Antimicrobial Stewardship - PowerPoint PPT Presentation
1 / 30
Title:
Antimicrobial Stewardship
Description:
Desrosiers M, et al.: J Otolaryngology 2002; 31(Suppl. 2):2S2-14. ... Bacterial Rhinosinusitis' Supplement to Otolaryngology - Head and Neck Surgery 123 (2000): S20. ... – PowerPoint PPT presentation
Number of Views:241
Avg rating:3.0/5.0
Title: Antimicrobial Stewardship
1
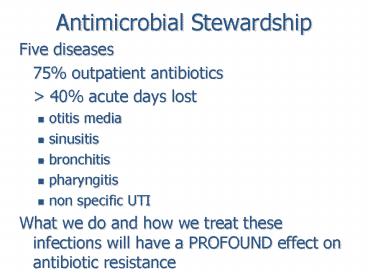
Antimicrobial Stewardship
- Five diseases
- 75 outpatient antibiotics
- gt 40 acute days lost
- otitis media
- sinusitis
- bronchitis
- pharyngitis
- non specific UTI
- What we do and how we treat these infections will
have a PROFOUND effect on antibiotic resistance
2
The major respiratory pathogens
Organism Sinusitis AECB CAP
Streptococcus pneumoniae x x
x Haemophilus influenzae
x x x Moraxella catarrhalis
x x
Mycoplasma pneumoniae!
x Chlamydia pneumoniae!
x Legionella pneumophila
x
Gram positive, Gram negative, No Gram colour!
3
Duration of Coryza Symptoms
4
For every thing there is a seasonCrop rotation
of the coryza viruses
5
Bacteriology of Community Acquired Respiratory
Tract Infections
- CAP AECOPD Sinus (ABRS)
- Organism (1967-2000) (1996-2000)
(1981-2000) - S. pneumoniae 20-60 10-25 20-43
- H. influenzae 3-54 15-50 18-35
- M. catarrhalis 1-21 10-33 2-47
Pathogen distribution in bacterial infections ()
Bartlett and Mundy. N Engl J Med. 19953331618
Sethi and Murphy. Clin Microbiol
Rev. 200114336 Sinus and Allergy Health
Partnership. Otolaryngol Head Neck
Surg. 2004130(Suppl)S1 Pfaller and Jones.
Diagn Microbiol Infect Dis. 20024477
Pfaller et al. Am J Med. 2001111(9A)4S.
6
Bacterial Rhinosinusitis
- Axelson and Runze
- 164 patients 69 items
- Six symptoms more common
- previous VRI
- nasal discharge
- painful mastication
- malaise
- cough
- hyposmia
7
Bacterial RhinosinusitisIs this really
rhinosinusitis?
8
ABRS Current Treatment Recommendations
- First-line antibiotics
- Indications
- Symptoms persisting longer than 7 days and
failing to resolve with symptomatic treatment - Example
- Amoxicillin 500 mg TID
- Despite concerns over antibiotic resistance, most
patients will resolve on first-line agents
Most viral ARS resolve in about 7 days
Desrosiers M, et al. J Otolaryngology 2002
31(Suppl. 2)2S2-14.Piccirillo JF, et al. JAMA
2001 2861849-56.
9
ABRS Current Treatment Recommendations (contd)
- Second-line antibiotics
- Indications
- No clinical response to first-line therapy after
72-96 hours - Frontal or sphenoid sinusitis
- Allergy to beta-lactams
- Patients receiving antibiotics in previous 3
months - Chronic underlying conditions or
immunosuppression - Protracted symptoms
- Second-line antibiotics
- Fluoroquinolones
- gatifloxacin, levofloxacin, moxifloxacin
- Macrolides
- Clarithromycin, azithromycin
- Oral beta-lactams
- amoxicillin/clavulanate
- Cefixime
- Cefprozil
Desrosiers M, et al. J Otolaryngology 2002
31(Suppl. 2)2S2-14.
10
American Academy of Pediatrics
- Acute Otitis Media defined as
- 1) Recent and abrupt onset of
11
America Academy of Pediatrics
- Caveat to observe option Can be seen in
follow-up with option to start antibiotics
12
Severe vs not severe illness
13
2007 Cochrane Review Acute Otitis Media in
infants and young children
- Randomised trials with two arms placebo and
treatment with antibiotics - 10 trials, 2287 children
- 80 pain settles in 48 hours
- 15 children must receive antibiotics to prevent 1
child from having pain at 48 hours - No difference relief 1, 3, 7 or 14 days
- Small differences re crying, use of analgesics
- No difference in mastoiditis or meningitis
- Dutch 4860 children, 1 children developed
mastoiditis, one had on presentation - Kids with antibiotics increase NV, diarrhea
14
Guidelines for the Optimum Treatment of
Community-acquired Pneumonia
IDSA/ATS joint guidelines (2005) - reserve
telithromycin for complicated CAP
15
23 Anti-Bacterial Classes
- IV antibiotics
- Aminoglycosides
- Vancomycin
- Carbapenems (meropenem)
- Streptogramins (synercid)
- Monobactams
- Colistin
- Glycocycline (tigecycline)
- Cyclo lipopeptide
- (daptomycin)
- IV or PO
- Penicillins
- Cephalosporins
- Macrolides
- Ketolides
- Clindamycin
- Metronidazole
- Quinolones
- Sulpha drugs
- Choramphenicol
- Fusidic Acid
- Oxazolidones (linezolid)
- PO
- Nitrofurans (MacroBID)
- Dapsone
- Tetracyclines
- Rifamycins
16
Macrolides Start Gram and work to respiratory
Gram negative
17
Macrolides/lincamycins
Agent with a long half-life
Agent with a short half-life
Concentration
MIC
Selective Pressure
Selective Pressure
Time
Antimicrobial Treatment Guidelines for Acute
Bacterial Rhinosinusitis Supplement to
Otolaryngology - Head and Neck Surgery 123
(2000) S20.
18
Quinolones Start Gram- and work to others
19
Mechanisms of Fluoroquinolone Resistance
DNA gyrase Mutations confer resistance to
moxifloxacin
Gemifloxacin has a high binding affinity for both
gyrA and parC at therapeutic levels
Most fluoroquinolones bind to the 2 enzymes with
varying affinities in different species,
inhibiting DNA replication
Topoisomerase IV Mutations confer resistance to
levofloxacin and ciprofloxacin
Hooper DC. Lancet Infect Dis. 2002 2530-8.
19
20
40
Clarithromycin
35
Epithelial Lining Fluid (ELF)
30
Serum
25
Moxifloxacin
Concentration (?g/ml)
20
15
Levofloxacin
Gatifloxacin
Telithromycin
10
5
Amoxicillin
Ciprofloxacin
Azithromycin
0
1-2
5
6
6
6
6
2
3
4
Time of Sampling Post-dose (hr)
Honeybourne, et al. J Antimicrob Chemother
20014863-66. Morrisey, et al. Int J Antimicrob
Agents 20011733-37.
Following 800 mg qd for 5 days.
21
Eradication of S. pneumoniae by Azithromycin and
Clarithromycin
Susceptible Low Resistance
High Resistance
0.06
2
0.03
1
2
4
8
16
Inoculum vs. Initial
Inoculum vs. Initial
4
8
16
32
64
64
Azithromycin MIC (µg/mL)
Clarithromycin MIC (µg/mL)
In vitro pharmacodynamic model drug
concentration achievable human ELF
concentration at 24 hours
Noreddin AM, et al. Antimicrob Agents Chemother.
2002464029-4034. Zhanel GG, et al. J Antimicrob
Chemother. 20035283-88.
22
What does BC has in common with NF?
Macrolide Resistance
1995
25
2001
20
15
10
5
0
AB
SK
MB
ON
QE
NB
NS
NF
BC
Province
Davidson R et al 13th ECCMID 2003
23
Table 2 Centers for Disease Control and
Prevention criteria for nosocomial pneumonia
Ig Immunoglobulin. Adapted from reference 3
24
Table 3 Microbiological causes of
hospital-acquired pneumonia and
ventilator-associated pneumonia (level A-2)
MSSA Methicillin-susceptible S aureus, MRSA
Methicillin-resistant S aureus. Adapted from
references 11,44-91
25
Table 4Pathogens causing hospital-acquired
pneumonia (HAP) and ventilator-associated
pneumonia (VAP) (level A-2)
Core pathogens include Streptococcus pneumoniae,
Streptococcus species, Haemophilus influenzae,
Enterobacter species, Escherichia coli,
Klebsiella species, Proteus species, Serratia
marcescens and methicillin-susceptible
staphylococcus aureus Risk factors for
resistance include antimicrobial therapy in the
past 90 days and late-onset during
hospitalization (gt5days) Mild to moderate
presentation no hypotension, intubation, sepsis
syndrome, rapid progression of infiltrates or
end-organ dysfunction Severe presentation
hypotension, intubation, sepsis syndrome, rapid
progression of infiltrates or end-organ
dysfunction. MRSA Methicillin-resistance S
aureus. Adapted from references 11,44-91
26
Table 8Clinical pulmonary infection score (CPIS)
chart
Microbiology not relevant in the case of the
modified clinical pulmonary infection score as
described by Farthukh et al (157) Determination
is only positive for the purpose of the
modified clinical pulmonary infection score as
described by Fartoukh et al (157). ARDS Acute
respiratory distress syndrome FiO2 Fraction of
inspired oxygen PaO2 Partial pressure of oxygen
in arterial blood.
27
AECB The agent selected should be potent against
the suspected pathogen(s)
- Etiology of AECB
Sethi S, et al. Ann Clin Microbiol Antimicrob.
2005 45.
28
Proposed Therapies for AECOPD According to
Patient Subsets
Complicated AECOPD at risk for P aeruginosa
Complicated AECOPD
Simple, uncomplicated AECBOPD
- Any age
- lt 4 exacerbations/yr
- No comorbid illness
- FEV1 gt50
- gt64 years
- gt4 exacerbations/yr
- Serious comorbid illness
- FEV1 lt50
- Patients with chronic bronchial sepsis
- Need for chronic corticosteroid therapy and
frequent (gt4/yr) courses of antimicrobials - FEV1 lt35
Macrolide (azithro- mycin, clarithromycin) or
new cephalosporin (cefpodoxime, cefuroxime,
cefdinir), doxycycline
Newer respiratory fluoroquinolone
or amoxicillin/clavulanate
Fluoroquinolone with antipseudomonal activity
(eg, ciprofloxacin)
FEV1 Forced expiratory volume in 1 second.
ODonnell et al. Can Respir J. 200310(Suppl
A)11A.
29
And what do biofilms have to do with Best of Class
- If you have COPD you have a biofilm in your
lungs, the structure is damaged and the bacteria
are always hanging outyou will not kill them
all.. - New events are caused by new strains of H.
influenzae arriving - Go in and settle things down and get out..dont
let the bacteria grow wise - Long half lives are evil here
30
Carriage of Resistant Pathogens 6 Week Post
Macrolide Therapy RCT for kids (6-16 yr) with
URI
85
100
80
60
Percent of Patients ()
40
17
17
20
0
Clarithromycin
Erythromycin
Azithromycin
7.5mg/kg/day BID x 7 days (n60) 13.3mg/kg/day
TID (n12) 10mg/kg/day x 3 days (n60)
Kastner Guggenbichler, Infections in Medicine
2001 29 251-256
31
SCREEN PATIENT FOR SEVERITY OF ILLNESS Does
patient present with one or more of the following
Consider illness to be MILD TO MODERATE
NO
Hypotension Intubation Sepsis syndrome Rapid
progression of infiltrates End organ dysfunction
YES
Determine if patient is at increased risk of
infection with a resistant pathogen Has patient
been hospitalized for ? 5 days and / or been on
antimicrobial therapy in the past 90 days?
Consider illness to be SEVERE
NO
YES
Potential pathogens include CORE pathogens
(Streptococcus pneumoniae, Streptococcus spp.,
MSSA, Haemophilus influenzae, Escherichia coli,
Klebsiella spp., Enterobacter spp., Proteus spp.
and Serratia spp.)
Potential pathogens include CORE pathogens PLUS
MRSA andP. aeruginosa
Potential pathogens include CORE pathogens PLUS
MRSA andP. aeruginosa, Legionella spp.
NO
NO
NO
Is patient intubated?
Is patient intubated?
Is patient intubated?
YES
YES
HAP (Group 3)
YES
HAP (Group 2)
HAP (Group 1)
VAP (Group 5) consider also Legionella
spp., Acinetobacter spp., Stenotrophomonas
maltophilia
VAP (Group 4)
Figure 3.
Clinical Guidelines for HAP/VAP Can J Infect Dis
Med Micro. 200819(1)19-53
32
SCREEN PATIENT FOR SEVERITY OF ILLNESS Does
patient present with one or more of the following
Consider illness to be MILD TO MODERATE
NO
Hypotension Intubation Sepsis syndrome Rapid
progression of infiltrates End organ dysfunction
YES
Determine if patient is at increased risk of
infection with a resistant pathogen Has patient
been hospitalized for ? 5 days and / or been on
antimicrobial therapy in the past 90 days?
Consider illness to be SEVERE
NO
YES
Potential pathogens include CORE pathogens
(Streptococcus pneumoniae, Streptococcus spp.,
MSSA, Haemophilus influenzae, Escherichia coli,
Klebsiella spp., Enterobacter spp., Proteus spp.
and Serratia spp.)
Potential pathogens include CORE pathogens PLUS
MRSA andP. aeruginosa
Potential pathogens include CORE pathogens PLUS
MRSA andP. aeruginosa, Legionella spp.
NO
NO
NO
Is patient intubated?
Is patient intubated?
Is patient intubated?
YES
YES
HAP (Group 3)
YES
HAP (Group 2)
HAP (Group 1)
VAP (Group 5) consider also Legionella
spp., Acinetobacter spp., Stenotrophomonas
maltophilia
VAP (Group 4)
Figure 3.
Clinical Guidelines for HAP/VAP Can J Infect Dis
Med Micro. 200819(1)19-53
33
SCREEN PATIENT FOR SEVERITY OF ILLNESS Does
patient present with one or more of the following
Consider illness to be MILD TO MODERATE
NO
Hypotension Intubation Sepsis syndrome Rapid
progression of infiltrates End organ dysfunction
YES
Determine if patient is at increased risk of
infection with a resistant pathogen Has patient
been hospitalized for ? 5 days and / or been on
antimicrobial therapy in the past 90 days?
Consider illness to be SEVERE
NO
YES
Potential pathogens include CORE pathogens
(Streptococcus pneumoniae, Streptococcus spp.,
MSSA, Haemophilus influenzae, Escherichia coli,
Klebsiella spp., Enterobacter spp., Proteus spp.
and Serratia spp.)
Potential pathogens include CORE pathogens PLUS
MRSA andP. aeruginosa
Potential pathogens include CORE pathogens PLUS
MRSA andP. aeruginosa, Legionella spp.
NO
NO
NO
Is patient intubated?
Is patient intubated?
Is patient intubated?
YES
YES
HAP (Group 3)
YES
HAP (Group 2)
HAP (Group 1)
VAP (Group 5) consider also Legionella
spp., Acinetobacter spp., Stenotrophomonas
maltophilia
VAP (Group 4)
Figure 3.
Clinical Guidelines for HAP/VAP Can J Infect Dis
Med Micro. 200819(1)19-53