Results of using a systemic model to introduce vasectomy services in Guatemala
Title:
Results of using a systemic model to introduce vasectomy services in Guatemala
Description:
Results of using a systemic model to introduce vasectomy services in Guatemala. Ricardo Vernon ... in Zone 19 of Guatemala was the most successful unit ... –
Number of Views:61
Avg rating:3.0/5.0
Title: Results of using a systemic model to introduce vasectomy services in Guatemala
1
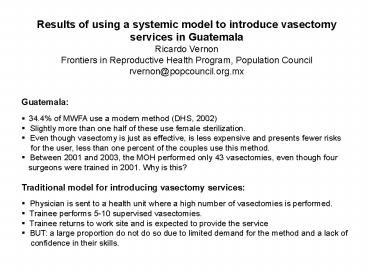
- Results of using a systemic model to introduce
vasectomy services in Guatemala - Ricardo Vernon
- Frontiers in Reproductive Health Program,
Population Council - rvernon_at_popcouncil.org.mx
- Guatemala
- 34.4 of MWFA use a modern method (DHS, 2002)
- Slightly more than one half of these use female
sterilization. - Even though vasectomy is just as effective, is
less expensive and presents fewer risks - for the user, less than one percent of the
couples use this method. - Between 2001 and 2003, the MOH performed only
43 vasectomies, even though four - surgeons were trained in 2001. Why is this?
- Traditional model for introducing vasectomy
services - Physician is sent to a health unit where a high
number of vasectomies is performed. - Trainee performs 5-10 supervised vasectomies.
2
- Systemic model for introducing vasectomy
- In this project we tested a systemic model for
introducing vasectomy in MOH hospitals and - maternities. The model had four basic components
- Self-selection of health units according to the
response to an invitation to participate in the
project - The development of a counseling and information
model for potential clients - Training and sensitizing of health teams
- On-site training of surgeons
- Self-selection of health units according to the
response to an invitation to - participate in the project
- We invited 15 hospitals and maternities to
participate in the project. - To start training activities, we required that
they identify at least one man interested in
3
- Development of a counseling and information model
for potential clients - We developed three printed materials a poster,
a leaflet and a brochure. - We requested vasectomy acceptors to identify and
inform friends and relatives about - the method.
- We requested that clients attending health
facilities are informed about vasectomy - We asked providers to always offer vasectomy as
an alternative for all women - interested in a permanent method.
- We asked providers to always mention vasectomy
in family planning talks to women - who just had a birth and in family planning
counseling sessions. - Training and sensitizing of health teams
- We conducted one-half day sessions with all the
staff in the six hospitals /maternities that - identified at least one vasectomy candidate
- We also conducted these sessions in two or
three health centers near the hospital, so - that they functioned as referral centers.
- In the sessions, we explained what a vasectomy
was and trained them to implement the
4
- On-site training of surgeons
- Surgeon training was carried out in two stages
- One-half day theoretical training
- Supervised practice sessions in their own
health units with the vasectomy candidates - identified by their health teams.
- Once the hospital team identified at least
three candidates for vasectomy, a vasectomy - trainer visited the hospital and trained the
surgeon in the service. - The trainer repeated visits until he reported
the trainee could provide services without - supervision and until the trainee reported
feeling confident to do the vasectomies without - supervision.
5
Table 1. Average of no-scalpel vasectomies by
place and number of sessions
6
Table 2. Number of no-scalpel vasectomies per
hospital, surgeon, certification time and
sessions before and after certification
7
- Effectiveness of Promotion Strategies
- 68 consulted their wives and 41 said they had
been the most influential person in - making the decision
- Health providers were the source of information
for 31 and the most influential - source for 9.
- Friends and relatives were a source of
information for 21 of men and the most - influential source for 6.
- However, 81 said they knew a vasectomized man.
- 46 said they had made the decision on their own
without any influence. - 53 were exposed to the projects brochure and
poster - 29 received information from their wives,
8
- Effectiveness of Promotion Strategies (continues)
- The maternity in Zone 19 of Guatemala was the
most successful unit in generating - patients.
- Maternity director and nurse auxiliary
attributed their success to daily family planning
talks - for women who had just delivered a baby.
- Health providers highlighted the importance of
operating on Friday after 1100 a.m., - (easier for men to rest/ only one-half day
off work)
9
Characteristics of the 158 clients that had a
vasectomy during the project
10
- Decision-Making Process
- We asked how long it took them from first
hearing about vasectomy until they decided to - get an operation 56 said they less than
two months, 13 said two months 14 3-6 - months
- 92 discussed with partner whether vasectomy or
female sterilization was a more - convenient method.
- 65 chose vasectomy to protect their partners
health or because a doctor recommended - it. Significant proportions mentioned
advantages of vasectomy over female sterilization - (greater safety, greater effectiveness, quick
recovery, refusal of wife to have an operation.
11
- Cost Analysis
- The total cost per trained surgeon was 4,335
dollars or 274 per surgery performed. - If we do not include the costs of the time of
the personnel trained (but including the - time of coordinators, instructors and
supervisors), the cost per trained surgeon would - be 2,930 and 185 per vasectomy performed.
- If we take into account the MOHs salary
structure and the per-diem and travel - expense scale, the total cost of the project
would be 29,204 and 17,571 without - taking into account the time of personnel
still being trained. - The projects most expensive component was the
training of health teams in 30 health - units (nearly US 20,000). If only the teams
from the six vasectomy service delivery - units were trained, these costs would be
reduced by 80. This component should be - eliminated.
- The theoretical and practical training of
surgeons was relatively inexpensive
12
- Cost Analysis (continues)
- Promotion and information costs were about
400 per participant center, including time - used by nurses, as well as IEC materials.
- If the MOH were to replicate the introduction
strategy, the costs would be lower given - that the MOHs salary structure and
per-diem. - We believe the MOH could replicate training at
an approximate cost of US 900 per - surgeon, including post-certification
follow-up costs and promotion costs, but
decreasing - costs related to training health teams in
nearby health centers. - These costs would decrease as the number of
trained surgeons increases and the - methods popularity rises.