Tooth Transplantation - PowerPoint PPT Presentation
1 / 38
Title:
Tooth Transplantation
Description:
The required amount of bone can be estimated by radiograph ... Root formation, thickness of periodontal ligament, root resorption in radiograph ... – PowerPoint PPT presentation
Number of Views:1147
Avg rating:3.0/5.0
Title: Tooth Transplantation
1
Tooth Transplantation
2
Tooth Transplantation
- a viable alternative
- endodontic treatment or extraction ?
- fixed or removable prosthetic treatment is not
ideal treatment in adolescent
3
Why tooth transplantation is successful?
Hertwigs epithelial root sheath
4
Tooth transplantation
- Autogenous transplantation
- Allogeneic transplantation
- Isogeneic transplantation
- Xenegeneic transplantation
5
Tooth autotransplantation
6
Indication
- Sufficient crown space and alveolar bone
- No periapical or periodontal inflammation
- Proximity of the transplant to the socket wall to
assure rapid organization of the clot between the
alveolar bone and the tooth - Excellent oral hygiene, low caries index
7
Tooth autotransplantation
- Transplantation from one region to another
- Transalveolar transplantation
Sagne S. Autotransplantation of teeth Int Dent
J. 1985 35 , 280-283
8
Transplantation from one legion to another
- Transplant from lower 3rd molar to lower 1st
molar - Transplant from upper 3rd molar to upper 1st
molar - Transplant from lower premolar to upper premolar
or upper premolar to lower premolar - Transplant from premolar to upper central incisor
9
Transplant from lower 3rd molar to lower 1st
molar
10
Transplant from lower3rd molar to lower 1st molar
- Most reported cases of autotransplantation
- a result of caries the first molar is frequently
missing or removal in adolescents - Developing third molars are usually available in
adolescents - In a majority of case the rate of success is well
over 95 for an extended period of time
Andreasen et al. 1992
11
Indication for 3rd molar to 1st molar
- Appropriate candidates are adolescent patients
( 13 to 20 years ) - Recent lost or about to lose a permanent first
molar - A suitable third molar
- The roots on the donor tooth developed to the
point of bifurcation ( should be equal to
approximately 3 -4 mm in root length ) - A fully formed crown
12
Indication for 3rd molar to 1st molar
- A suitable third molar
- Complete enamel calcification coincides closely
with development of the bifurcation - The third molar should be no larger than the
first molar it is replacing - Slight of third molar to make it a suitable size
is acceptable - During instrumentation in the removal of the
donor tooth, the vulnerable tooth buds are avoided
13
Surgical technique
1.Mobilization of the transplant
- A mucoperiosteal flap prepared by a sulcular
incision from the mesial of second premolar to
the distal of second molar then extending
distolaterally and no vertical incision, assuring
an excellent blood supply
- It is important that the flap design allow both
adequate surgical field and blood supply
14
Surgical technique
1.Mobilization of the transplant
- The impacted third molar is carefully exposed ,
avoiding any contact of bone-cutting instruments
with the tooth, grasping the crown with forceps
avoid trauma to the root sac
15
Surgical technique
1.Mobilization of the transplant
- The tooth is then luxated, elevated from its
position and gently returned to its position or
maintained in its socket - Leaving the donor tooth in the socket after
luxation will allow it to continue to receive
nutrients and be hydrate while the host site is
being preparation
16
Surgical technique
- Preparation of the host site
- The first molar and interradicular bone are
carefully removed - Amount of cortical bone removed is critical, if
an injudicious amount of bone is removed , there
will not be an adequate bone support
17
Surgical technique
- Preparation of the host site
- The required amount of bone can be estimated by
radiograph - Irrigate and inspected for debris before a trial
positioning of the transplant
18
Surgical technique
- Transplantation and stabilization
- The third molar is carried forward to new socket
- The area of resistance is relieved before seating
the third molar
- The transplant may be stripped to seating but the
roots of the transplantation should not be
scraped or filed
19
Surgical technique
- Transplantation and stabilization
- The occlusion should be carefully examined to be
certain that the opposing teeth will not exert
pressure on the transplant - avoid premature contact
- Infraocclusion about 2 3 mm
20
Surgical technique
- Transplantation and stabilization
- Mucoperiosteal flap is repositioned and suture
- The transplant is splinted in position using 0.14
gauge stainless steel wire - The wire ligation technique used can be figure
eight or circumferential technique
21
Surgical technique
- Transplantation and stabilization
- Additional stabilization of the transplant can be
achieved by gently packing periodontal surgical
dressing such as Coe-Pak around the transplant
and adjacent teeth
22
Postoperative care and follow-up
- Postoperative instructions are the same as those
given following extraction of impacted teeth - After surgery
- 1 day the tooth has retained its new position
- periodontal pack still in good position
- swelling is within acceptable levels
- 7 days stitch off
23
Postoperative care and follow-up
- The patient should be seen at weekly intervals
- At the end of a month the transplant may still be
slightly mobile, but splinting can be removed - Follow-up every month within 6 months
- every 3 month within 2 years
- every year
24
Postoperative care and follow-up
- At each visit should be checked
- The stability of the transplant
- Sulcular depth
- Gingival recession
- Vitality test
- Occlusion
- Root formation, thickness of periodontal
ligament, root resorption in radiograph - Oral hygiene
25
Precautions
- The precaution that help ensure successful
autogenous transplantation are the following - Root development of donor tooth is between 1/3 to
1/2 of the total root - Hertwigs epithelial root sheath is not injured
during surgery - The host site is prepared to avoid injury to the
epithelial root sheath - The patient should be healthy with adequate oral
hygiene - Pulpy foods that might pack into the cervicular
space should be avoided - The patient should consider the procedure
important, keep operative site clean and avoid
trauma from occlusion
26
Transplantation from one legion to another
- Transplant from lower 3rd molar to lower 1st
molar - Transplant from upper 3rd molar to upper 1st
molar - Transplant from lower premolar to upper premolar
or upper premolar to lower premolar - Transplant from premolar to upper central incisor
27
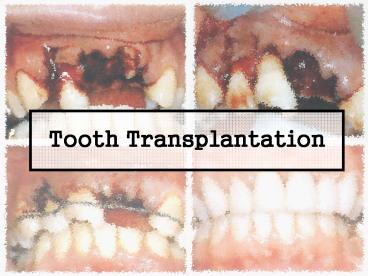
Transplant from premolar to upper central incisor
28
Transplant from premolar to upper central incisor
29
Surgical technique
The treatment plan is to transplant a maxillary
second premolar to the maxillary central incisor
which is to be removed due to root resorption
30
Surgical technique
The maxillary central incisor is extracted
31
Surgical technique
The socket is enlarged with surgical bur The
socket is expanded palatally , then rinse with
saline
32
Surgical technique
Testing the size of socket by a glass replica of
a premolar
33
Surgical technique
Removing maxillary second premolar using gentle
luxation movement
34
Surgical technique
Repositioning of the transplant, it is placed 45?
rotate in order to achieve sufficient cervical
width
35
Surgical technique
Splint the transplant with 0.20 mm stainless
steel wire
36
Surgical technique
Complete treatment, after grinding and restore
with crown
37
Summary
Although it is not possible to perform tooth
autotransplantation in all patients with
nonrestorable molars, it may be a viable
alternative in some instance
38
Reference
Bowden David E. J. et al Autotransplantation of
premolar teeth to replace missing maxillary
central incisor, British Journal of
orthodontics, Vol. 17, 1990 Munksgaard Text
book and color atlas of traumatic injuries to
the teeth, 1994 Plainfield S. et al A viable
alternative Tooth transplantation, Journal of
Prosthodontics, Vol. 50, 1983 Robison J. Peter
and Grossman I. Louis Tooth Transplantation,
Clinical transplantation in dental
specialties Smith J. J. et al Successful
Autotransplantation, Journal of Endodontics,
Vol.13, 2, 1987