Case Complexity PowerPoint PPT Presentation
1 / 13
Title: Case Complexity
1
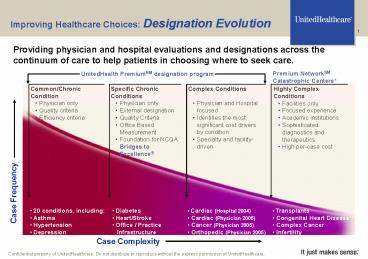
Improving Healthcare Choices Designation
Evolution
Providing physician and hospital evaluations and
designations across the continuum of care to help
patients in choosing where to seek care.
Premium NetworkSM Catastrophic Centers
UnitedHealth PremiumSM designation program
- Complex Conditions
- Physician and Hospital focused
- Identifies the most significant cost drivers by
condition - Specialty and facility-driven
- Specific Chronic Conditions
- Physician only
- External designation
- Quality Criteria
- Office Based Measurement
- Foundation for NCQA Bridges to Excellence
- Common/Chronic Condition
- Physician only
- Quality criteria
- Efficiency criteria
- Highly Complex Conditions
- Facilities only
- Focused experience
- Academic institutions
- Sophisticated diagnostics and therapeutics
- High per-case cost
- Diabetes
- Heart/Stroke
- Office / Practice
- Infrastructure
- 20 conditions, including
- Asthma
- Hypertension
- Depression
- Cardiac (Hospital 2004)
- Cardiac (Physician 2005)
- Cancer (Physician 2005)
- Orthopedic (Physician 2005)
- Transplants
- Congenital Heart Disease
- Complex Cancer
- Infertility
Case Complexity
2
Program Philosophy
There is a significant desire today on the part
of many stakeholders in health care to increase
the availability and utility of assessment
information regarding the quality and efficiency
of clinical care delivery. The UnitedHealth
PremiumSM Designation program is a new component
of this effort.
3
The Cost Challenge
Improving the quality of care consumers receive
leads to decreased costs
The Premium NetworkSM Formerly United Resource
Network (URN) - includes Transplantation,
Congenital Heart Disease, Complex Cancer,
High-Risk Pregnancy, Infertility, Neonatology,
Bariatric Surgery, Kidney Disease/Dialysis
- Improved Quality
- Decreased complications, recurrence and
re-operation rates - Improved long term care leading to healthier
employees and better employee productivity - Physicians utilize better standards for testing
and preventive measures - Greater efficiency
Sources Milliman USAs Transplant Report U.R.N.
claims and cost data
4
UnitedHealth Premium Designation Program
Common or chronic conditions affect over 50 of
the patient population (frequency) and drive
substantial health care expense
Designation (quality and/or efficiency)
- Physicians designated for their performance
against certain quality and efficiency criteria,
based on review of claims data - Quality designation based on external criteria,
including use of evidence-based medicine and
national clinical standards - Efficiency criteria based on claims-based
analysis and industry data
There is limited quality data for Pediatrics and
outpatient procedure specialties such as
Dermatology, Ophthalmology, ENT, Urology, etc.,
due to lack of applicability of current evidence
based medicine (EBM) guidelines in these areas.
As such, physicians practicing in these
specialties are not included at this time.
5
UnitedHealth Premium Designation Program
Complex conditions make up nearly 40 of the
total health care spend (cost)
(Quality only)
Complex Conditions
Designations
(Quality Efficiency)
- Physicians and hospitals designated based on
quality and efficiency criteria - Quality criteria based on evidence-based
medicine, expert physician guidance and national
clinical standards - Efficiency criteria based on claims-based
efficiency analysis and industry data - Search physician directory on myuhc.com to find
designated physicians and hospitals
- Cardiac Care
- Cancer Care
- Orthopedic Care
Cardiac hospitals today. Other
facilities/hospitals to come.
6
Sample Physician Report
7
The UnitedHealth Premium Designation Program
A win-win situation for employers, consumers and
physicians
Employers
Consumers
Physicians
- Information for assessing quality across the
entire continuum of care - Potential for
- More healthy and productive employees
- Lower absentee rates
- Providing quality of care information to
enrollees - Confidence in the health care benefits purchased
for employees
- Informed choice- identification of hospitals and
physicians that meet criteria - Educated selection of designated physicians and
specialty centers - Potential for reduced variability in care
- Potential for higher volume
- Broadcasting of their achievements and quality
care - Sharing of best practice information
- Access to peer comparison data
8
Bridges to Excellence (BTE)
BTE is an employer sponsored pay for performance
program that utilizes NCQA physician recognition
programs to drive advances in the quality of care
and reduce waste and inefficiencies through
accountability and financial incentives.
- UnitedHealth Group involvement
- First health care company licensee
- In pilot markets supporting physicians in
achieving NCQA recognition - Discounts, application support, data sharing
- Formal recognition of NCQA involvement
- NCQA recognition designations featured in the
UnitedHealthcare online and print physician
directories - Implemented Boston and Albany
- Pilot Cincinnati, Louisville
- Planned expansions to 5 new markets Omaha, NE,
Dayton, OH, St. Louis, MO, and Miami and Tampa, FL
9
Bridges to Excellence (BTE)
NCQA offers three physician recognition programs
based on demonstrable high quality care and use
of up-to-date information and systems to enhance
patient care
Designations Physician Practice
Heart/Stroke Diabetes
- UnitedHealthcare actively supports NCQA in its
recognition programs - Including identification of physicians in the
physician directory - This NCQA recognition program is the foundation
for Bridges to Excellence (BTE) - BTE is an employer-sponsored financial rewards
program for physicians that seek to drive quality
through the network
10
Employer Perspective
- Employer groups are developing benefit plans
structured to encourage utilization of physicians
with demonstrated performance on nationally
recognized quality and efficiency standards. - The evolution toward consumer driven health care
creates engaged consumers who are informed about
health care choices treatment options and
costs. - Employer groups may offer benefit differentials
to employees when care is received from
physicians designated as high quality, high
efficiency.
The train has left the station
11
This is a Period of Transition in Assessing
Physician Performance
12
THE LEADERSHIP PROJECT
As Consensus is Reached on Industry Standards,
We Will Incorporate Them Into Our Assessment
Program
- Sponsors
- Agency for Healthcare Research Quality
- American College of Physicians
- American Academy of Family Physicians
- Americas Health Insurance Plans
- Goal
- Measuring performance at the physician level
- Collecting and aggregating data in the least
- burdensome manner
- Reporting meaningful information to consumers,
- physicians, and other stakeholders to inform
- choices and improve outcomes
13
Our Focus Is Straightforward and Integrated
Decreasing health care costs
Assisting health professionals to improve
quality, safety, and the appropriate use of
resources
Evaluating performance
Enhancing consumer health decisions
Facilitating the relationship between a patient
and their physician the right care for the
right person, at the right place, at the right
time!