Quinolones PowerPoint PPT Presentation
1 / 34
Title: Quinolones
1
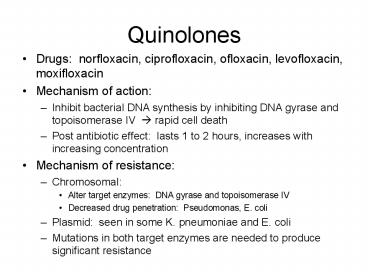
Quinolones
- Drugs norfloxacin, ciprofloxacin, ofloxacin,
levofloxacin, moxifloxacin - Mechanism of action
- Inhibit bacterial DNA synthesis by inhibiting DNA
gyrase and topoisomerase IV ? rapid cell death - Post antibiotic effect lasts 1 to 2 hours,
increases with increasing concentration - Mechanism of resistance
- Chromosomal
- Alter target enzymes DNA gyrase and
topoisomerase IV - Decreased drug penetration Pseudomonas, E. coli
- Plasmid seen in some K. pneumoniae and E. coli
- Mutations in both target enzymes are needed to
produce significant resistance
2
Quinolones
- Parent drug nalidixic acid
3
Classification
- Quinolones (1st generation)
- Highly protein bound
- Mostly used in UTIs
- Fluoroquinolones (2nd, 3rd and 4th generation)
- Modified 1st generation quinolones
- Not highly protein bound
- Wide distribution to urine and other tissues
limited CSF penetration.
4
(No Transcript)
5
Mechanism of Action
- Dual MOA
- Inhibition of bacterial DNA Gyrase (Topoisomerase
II) - Formation of quinolone-DNA-Gyrase complex
- Induced cleavage of DNA
- Inhibition of bacterial Topoisomerase IV
- Mechanism poorly understood
- Mechanism of DNA Gyrase
6
Mechanism of Action
7
Quinolones
- Conc gt serum
- Prostate tissue
- Stool
- Bile
- Lung
- Neutrophils
- Macrophages
- Kidneys
- Conc lt serum
- Prostatic tissue fluid
- Bone
- CSF
8
Quinolones
- Drug interactions
- ? absorption Al3, Mg2, and Ca2 antacids
- CYP450 inhibition potential drug interactions for
ciprofloxacin - (Ex) can increase warfarin exposure (real changes
in INR are rare, but monitor) - Adverse effects
- GI Nausea, vomiting
- CNS HA, dizziness, confusion, insomnia,
delerium, hallucinations, seizure (rare) - Cardiovascular Torsades de pointes (rare)
- Musculoskeletal Rupture of tendon (rare)
- Neurologic Polyneuropathy (rare)
9
Quinolones PK/PD
- Bactericidal antibiotics
- Show both time-dependent and a combination of
time-dependent and concentration dependent
killing - Time-Dependent vs.
Concentration-Dependent Killing
10
Ciprofloxacin
- Administration Usual Dosage IV, PO 500 750
mg q 8-12h - Spectrum Gram- aerobic rods, and Legionella
pneumophila, and other atypicals. Poor activity
against Strep. pneumoniae. - Indications
- -- Nosocomial pneumonia
- -- Intra-abdominal infections
- Uncomplicated/complicated UTI
- Anthrax exposure and prophylaxis
- Unique Qualities
- Binds divalent cations (i.e. Ca Mg) which
decreases absorption - -- Increased effects of warfarin
- ADRs
- QTC prolongation, torsades de pointes,
arrhythmias - Nausea, GI upset
- Interstitial nephritis
11
Levofloxacin
- Brand Name Levaquin, Quixin
- Administration Usual Dosage IV, PO and
ophthalmic 500-750 mg q24h - Spectrum Gram-, Gram (S. aureus including MRSA
S. pneumoniae) and Legionella pneumophila,
atypical resp. pathogens, - Mycobacterium tuberculosis
- Indications
- Chronic bronchitis and CAP
- -- Nosocomial pneumonia
- SSTIs
- Intra-abdominal infections
- Unique Qualities
- Binds divalent cations (i.e. Ca Mg) which
decreases absorption - ADRs
- Blood glucose disturbances in DM patients
- QTC prolongation, torsades de pointes,
arrhythmias - Nausea, GI upset
- Interstitial nephritis
12
Moxifloxacin
- Brand Name Avelox, Vigamox
- Administration Usual Dosage IV, PO and
ophthalmic 400mg q24h - Spectrum Gram-, Gram (S. aureus including MRSA
S. pneumoniae) atypicals (L. pneumophila, C
pneumonia M. pneumoniae), Mycobacterium
tuberculosis, gram-negative anaerobes - Indications
- Chronic bronchitis
- CAP
- Bacterial conjuctivitis
- Sinusitis
- Unique Qualities
- Binds divalent cations (i.e. Ca Mg) which
decreases absorption - Safety and efficacy not established in patients
lt18 y.o. - ADRs
- Blood glucose disturbances in DM patients
- QTC prolongation, torsades de pointes,
arrhythmias - Nausea, GI upset
- Interstitial nephritis
13
Resistance Mechanisms
- Mutations that enhance antibiotic efflux
capability - Bacterial chromosomal mutations for genes that
encode for bacterial DNA gyrase and Topo IV - Mutations in outer membrane porins (Gram-)
14
Metronidazole
- Mechanism of action
- Enters bacteria via cell diffusion
- Activated via single reduction step by bacteria?
forms radicals ? reacts with nucleic acid ? cell
death - Spectrum of activity
- Anaerobic bacteria
- Microaerophilic bacteria
- Protozoa
- Resistance
- Rare
- Mechanism decreased activation (? redox
reaction) of drug
15
Metronidazole
- Indications
- Anaerobe infections
- C. difficile
- H. pylori
- Bacterial vaginosis
- Trichomonas vaginitis
- Amebiasis
- Giardiasis
- Drug interactions
- EtOH
- Antacids
- CyA/tacrolimus
- Lithium
- Phenytoin
- Rifampin
- Warfarin
Dose can vary by indication
16
Metronidazole
- Distribution into tissue
- Therapeutic levels
- PMNs
- Unobstructed biliary tract
- Pancreas
- CSF
- Empyema fluid
- Peritoneal fluid
- Hepatic abscess
- Pelvic tissues
- Vaginal/seminal fluid
- Adverse Effects
- GI N, V, epigastric distress
- Metallic taste
- Darkening of urine
- Peripheral neuropathy
- Pancreatitis
- Hepatitis
- Fever
- Reversible neutropenia
17
Tetracyclines
- Broad-spectrum activity
- Includes aerobic G and G-, atypicals Rickettsia
spp, treponema spp, chlamydia spp, and others - Little to no effect on fungi or viruses
- Tetracycline
- Doxycycline
- Minocycline
- Tigecycline
www.3dchem.com
18
Mechanism of Action
- Passive diffusion
www.solvo.com
19
Mechanism of Action
- Once inside the cell
- Bind 30S ribosomal subunit
- Blocks binding of aminoacyl-tRNA to acceptor site
on mRNA-ribosome complex - Protein synthesis is inhibited bacteriostatic
effect
http//genomebiology.com/content/figures/gb-2003-4
-12-237-1.jpg
20
Tetracycline
- Dosing
- Adult 250 - 500 mg PO q6h
- Peds 25 - 50 mg/kg/d q6h
- Food and milk decrease absorption about 50
- Administer at least 1-2 hours prior to or 4 hours
after antacid or vitamins due to chelation Al3,
Mg2, Ca2, Fe2
www.wikipedia.org
www.3dchem.com
21
Tetracycline
- Dosage forms
- Capsule 250, 500 mg
- Tablet 250, 500 mg
- Suspension 125 mg/5 mL
- Adverse Effects
- Photosensitivity
- Discoloration of teeth
- N/V/D
- Candidal superinfection
- Hepatotoxicity
22
Tetracycline - Special Populations
- Pregnancy
- Category D
- Enters breast milk
- Renal insufficiency
- CrCl 50-80 mL/min every 8-12 hours
- CrCl 10-50 mL/min every 12-24 hours
- CrCl lt10 mL/min every 24 hours
- Hepatic insufficiency
- Avoid use
- If necessary, maximum 1g/day
23
Doxycycline
- Dosing
- Adults 100-200 mg/day in 1-2 divided doses PO or
IV - Peds gt 45 kg use adult dosing
- lt 45 kg 2-5 mg/kg/day in 1-2 divided doses.
Max. 200 mg/day - Give with meals to decrease GI upset
- Take with water and sit up for 30 minutes to
avoid esophageal irritation
http//www2d.biglobe.ne.jp/chem_env/chem8/doxycyc
line.gif
http//sitemaker.umich.edu/mc9/files/doxycycline.j
pg
24
Doxycycline
- Dosage forms
- Capsules
- Hyclate, monohydrate 50, 100 mg
- Coated pellets 75,100 mg
- Variable release 40mg - 30 immediate and 10
delayed - Injection 100 mg
- Suspension 25mg/5mL
- Tablet
- Hyclate 100 mg
- Monohydrate 50,75,100 mg
- Delayed-release coated pellets 75,100 mg
- Adverse Effects
- Discoloration of teeth
- Diarrhea
- Rash
- Photosensitivity
- Urticaria
25
Doxycycline - Special Populations
- Pregnancy
- Category D, but use in pregnancy and
- Use in children single 5-7 day course for RMSF
is safe - Renal Insufficiency
- No adjustment necessary
26
Tigecycline
- Dosing
- Adults initial dose of 100 mg. Maintenance dose
50 mg q12h x 5-14 days. - FDA indications complicated SSTIs and
intraabdominal infections
http//www.wyeth.de/images/packshot_tygacil_thumb.
jpg
http//www.rxlist.com/cgi/images/tygacil1.gif
27
Tigecycline
- Dosage forms
- Injection 50 mg
- Administration
- Infuse over 30-60 mins through dedicated line or
via Y-site. - Stable in D5W or NS
- Adverse Effects
- N/V/D
- Hypertension
- Edema
- Hypotension
- Headache
- Rash
- Pruritus
- Local irritation
28
Tigecycline - Special Populations
- Pregnancy
- Category D
- Not recommended - crosses placenta
- Renal Insufficiency
- No dosage adjustment required
- Hepatic Impairment
- Severe initial dose 100 mg followed by 25 mg q12h
29
Tigecycline
- Aerobic and facultative gram negative organisms
- Citrobacter freundii
- Enterobacter cloacae
- Escherichia coli
- Klebsiella species
- Anaerobic organisms
- Bacteroides species (including fragilis)
- Clostridium perfringens
- Peptostreptococcus micros
30
Tigecycline
- Distribution
- Gall bladder, Colon, Lung gt Serum
- Bone, Synovial fluid lt Serum
- Elimination
- Mostly feces/biliary excretion (59)
- Some excretion in urine (33)
- Adverse Effects (incidence)
- Nausea (29.5)
- Vomiting (19.7)
- Diarrhea (12.7)
- Local reaction (9.0)
31
TMP/SMX
- Good activity against Gr () and Gr (-)
organisms MRSA, very active against PCP.
Covers Stenotrophomonas maltophila, Nocardia, and
enteric gram-negative rods. - Exceptions Pseudomonas aeruginosa, Group A
strep, enterococcus, Gr (-) anaerobes. - MOA Sulfamethoxazole interferes with bacterial
folic acid synthesis and growth via inhibition of
dihydrofolic acid formation from
para-aminobenzoic acid trimethoprim blocks the
production of tetrahydrofolic acid by inhibiting
the enzyme dihydrofolate reductase. - Use with caution in pts with severe G6PD
deficiency - Toxicity GI upset, rash can progress to SJS and
TEN, thrombocytopenia, leucopenia, hepatitis
hyperkalemia - SMXTMP is a 51 ratio, in oral and IV dosage
forms. - 10-20 mg/kg (of TMP) daily, in 2 to 4 divided
doses (q 6 h) for PCP, Nocardia,
Stenotrophomonas, GNR DS 2 BID for MRSA.
32
Colistin (polymyxin E)
- MOA binds to lipopolysaccharide on outer cell
wall of GNR permeability change in cell
envelope leakage of cell content. - Formulation, IV colistimethate hydrolyzed to
colistin. - PK/PD negligible oral absorption, predominant
renal elimination concentration-dependent
activity.
33
Colistin
- Spectrum aerobic gram-negative rods, including
Acinetobacter, Ps. aeruginosa, Stenotrophomonas. - NOT active against Burkholdaria, Proteus,
Serratia, Brucella, gram-negative anaerobes,
gram-positive cocci - Adverse effects ATN Neurotoxicity dizziness,
weakness, vertigo, visual changes, confusion,
ataxia.
34
Colistin
- Dosing regimens (poorly defined)
- 2.5 to 5 mg/kg/day in 2-4 doses
- For SCr 1.3 1.5 160 mg q 12h
- SCr 1.6 2.5 160 mg q 24 h
- SCr gt 2.6 160 mg q 36 h
- Hemodialysis Load with 160 mg, then 80 mg after
each dialysis.