ABSTRACT PowerPoint PPT Presentation
1 / 1
Title: ABSTRACT
1
Association Between Low Blood Pressure and
Cognitive Function in Late Life The
Honolulu-Asia Aging Study.
Gina Fujikami, MSIV Kamal Masaki, MD Randi
Chen, MS Irwin Schatz, MD Danielle Laurin, PhD
Robert Abbott, PhD G. Webster Ross, MD Helen
Petrovitch, MD Lon White, MD, MPH Patricia
Lanoie Blanchette, MD, MPH Lenore Launer,
PhD. The research reported on this poster was
supported by The Hawaii Medical Student Aging
Research National Training Center (National
Institute on Aging, John A. Hartford Foundation
and American Federation for Aging Research
grant), Department of Geriatric Medicine, John A.
Burns School of Medicine, University of Hawaii,
Pacific Health Research Institute, Honolulu
Department of Veteran Affairs, National Institute
on Aging, National Heart, Lung, and Blood
Institute. The investigators retained full
independence in the conduct of this research.
METHODS
RESULTS
METHODS
ABSTRACT
CONCLUSIONS
METHODS
Introduction Hypertension in mid-life is a
strong predictor of subsequent dementia. The
relationship between blood pressure (BP) in late
life and cognitive function is less understood,
especially for low BP. We studied the association
between low BP and cognitive function over 6
years. Methods The Honolulu-Asia Aging Study
began in 1991-93, when 3734 Japanese-American men
ages 71-93 years were administered the Cognitive
Abilities Screening Instrument (CASI). CASI
scores ranged from 0-100, and 3-year and 6-year
cognitive decline were defined as a drop in score
of gt10 or gt14 points, respectively (1 SD). BP
was measured by standard manometer and mean of
two readings was used. Subjects were divided into
4 groups for systolic (SBP) lt120, 120-139,
140-159, and 160 mmHg and 3 groups for
diastolic (DBP) lt80, 80-89, and 90 mmHg.
Analyses used chi square, GLM, logistic
regression, mixed models for change in CASI and
Cox proportional hazards models. Results The
prevalence of dementia was 6, and an additional
10 had cognitive impairment (CASI lt74).
Prevalent dementia and cognitive impairment were
more common in low SBP (lt120 mmHg) and low DBP
(lt80 mmHg) groups (plt0.0001). Multiple logistic
regression analyses adjusting for age, education,
apoE4, stroke, diabetes and smoking found that
low SBP was significantly associated with
prevalent dementia (OR2.70, 95 CI1.68-4.35,
plt0.0001), with normal SBP (120-139) as
reference. Those with low SBP were more likely to
have prevalent Alzheimers Disease (OR2.20, 95
CI1.04-4.66, p0.04), but not vascular or
mixed/other dementias. Multivariate models found
no association between low SBP or low DBP and
cognitive decline or incident dementia over 6
years. Those with low SBP had significantly
higher rates of prevalent CHD, stroke and
functional impairment, suggesting that the
association with prevalent dementia may be due to
chronic disease rather than causal. Conclusion
Low SBP in late life had a significant
association with prevalent dementia and
Alzheimers Disease, but not cognitive decline or
incident dementia. Those with low BP were
significantly sicker and no longer reflected a
healthy group of elderly subjects.
- The Honolulu Heart Program (HHP)
- Began in 1965 to study cardiovascular diseases in
8,006 Japanese-American men living on Oahu,
Hawaii - Ages 45 to 68 years at baseline (born 1900-1919)
- 42-year longitudinal follow-up with serial
examinations, review of hospital and death
records - The Honolulu-Asia Aging Study (HAAS)
- Began with the fourth HHP examination (1991-93)
to study cognitive function and other diseases of
aging - 3,734 men ages 71-93 years examined (80 of
survivors) - Follow-up at 3 years (exam 5, 1994-96) and 6
years (exam 6, 1997-99) for cognitive decline and
dementia - Cognitive Abilities Screening Instrument (CASI)
- A comprehensive measure of global intellectual
function - Developed for use in cross-cultural and
cross-national studies to test 9 cognitive
domains - Scores range from 0-100, higher scores are better
- Outcomes
- Cognitive impairment No Dementia (CIND) CASI lt74
- 3-Year cognitive decline (3Y CD) Drop in CASI gt
10 points (1 SD) 541/2693 (20.1) - 6-Year cognitive decline (6Y CD) Drop in CASI gt
14 points (1 SD) 409/1982 (20.6) - Dementia DSM III/R criteria
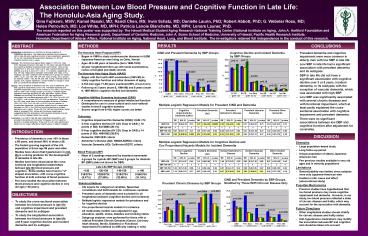
CIND and Prevalent Dementia by SBP Groups
Cognitive Decline and Incident Dementia by SBP
Groups
- Prevalent dementia and cognitive impairment were
more common in elderly men with low SBP in late
life. - Low SBP in late life had a significant
association with prevalent dementia and its
subtypes. - SBP in late life did not have a significant
association with cognitive decline over 3 or 6
years, incident dementia, or its subtypes with
the exception of vascular dementia, which was
associated with high SBP. - Low SBP was significantly associated with several
chronic diseases and with functional impairment,
which at least partly explained the
cross-sectional association with cognitive
impairment and prevalent dementia. - There were no significant associations between
low DBP and cognitive function after adjustment
for covariates.
Multiple Logistic Regression Models for Prevalent
CIND and Dementia
Cognitive Impairment No Dementia (CIND) Cognitive Impairment No Dementia (CIND) Cognitive Impairment No Dementia (CIND) Prevalent Dementia (All) Prevalent Dementia (All) Prevalent Dementia (All) Prevalent Alzheimers Disease Prevalent Alzheimers Disease Prevalent Alzheimers Disease Prevalent Vascular Dementia Prevalent Vascular Dementia Prevalent Vascular Dementia Prevalent Other Dementia Prevalent Other Dementia Prevalent Other Dementia
OR 95 CI p-value OR 95 CI p-value OR 95 CI p-value OR 95 CI p-value OR 95 CI p-value
SBPlt120 1.41 0.89-2.26 0.15 2.70 1.68-4.35 lt0.0001 2.20 1.04-4.66 0.04 0.77 0.20-2.97 0.71 2.53 0.42-15.3 0.31
SBP 120-139 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1
SBP 140-159 0.81 0.58-1.12 0.21 1.01 0.67-1.52 0.98 0.98 0.53-1.79 0.94 0.57 0.24-1.38 0.21 1.02 0.23-4.57 0.98
SBPgt160 0.64 0.46-0.89 0.008 0.62 0.41-0.95 0.03 0.42 0.21-0.84 0.01 0.64 0.29-1.41 0.27 0.45 0.07-2.78 0.39
RESULTS
INTRODUCTION
- Prevalence of dementia is over 10 in those gt 65
years, and almost 50 in those gt 85. - The fastest growing segment of the U.S.
population is those age 85 years and older. - Studies have shown that hypertension in mid-life
is a strong predictor for the development of
dementia in late life. - Studies have been mixed about the cross-sectional
and longitudinal relationships between late life
blood pressure and cognition. Some studies have
found a U shaped association, with worse
cognitive function at both extremes of blood
pressure. - Few have studied the association between blood
pressure and cognitive decline in very old age (gt
80 years).
Multiple Logistic Regression Models for Cognitive
Decline and Cox Proportional Hazards Models for
Incident Dementia
- Strengths
- Large population-based study
- Long follow-up period
- Unique population of elderly Japanese- American
men - Few previous studies available in very old ages
and in minority populations - Limitations
- Generalizability was limited, since subjects were
only Japanese-American men - Unable to infer cause and effect (observational
study) - Possible Mechanisms
- Previous studies have hypothesized that low blood
pressure may cause cognitive impairment and
dementia. However, in our study, low blood
pressure reflected a state of chronic disease and
frailty, which may account for the association
with dementia. - Future Directions
- Other longitudinal studies should stratify for
chronic disease and frailty status - Anti-hypertensive medications may modify the
association between BP and cognition and should
be taken into account
6-Year Cognitive Decline 6-Year Cognitive Decline 6-Year Cognitive Decline Incident Dementia (All) Incident Dementia (All) Incident Dementia (All) Incident Alzheimers Disease Incident Alzheimers Disease Incident Alzheimers Disease Incident Vascular Dementia Incident Vascular Dementia Incident Vascular Dementia Other Incident Dementia Other Incident Dementia Other Incident Dementia
OR 95 CI p-value RR 95 CI p-value RR 95 CI p-value RR 95 CI p-value RR 95 CI p-value
SBPlt120 1.21 0.74-1.97 0.45 1.11 0.60-2.05 0.73 1.48 0.72-3.02 0.29 0.82 0.10-7.10 0.86 0.57 0.13-2.50 0.45
SBP 120-139 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1
SBP 140-159 1.02 0.75-1.38 0.90 1.0 0.69-1.44 0.99 0.87 0.54-1.41 0.32 0.96 0.48-1.95 0.92 0.96 0.48-1.95 0.92
SBPgt160 1.19 0.88-1.61 0.27 0.83 0.56-1.23 0.35 0.47 0.27-0.84 0.01 3.63 1.36-9.67 0.01 0.59 0.27-1.30 0.19
Late Life SBP Groups (mmHg) Late Life SBP Groups (mmHg) Late Life SBP Groups (mmHg) Late Life SBP Groups (mmHg)
lt120 120-139 140-159 gt 160
316/3734 (8.47) 1029/3734 (27.59) 1216/3734 (32.60) 1169/3734 (31.34)
CIND and Prevalent Dementia by SBP Groups,
Stratified by Those WITH Chronic Disease Only
Prevalent Chronic Diseases by SBP Groups
- Statistical Methods
- Chi square for categorical variables, Spearman
correlations and GLM models for continuous
variables - Prevalent cases of dementia were excluded for all
longitudinal analyses (cognitive decline and
incidence) - Multiple logistic regression models for
prevalence and for cognitive decline - Cox proportional hazards models for incidence
- All multivariate models were adjusted for age,
education, apoE4, stroke, diabetes and smoking
status - Subgroup analyses were performed for those with
or without Prevalent Chronic Diseases (Cancer,
Coronary heart disease, Stroke, Diabetes) or
Functional impairment (FI) (defined as difficulty
walking ½ mile)
OBJECTIVES
- To study the cross-sectional association between
low blood pressure in late life and cognitive
impairment and prevalent dementia and its
subtypes - To study the longitudinal association between low
blood pressure in late life and 6-year cognitive
decline and incident dementia and its subtypes