Periodontal Overview - PowerPoint PPT Presentation
1 / 85
Title:
Periodontal Overview
Description:
Recalls decrease tooth loss in patients with severe periodontitis. ... Clinical Evaluation of Subgingival Debridement with Ultrasonic Instruments Used ... – PowerPoint PPT presentation
Number of Views:647
Avg rating:3.0/5.0
Title: Periodontal Overview
1
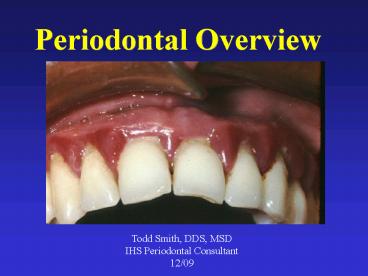
Periodontal Overview
Todd Smith, DDS, MSD IHS Periodontal
Consultant 12/09
2
All IHS, Tribal, and Urban Dental Programs should
provide
- Access to diagnosis for all individuals,
demonstration of appropriate self care behavior
and discussion of individual needs. - An explanation of what the individual can do for
him/herself. - An explanation of what can be done (what is
available) at the clinic and what needs to be
referred out.
3
Detecting Periodontitis
4
(No Transcript)
5
(No Transcript)
6
(No Transcript)
7
Detecting Periodontitis
- Conventional methods
- Visual changes
- Radiographs
- Mobility
- Probing depths and attachment levels
- Others
- Enzymes- GCF or saliva
- DNA/RNA probes
- Cytokines
8
Do you use the who probe?
9
(No Transcript)
10
(No Transcript)
11
(No Transcript)
12
(No Transcript)
13
(No Transcript)
14
(No Transcript)
15
(No Transcript)
16
(No Transcript)
17
(No Transcript)
18
(No Transcript)
19
(No Transcript)
20
CPITN- Whats the sextant score?This is the
worst finding.
CPITN 3?
CPITN 0
0, 1, 2, 3, or 4?
21
What is the periodontal diagnosis?
22
Localized gingivitis in a 30 y.o. male?
Generalized severe aggressive periodontitis
23
Post periodontal surgical recession
24
Pre and Post Scaling Root Planing
2, 3, and a couple 4mm pockets. No calculus or
bleeding.
4 5mm pockets
CPITN 3
CPITN ?
CPITN 3
25
Indicators of periodontal disease
- Visual redness or swelling of papilla/gingiva
- Bleeding on probing
- Calculus
- Pockets
- Mobility
- Furcation involvement
- Recession
- Loss of attachment
- Radiographic bone loss
26
Function of Probe
- Findings from an examination with a periodontal
probe are used to determine the health of the
periodontal tissues. - Used like miniature rulers for making intraoral
measurements
27
Millimeter Markings
- The working-end of a probe is marked in
millimeter intervals. - There are many different patterns of millimeter
markings.
28
Markings at Each Millimeter
- The UNC 15 probe has millimeter markings at 1, 2,
3, 4, 5, 6, 7, 8, 9, 10. 11, 12, 13, 14, and 15
millimeters
29
Markings at Certain Intervals
- This probe has millimeter markings only at
certain intervals. - Marks are found at 1, 2, 3, 5, 7, 8, 9, and 10 mm.
30
Color-Coded Probe
- Marked in bands with each band being several mm
in width - This example is marked at 3, 6, 9, and 12 mm.
31
Probe in Periodontal Pocket
- A probing depth deeper than 3 mm indicates a
periodontal pocket.
32
IHS-514
33
Missing Teeth
34
Probing Depths
35
Recession
0
4
6
2
36
Furcations
Grade I
Grade III
Grade II
37
(No Transcript)
38
Mobility
39
Recording
40
Spot probing as an alternative
Spot probing takes no additional time while
doing the CPITN.
Might as well use the IHS 514 for this sextant.
41
(No Transcript)
42
Bone levels lower anterior incisors?
43
Actual bone levels
44
Horizontal BW
45
Horizontal BW
46
Periodontal Diagnoses and Etiology
47
Periodontal Diagnoses
- Gingivitis- bleeding gums, generally with no
attachment or bone loss - Chronic periodontitis -usually slowly progressive
disease with loss of gum attachment and bone. - Severity
- Slight- 3-4mm pockets, up to 30 bone loss
- Moderate 4-6 mm probings, up to 50 bone
loss Severe gt 6mm probings, gt50 bone loss - Extent
- Localized lt 30 of sites involved. Generalized gt
30 - Aggressive Periodontitis- Highly destructive,
with rapid attachment loss and bone destruction,
usually affecting patients under age 30 years of
age. - Extent
- Localized lt 30 of sites involved. Generalized gt
30
48
Other Periodontal Diagnoses
- Abscesses of the periodontium
- Perio-endo lesions
- Necrotizing ulcerative gingivitis and
periodontitis - Perio as a manifestation of systemic disease
- Rare genetic and blood disorders (cyclic
neuropenia, histiocytosis, leukemia) - Developmental or acquired deformities
- Mucogingival deformities or conditions around
teeth i.e. recession, limited or no
gingiva, high frenums, gingival overgrowth - Occlusal trauma- primary and secondary
Generally,90-95 of diagnoses will be gingivitis
or chronic perio!
49
Classify by Location, Severity, Type, and Disease
Location Severity Type of Disease Generalized
Moderate Chronic Periodontitis Localized
Severe Acute Gingivitis Localized
Severe Necrotizing Periodontitis Generalized
Severe Chronic Periodontitis, treated, on recall
50
Initiation and Progressionof Periodontitis
- Periodontitis is initiated by specific bacteria
that activate a series of inflammatory and
immunologic changes leading to destruction of
connective tissue and bone.
51
Bacterial interactions- tooth and sulcus
52
Bacterial interactions- biofilm complexes
53
Localized mild chronic periodontitis
54
Generalized severe aggressive periodontitis. Less
than 3 years later.
55
Pathway to Periodontal Disease
Genetic Risk Factors
Antibody
Cytokines
PMN
Connective Tissue and Bone Metabolism
Host Immuno- inflam-matory Response
Antigens
Clinical Signs of Disease
Microbial Challenge
Prostanoids
LPS
Other Virulence Factors
MMPs
Environmental AcquiredRisk Factors
Tissue Breakdown Products Ecological Factors
After Kornman, 1997.
56
The Nature of Periodontal Disease
- Periodontitis does not affect all people and all
areas of the mouth similarly. There is great
variation among people and among teeth within the
same mouth. - Periodontitis does not necessarily progress
steadily over the years if left untreated.
57
At Periodontal Risk
- Smokers and Diabetics
- Early onset perio disease- chronic or aggressive
periodontitis - Genetic factors
- Stress Immunocompromised individuals
- Certain medications
- Anatomic considerations
- Obese individuals
- Nutritional factors
- Alcohol
58
Anatomic considerations in perio risk
- Cervical enamel projections
- Furcations
- Palatogingival grooves
- Short roots and fused roots
- Root surface roughness
- Concavities/flutings
- Horiz vs. angular bone loss
59
Rams et al AAP ab 96
Angular bone defects more frequently developed
periodontitis recurrence than sites with horiz
bone loss. The presence of a crestal lamina dura
is asso. with clinical stability for up to 30
months.
60
Diabetic with severe periodontitis
61
- Epidemiologic Studies in the Pimas
Shlossman, Emrich,
Knowler, and others - Diabetics had more severe periodontitis than
non-diabetics. - Destructive periodontitis occurred much earlier
in life in the diabetics (27 of diabetics 15-19
years old). - Diabetics were 15X more likely to lose all their
teeth.
62
(No Transcript)
63
Diabetic protocol in those with moderate to
severe periodontitis
- Intensive OHI
- 1/2 mouth ultrasonic SRP with LA
- In deep pockets until bony resistance is felt
- Extract hopeless teeth
- Antibiotic
- Doxy 100mg bid X 14 or 21 days
- CHX mouthrinse
- Analgesic
- Recall 2-6 months
64
Initial Therapy- Lower anterior
65
Recall- Lower anterior
66
8 y.o. with Gen. Severe Aggressive Periodontitis-
LAD
67
Localized Aggressive Perio (LJP) in a 16 y.o.
female
68
Nifedipine induced gingival overgrowth
69
The Relationship BetweenPeriodontitis and
Systemic Disorders
- Diabetes
- Atherosclerosis, stroke, and heart disease
- Pregnancy outcomes
- Lung disease
- Infective endocarditis
- Late prosthetic joint infection
- Others RA, Alzheimers, cancer
70
PUBLIC HEALTH IN PERIODONTICS
71
(No Transcript)
72
Public Health in Periodontics
- Target to those at high risk for periodontitis
- Self efficacy- its their job to control disease
with good home care - Treat them before advanced periodontitis occurs
- Provide individualized recall when appropriate
73
Goals of Treatment
- Arrest active disease
- Prevent additional loss of attachment
- Prevent recurrence
- Preserve a functional and comfortable dentition
74
Supragingival
Subgingival Plaque
Therapy Control
Can
Halt the Progression of Periodontitis
Kornman
The Basics of Periodontal Therapy
Supragingivasl plaque control reduces subgingival
bacteria. Gomes 2008
75
Recalls decrease tooth loss in patients with
severe periodontitis.Recalls are more important
for tooth preservation than plaque
scores.Patients who didnt comply with recalls
were more than 5X more likely to have tooth loss.
Checci 2002
Preventing Tooth Loss
Recall intervals can be extended beyond 6 months
for low risk patients.
Mettes 2005
76
Perio Definitions
Scaling Removal of plaque and calculus from the
crown and root surfaces of teeth. Prophy Removal
of plaque and coronal calculus using ultrasonic
and/or hand instruments. Normally reported for
patients with CPITNs of 2 or less. Root
planing Removal of plaque, embedded calculus,
and altered cementum from the root surfaces.
Normally reported for patients with CPITNs of 3
or 4. Periodontal debridement Treatment of the
root surface, pocket space, pocket wall, and
underlying tissue using ultrasonic and/or hand
instruments.
77
Clinical Evaluation of Subgingival Debridement
with Ultrasonic Instruments Used by Trained
and Untrained Operators
- Results
- After minimal training with an ultrasonic
scaler, dental assistants were as efficient in
removing subgingival calculus as dentists and
hygienists.
Dragoo Wheeler, Gen Dent 1996
78
TEAMWORKin the treatment of periodontitis
- Who is going to scale this patient?
79
Establishing and Maintaining Perio Healthin
I/T/U Dental Clinics
- Hygienist/s able to meet the need.
- Regular recalls provided
- DDS- Exam and Treatment Plan, Perio Tx?
- RDH- OHI, Perio Tx, and recall
- DA- TB prophy, OHI
80
Establishing and Maintaining Perio Healthin
I/T/U Dental Clinics
- Hygienist/s unable to meet the need.
- Targeted recalls provided
- DDS- Exam and Tx Plan, Perio Tx of severe cases
requiring extractions - RDH- OHI, Perio Tx of moderate to severe cases,
and those recalls - DA- Gingivitis to mild perio (CPITN 1,2,3),
select gross debridements, prophys, and recalls.
81
Establishing and Maintaining Perio Healthin
I/T/U Dental Clinics
- No hygienist
- Targeted recalls provided
- DDS- Exam and Tx Plan, Perio Tx of moderate to
severe cases and their recalls. - DA- Gingivitis to mild perio (CPITN 1,2,3),
select gross debridements, prophys, and select
recalls.
82
(No Transcript)
83
Treatment Planning
- Medical and Dental History
- Initial Therapy
- Palliative therapy/Tx of acute pain
- Perio
- Restorations
- Endo
- Extractions
- Occlusion
84
Treatment Planning
- Re-evaluation
- Extractions
- Perio Surgery
- Ortho
- Pros
- Recall/ SPT
85
Periodontal Treatment
- Risk factor reduction
- Diet
- Oral hygiene motivation
- Smoking cessation
- Blood sugar control
- Risk profile assessment
- Medical history
- Medications
86
Periodontal Treatment
- Eliminate infection
- Mechanical- ultrasonics and curets
- Surgical
- Topical antimicrobials - gels, chips, spheres
- Systemic antimicrobials - antibiotics
- Modulate the host response
- Local- Emdogain, GFs, BMP
- Systemic- NSAIDS, enzyme suppressors, immune
system enhancers
87
Perio Hygiene for the 21st Century Therapeutic
Endpoints Gutter 2005
- Consistent absence of bleeding in all sites
- Pockets dont get deeper
(and no further
attachment loss) - Gingival collar tightens around the tooth
- Minimal volatile sulfur compounds.
- This is accomplished through
- Root treatment with bactericidal ultrasonic
debridement. - Use of local antibiotics in deep pockets
- Use of low dose doxycycline in nonresponders
- Use of systemic antibiotics in nonresponders.
88
Questions? Gregory.Smith3_at_ihs.gov











![STN 125011 Tositumomab Therapeutic Regimen (TTR) [tositumomab plus I-131 tositumomab] PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/7258373.th0.jpg?_=20151013059)


















