Cost-Effectiveness Problem - PowerPoint PPT Presentation
Title:
Cost-Effectiveness Problem
Description:
Cost to payer (employer, HMO, insurance) Health to patient pool. Social ... Life-saving interventions become less cost-effective in the elderly, who are net ... – PowerPoint PPT presentation
Number of Views:30
Avg rating:3.0/5.0
Title: Cost-Effectiveness Problem
1
Cost-Effectiveness Problem
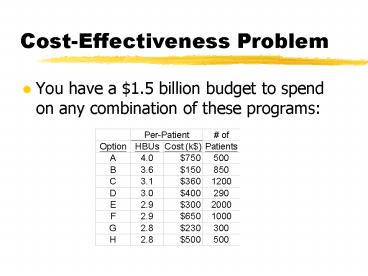
- You have a 1.5 billion budget to spend on any
combination of these programs
2
Issue Limited Resources
- Assumption Theres not enough money to fund
every effective treatment (screening program,
etc.) - Goal Get the most health for our money. How can
we allocate our fixed budget to provide the most
health care?
3
Answer Cost-Effectiveness
- Determine how much health per dollar each
intervention provides - its cost-effectiveness
and how many of these interventions are needed - Fund interventions in decreasing order of
cost-effectiveness until the budget is spent.
4
Cost-effectiveness
- Fund I,B,G,E,C,D, and H for 291
patients15,374.8 HBUs (3.06 per 5031 people)
5
Effectiveness only
- Result Fund A-D and E for 1498
patients13,994.2 HBUs (3.21 per 4338 people)
6
Perspective
- Patient perspective
- Cost to patient (may be 0 due to insurance)
- Health to patient
- Payers perspective
- Cost to payer (employer, HMO, insurance)
- Health to patient pool
- Social perspective
- Cost to society, including lost productivity
- Health to society
7
Measuring Costs
- Costs are usually measured in dollars, adjusted
for inflation over time. - Costs differ from charges, which include profits,
market effects, etc. - Costs should include future related medical costs
and savings. Future costs are discounted
8
Future Costs
- Some argue that costs should include all future
costs and savings (wages, etc.) If you do this - Life-extending interventions become less
cost-effective than life-enhancing interventions,
because youre usually extending low-quality
life. - Life-saving interventions become less
cost-effective in the elderly, who are net
consumers, than in the young, who are net
producers.
9
Benefit, Effectiveness, Utility
- Cost-benefit analysis Benefit in dollar
units (e.g. willingness to pay for result) - Cost-effectiveness analysis Benefit in health
units (e.g. AIDS cases prevented, lives saved) - Cost-utility analysis Benefit in utility
(quality-of-life) units (e.g. QALYs)
10
Measuring Effectiveness
- The recommended measure for cost-effectiveness is
the quality-adjusted life year, a common unit for
comparison. - QALYs ? (time in state utility of state)
- 1 year of life in perfect health is as good as 2
years of life in 0.5 utility health. - Under 50,000 or 100,000/QALY is widely regarded
as cost-effective
11
Graphing the CE Ratio
12
CEA problem 2From Stinnett Paltiels CEA short
course
You must choose which of 5 mutually exclusive
programs to fund. You currently fund option A.
Considering your other decisions, youre willing
to spend up to an additional 200,000 per QALY.
13
Marginal CEA(aka Incremental CEA)
- What if we have to weigh programs against each
other, or determine if a new treatment is better
to give than the current standard? - Marginal CEA focuses on how much more health
could we get by spending an additional amount
14
CEA Problem 2
Step 1 Order the programs by cost. If some
option costs more and delivers less than another,
eliminate it from consideration.
15
CEA Problem 2
Step 2 Calculate a marginal CE ratio for each
program, relative to the one above it.
16
CEA Problem 2
Step 3 Eliminate any program that has a higher
marginal CE ratio than the program below it.
If youd spend 571k more to get 17.1 more QALYs,
instead spend 175k more to get 17.9.
17
CEA Problem 2
Step 4 Recalculate marginal CE ratios and choose
the program that has the largest marginal CE
ratio thats less than the threshold CE ratio
(200,000).
In this case, neither C nor E meets our
threshold. We should continue to fund A.
18
CEA GuidelinesThe Panel on Cost-Effectiveness in
Health and Medicine (1993)
- 1. Reference case analysis
- Societal perspective (resource allocation)
- Compare interventions with status quo
- Use QALYs based utilities on community
preferences, not patient preferences - Use direct and indirect costs, but need not
include unrelated future health and non-health
costs. Discount costs at 3. - 2. Perform sensitivity analysis
19
Conclusions
- Cost-effectiveness analysis asks how to spend a
fixed budget for the most health - The cost-effectiveness of an intervention is
usually reported as its cost-per-QALY ratio. - Interventions with lower /QALY are more
cost-effective and should be preferred to
interventions with higher /QALY
















![[Dental Implants Cost] PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/3840011.th0.jpg?_=201909240612)













