperm to the oviduct
- Many sperm
- Trapped in the folds and crypts of the cervix
- Formation of sperm reservoirs within the cervix
- Critical
- More sperm ultimately reach the oviduct when more
sperm are available in the cervical reservoir
Folds and crypts of the cervix
23
Transport of sperm to the oviduct
- Slow transport of sperm
- After establishment of reservoir
- Ensures the availability of sperm in the oviduct
continuously - Large number of sperms
- Fails to reach the oviduct
- Many obstacles such as folding of the uterine
endometrium and the narrow diameter of the
uterotubal junction - Presumably to prevent polyspermy (more than one
sperm fertilizing the oocyte)
24
Transport of sperm to the oviduct
Uterotubal Junction
Ampullary- isthmic Junction
Isthmus
Ampulla
Infundibulum
- Aggregation of sperms
- The isthmus
- Sperm remain in the isthmus until ovulation
- Hyperactivation
- Rapid movement of tail and erratic swimming
motion - Near ovulation
- Essential for their upward movement toward the
ampulla.
25
Transport of sperm to the oviduct
Uterotubal Junction
Ampullary- isthmic Junction
Isthmus
Ampulla
Infundibulum
- Capacitation
- Changes in cell surface of the sperm
- Required for proper attachment and penetration of
the zona pellucida when the sperm encounters the
oocyte
26
- Capacitated sperms
- Acrosome reaction when encountering the oocyte
- Ability to bind and penetrate zona pellucida
- Swelling of acrosome
- Fusion of acrosomal membrane
- Exocytosis of acrosomal content
- Ca and cAMP dependent
27
(No Transcript)
28
- Acrosome reaction
- Triggered by the protein in the zona pellucida
- ZP3
- Sperms have receptors for ZPs
- Increased Ca uptake
- Release of hexosaminidase B (removal of ZP3)
29
- Acrosome reaction
- Must take place near the oocyte
- Reduced sperm viability
30
Fertilization
- Sperm encountering the oocyte
- Migration through the remaining cumulus cells
that surround the oocyte - Sperm binds to the zona pellucida
- Mediated by the sperm binding sites present on
zona pellucida
Cumulus cells
First polar body
31
Fertilization
- Within minutes of binding, the sperm begins to
penetrate the zona pellucida, and eventually
fuses with the oocyte - Equatorial and postacrosomal region
- Ca-dependent reaction
- Immediately after the sperm fuses with the
oocyte, the oocyte extrudes the second polar body - Oocyte becomes a haploid cell
Zona pellucida
Second polar body
32
Fertilization
- Once a sperm fuses with the oocyte, the zona
pellucida becomes hardened - Release of Ca
- Sperm binding sites disappear from the zona
pellucida - Hardening of zona and loss of sperm binding sites
are necessary in order to prevent polyspermy
Head of sperm
33
Fertilization
- Membrane of the sperm head
- Degraded and replaced by a new membrane
- Formation of a structure called the male
pronucleus - The maternal half of chromosomes
- The female pronucleus.
Male pronucleus
Female pronucleus
34
Fertilization
- Male and female pronuclei move toward the center
of the oocyte - Degradation of the membrane that surrounds each
pronucleus - Mixing of maternal and paternal chromosomes
- Restoration of the total number of chromosomes
Zygote