Decreased red cell production PowerPoint PPT Presentation
1 / 37
Title: Decreased red cell production
1
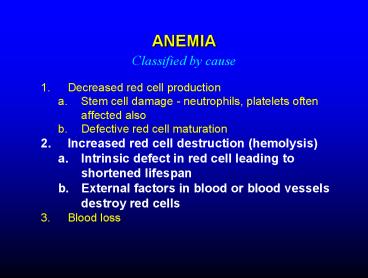
ANEMIA
Classified by cause
- Decreased red cell production
- Stem cell damage - neutrophils, platelets often
affected also - Defective red cell maturation
- Increased red cell destruction (hemolysis)
- Intrinsic defect in red cell leading to shortened
lifespan - External factors in blood or blood vessels
destroy red cells - Blood loss
2
HEMOLYTIC ANEMIA
- Increased rate of red cell destruction
- Increased rate of production - increased
reticulocytes - Red cell destruction causes increased bilirubin
production and jaundice - Most red cell destruction occurs in spleen
- splenectomy may cause improvement
3
Hemolytic anemia low hematocrit, plasma too
yellow due to high bilirubin
4
INHERITED HEMOLYTIC ANEMIA
Sickle cell anemia
- Mutation changes structure of hemoglobin
- Mutant hemoglobin (deoxy form) polymerizes in
cells and damages cell membranes - membrane damage causes hemolysis
- hemoglobin crystals change cell shape to "sickle"
- sickled cells are rigid and block small blood
vessels, causing tissue damage - Genetics mainly affects those of African and
Middle Eastern descent recessive inheritance
(carriers partially protected from malaria)
O2
Sickled cell
5
SICKLE CELL ANEMIA
Sickle cell
Normal
6
Sickle Cell
Normal red cell
Sickle cells inflexible, cant do this
7
Sickle cell anemia - pathophysiology
8
Retinal vessel occlusion in sickle disease
9
IMMUNE HEMOLYTIC ANEMIA
- Production of "autoantibodies" against one's own
red cells - Antibodies coat cells and lead to destruction in
spleen and liver - Positive Coombs test (detects antibodies on red
cells) in most cases - Treatment corticosteroids, splenectomy, i.v.
gamma globulin
10
TRANSFUSION REACTION
- Giving a person blood of the wrong type may cause
destruction of the transfused cells (hemolysis)
by antibodies in the recipient's blood - The most serious reactions occur with blood
mismatched for antigens in the ABO system - giving O patient A, B, or AB blood
- giving A patient B or AB blood
- giving B patient A or AB blood
- In such instances there may be very rapid
hemolysis accompanied by shock, kidney failure,
bleeding, and death
11
HEMOLYTIC DISEASE OF THE NEWBORN
- Caused by maternal antibodies against antigens on
fetal red cells (usually Rh antigens) mother
usually exposed (sensitized) to Rh antigen during
prior pregnancy - These antibodies cross the placenta and cause
destruction of fetal red cells - Infant liver unable to properly metabolize
hemoglobin breakdown products (bilirubin) - Stillbirth or anemia, jaundice, and brain damage
may result - Prevention prevent sensitization by giving
antibody against Rh factor (Rhogam) to
Rh-negative woman soon after delivery of
Rh-positive child
12
POLYCYTHEMIA
- Definition increased total red cell volume
- high hematocrit
- thick blood can cause thrombosis, other
circulatory disorders - Polycythemia vera increased, unregulated red
cell production - Most cases due to an acquired mutation in marrow
cells that makes red cell precursors much more
sensitive to erythropoietin - Secondary polycythemia increased erythropoietin
production due to decreased oxygen delivery to
kidney - Often due to low levels of oxygen in the blood
13
NEUTROPHIL DISORDERS
- Neutropenia (decreased neutrophils)
- Decreased production (bone marrow failure, cancer
chemotherapy) - Increased consumption (some infections, enlarged
spleen, autoimmune) - Increased risk of infection when neutrophil count
low - Neutrophilia (increased neutrophils)
- Increased production due to physiologic stimuli
(e.g., infection) - Increased production due to bone marrow neoplasm
14
10/31/97
11/7/97
2/12/98
neutrophils 0
neutrophils 19,000
neutrophils 1200
15
CANCERS OF THE BLOOD AND LYMPHATIC SYSTEMS
16
LEUKEMIA
- Malignant proliferation of white cells and/or
their precursors (blasts) - Myelogenous (neutrophil precursors)
- Acute myelogenous leukemia (AML)
- Chronic myelogenous leukemia (CML)
- Lymphocytic
- Acute lymphocytic leukemia (ALL)
- Chronic lymphocytic leukemia (CLL)
- Chronic leukemias more mature cells,
slow-growing - Acute leukemias immature cells (blasts),
fast-growing
17
PATHOPHYSIOLOGY OF LEUKEMIA
- Bone marrow failure (marrow fills with leukemic
cells) - anemia
- neutropenia (infections)
- thrombocytopenia (bleeding)
- Leukemic cells in blood may impair circulation
- Leukemic cells in other organs
- spleen, lymph nodes
- skin
- brain
- Toxic substances from leukemic cells
- uric acid (gout, kidney failure)
- proteolytic enzymes (tissue damage, bleeding)
18
White cells
Leukemia
19
GUM INFILTRATION IN ACUTE LEUKEMIA
20
SKIN INFILTRATION IN ACUTE LEUKEMIA
21
CEREBRAL HEMORRHAGE IN ACUTE LEUKEMIA
22
PURPURA IN LEUKEMIA
23
DISSEMINATED FUNGAL INFECTION IN ACUTE LEUKEMIA
24
ACUTE LEUKEMIAS
- Acute myelogenous leukemia (AML)
- adults gt children
- fatal if untreated
- remission, occasional cure possible with
intensive chemotherapy - sometimes curable with bone marrow transplant
- Acute lymphocytic leukemia (ALL)
- children and adults (most common childhood
leukemia) - fatal if untreated
- curable with chemotherapy or bone marrow
transplantation - Cure rates in children gt 75
25
DIFFERENTIATION OF NEUTROPHILS AND RED CELLS
26
Bone marrow in acute leukemia
Normal
AML
27
Immature cells (blasts) in acute myelogenous
leukemia
Mature lymphocytes in chronic lymphocytic leukemia
28
CHRONIC LEUKEMIAS
- Chronic myelogenous leukemia (CML)
- rare in children
- treatable but often fatal within 5-10 years
- Newer treatments will probably improve the
prognosis - may be curable with bone marrow transplantation
- Chronic lymphocytic leukemia (CLL)
- almost all patients middle-aged and older
- treatable but incurable
- not all patients need treatment, many live gt 10
years
29
Enlarged lymph nodes (lymphadenopathy) in chronic
lymphocytic leukemia
30
LYMPHOMAS
- Cancer of lymphocytes or their precursors
- Forms tumors in lymph nodes, spleen, bone marrow,
other organs - Sometimes in blood - overlap with lymphoid
leukemia - Many different kinds - spectrum of severity
- Hodgkin's vs non-Hodgkin's
- B-cell vs T-cell
- Mature vs immature lymphoid cells
- Fast vs slow-growing
- Usually treatable, sometimes curable
(chemotherapy, radiation, marrow transplantation)
31
NON-HODGKIN'S LYMPHOMAS
Many types, complex classification scheme
- LOW GRADE
- Cells appear mature
- Good news slow-growing - patients may live many
years with disease - Bad news treatable but generally incurable
- Usually affect older people
- HIGH GRADE
- Cells less mature
- The most aggressive forms resemble acute
lymphoblastic leukemia - Good news often curable with chemotherapy
- Bad news faster-growing, fatal in months if not
treated or treatment doesn't work - Some varieties occur in children
- Example Burkitt lymphoma (resembles acute
leukemia) - Rule of thumb the less mature the cancer cell,
the faster growing the lymphoma, and the more
likely the disease is to affect younger people
and to be curable
32
HODGKIN'S DISEASE
- Probably a cancer of lymphocytes (lymphoma)
- Almost always begins in lymph nodes
- Spreads gradually to other lymph nodes organs
- stage extent of spread
- Relatively common in young adults
- Curable in many cases with radiation or
chemotherapy
Reed-Sternberg cell characteristic of Hodgkins
disease
33
HODGKINS DISEASE
Staging
- Stage I single lymph node or contiguous group
of nodes - Stage II more than one node group, same side of
diaphragm - Stage III confined to nodes (and/or spleen) but
present on both sides of diaphragm - Stage IV spread outside nodes (liver, bone
marrow, lung, etc) - Presence of symptoms (fever, weight loss, night
sweats) designated by "B" after stage (no
symptoms "A") - Lower stage disease often treated with
radiotherapy higher stage disease with
chemotherapy
34
HODGKINS DISEASE Response to treatment
Before treatment
After 6 months (Treatment completed)
After 7 years
35
MULTIPLE MYELOMA
- Cancer of plasma cells (antibody-producing cells)
- Most patients have monoclonal immunoglobulin
(antibody-like protein) in blood or urine - This protein may damage kidneys, other organs
- Bone destruction, bone marrow failure common
36
MULTIPLE MYELOMA
Red cells stuck together by abnormal protein
(rouleaux)
Plasma cell
37
BONE LESIONS IN MYELOMA