Motor dysfunction: motor unit PowerPoint PPT Presentation
1 / 32
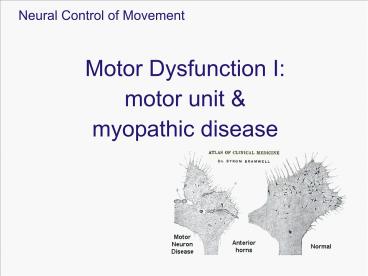
Title: Motor dysfunction: motor unit
1
(No Transcript)
2
Motor dysfunction motor unit myopathic disease
- Learning objective
- To understand and describe
- Myopathic and neurogenic disorders
- Four examples of motor dysfunction Muscular
dystrophy, Amyotrophic Lateral Sclerosis (ALS),
Multiple Sclerosis, Cerebral Palsy
3
Motor dysfunction
Characteristic of the disease depends on the
specific component of motor unit
affected. Different clinical implications for
different sources of disease. Myopathic
problems with the muscle Neurogenic problems
with the motor neuron and pre-motor neuron
4
Characteristics of the disease
Nerve cell body motor unit disease (1) Motor
neuron axon/neuromuscular junction peripheral
neuropathy (23) Muscle degeneration myopathy
(4)
5
Neurogenic vs Myopathic diseases
Criteria for distinguishing neurogenic (cell body
axon) versus myopathic (muscle)
diseases. Myopathic main symptom muscular
weakness/wasting (atrophy) leads to
difficulty walking, lifting, etc. also
myotonia, myalgia, cramps Neurogenic diseases
have these characteristics also, but also ...
tendon reflexes lost gradual weakening
fasciculations (visible muscle twitches)
6
Upper and Lower motor neurons
Each produces distinctive symptoms
7
Neurogenic vs Myopathic diseases
Normal muscle
Denervated muscle
Myopathy
Neurogenic and myopathic diseases have different
effects on the motor unit.
8
Neurogenic vs Myopathic diseases
Normal muscle
Denervated muscle
Myopathy
EMG activity during rest, slight contraction, and
maximum contraction to distinguish between
neurogenic and myopathic diseases.
9
Neurogenic vs Myopathic diseases
Biopsy results show histochemistry differences in
the muscle fibres
Type I and II fibres usually equal distributed
randomly
Neuropathy can see size changes, clustering
Myopathy can see damage
10
Neuropathies symptom mechanisms
Motor neuron disease affects motor neurons
leaving sensory neurons intact Peripheral
neuropathies affect sensory and motor
functions often have paresthesias (numbness,
tingling, etc) May be categorized as
demyelinating or axonal demyelinating
more common
11
Demyelination
Record action potentials after simulating the
motor nerve at two distances to determine
conduction velocity.
12
Demyelination
Leads to slowing of conduction velocity In
partially demyelinated nerve fibers, the action
potentials propagate less efficiently.
13
Demyelination
Nerves with different amounts of myelin (normal
or partial) will conduct at different velocities,
so lose synchrony of
conduction.
Can lead to reflex problems and odd sensations.
insulation loss
14
Demyelination Causes
Viral certain viruses can affect motor nerves
selectively (e.g. poliomyelitus) Neonatal
hypoxia (e.g. cerebral palsy) Genetic (e.g.
muscular dystrophies) Unknown (e.g., multiple
sclerosis)
15
Case 1 Duchenne Muscular Dystrophy
Description Genetic disorders characterized by
progressive muscle wasting and weakness that
begin with microscopic changes in the
muscle. Shows signs of muscle weakness as early
as age 3. The disease gradually weakens the
skeletal or voluntary muscles, esp. those in the
arms, legs and trunk. By the early teens, the
heart and respiratory muscles may also be
affected.
16
Case 1 Duchenne Muscular Dystrophy
Symptoms (boys only) Children with the disorder
are often late in learning to walk clumsy,
unsteady gait, difficulty raising arms, walk on
toes lose the ability to walk sometime between
ages 7 12 in teen years, activities
involving the arms, legs or trunk require
assistance or mechanical support
17
Case 1 Duchenne Muscular Dystrophy
Muscle hypertrophy enlarge muscles, esp the
calf increases with age most commonly due
to muscle fibrosis
18
Causes of Duchenne Muscular Dystrophy
An absence of dystrophin, a protein that helps
keep muscle cells intact. Dystrophin strengthens
muscle cells by anchoring elements of the
internal cytoskeleton to the surface membrane.
19
Causes of Duchenne Muscular Dystrophy
Without it, the cell membrane becomes permeable,
so that extracellular components enter the cell,
increasing the internal pressure until the muscle
cell "explodes" and dies.
20
Case 2 Amyotrophic Lateral Sclerosis
Amyotrophic neurogenic muscle atrophy, Lateral
sclerosis hardening of lateral corticospinal
tracts Description Upper and lower motor neuron
disease Motor neurons undergo shrinkage, caused
by altered cytoskeleton they innervate less
and less musculature, and those muscles atrophy
Mean onset age 56-63
21
Case 2 Amyotrophic Lateral Sclerosis
Symptoms Initially, muscle weakness and
stiffness Usually the first muscles affected are
those in the hands, arms and legs. (lateral CS
tracts) Speech problems, such as slurring,
hoarseness, or decreased volume may also occur
(dysarthria)
22
Case 2 Amyotrophic Lateral Sclerosis
Symptoms Motor neuron signs (normal sensation)
atrophy, hyperactive MSR, hyper/hypotonia,
Babinskis sign, spasticity, fasciculations. Event
ually, the ability of the brain to start and
control voluntary movement is lost.
23
Case 2 Amyotrophic Lateral Sclerosis
Causes Exact causes of the neural degeneration
is unknown 5 to10 can be attributed to
heredity there are multiple genes in which, if
mutated, may cause ALS Suspects viruses,
neurotoxins , heavy metals, DNA defects
(especially in familial ALS), immune system
abnormalities, and enzyme abnormalities
24
Case 2 Amyotrophic Lateral Sclerosis
Treatment Motor deficits only. Sensory and
cognitive function intact Treatment focuses on
relieving symptoms and maintaining an optimal
quality of life Medications for spasticity,
discomfort, pain Physical therapy for cramping,
contractures
25
Case 3 Multiple Sclerosis
Description Myelin is lost in multiple areas,
leaving scar tissue called sclerosis. damaged
areas are also known as plaques or lesions
sometimes the nerve fiber itself is damaged or
broken MS is a chronic, unpredictable
neurological disease The majority of people with
MS dont become severely disabled.
26
Case 3 Multiple Sclerosis
Symptoms Wide range of unpredictable symptoms,
vary from person to person, time to time can
affect vision, speech, balance, bladder function,
coordination may cause dizziness, pain, and
tremors Age onset peaks between 20 30
years Most people with MS are diagnosed between
the ages of 20 and 50. Women twice as likely
to get it
27
Case 3 Multiple Sclerosis
Causes It is believed that MS is an autoimmune
disease myelin is attacked. Unknown what
triggers the improper autoimmune
reaction Several factors are involved Genetics
Gender Environmental Triggers, possibilities
include viruses, trauma, and heavy metals
28
Case 3 Multiple Sclerosis
Treatment In the past, steriods have been used
to reduce the duration and severity of attacks in
some patients, or the symptoms such as
spasticity. Some of the FDA-approved drug
treatments include Synthetic protein (Glatiramer
Acetate or Copaxone) used to simulate myelin
basic protein (acts as a decoy) Mitoxantrone
suppress attack (e.g. from T-cells) on the myelin
sheath.
29
Case 4 Cerebral Palsy
Description (not a disease, actually) A
non-progressive medical condition that affects
control of the muscles, muscle tone Cerebral
means anything in the head and palsy refers to
anything wrong with control of the muscles or
joints in the body
30
Case 4 Cerebral Palsy
Different types Spastic (high tone),
50 Ataxic (low tone) 25 Athetoid (mixed
tone) 25 Movement symptoms depend on type
affects limbs, face, mouth, head Learning
disabilities in 25-50 of CP children slower
rate of learning Seizures in about 50 of children
31
Case 4 Cerebral Palsy
Causes Injury to the brain before, during, or
shortly after birth. In many cases, not sure
what caused the brain injury or what could have
prevented the injury. - Neonatal/perinatal
insufficient oxygen (hypoxia) and/or insufficient
blood (ischemia) is a major cause of damage to
the newborn infants brain - Prenatal maternal
infection or accident, maternal medical condition
such as high blood pressure or diabetes
32
Case 4 Cerebral Palsy
Treatments Exercise and its favourable impact
factors Cardio-pulmonary condition- ing, muscle
strength building and coordination. Therapies P
hysical, recreational, speech,
occupational Adapted objects, communication
mobility aids