RESULTS PowerPoint PPT Presentation
1 / 1
Title: RESULTS
1
The Effect of Low Dose Aspirin on the Risk of
Development of Dyspepsia and Gastrointestinal
Ulcers E Benito-Garcia, Kaleb Michaud and
Frederick Wolfe - National Databank for
Rheumatic Diseases, Wichita, KS
ABSTRACT
RESULTS
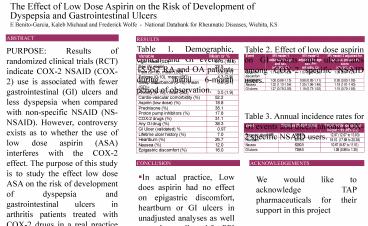
Table 1. Demographic, clinical and GI events in
15,952 RA and OA patients during initial 6-month
period of observation.
Table 2. Effect of low dose aspirin on GI events
and ulcer rates among COX-2 specific NSAID users.
PURPOSE Results of randomized clinical trials
(RCT) indicate COX-2 NSAID (COX-2) use is
associated with fewer gastrointestinal (GI)
ulcers and less dyspepsia when compared with
non-specific NSAID (NS-NSAID). However,
controversy exists as to whether the use of low
dose aspirin (ASA) interferes with the COX-2
effect. The purpose of this study is to study the
effect low dose ASA on the risk of development of
dyspepsia and gastrointestinal ulcers in
arthritis patients treated with COX-2 drugs in a
real practice setting where results might differ
from those obtained in RCT. METHODS Using a
longitudinal data bank, we performed nested case
control studies in patients receiving COX-2
therapy for rheumatoid arthritis or
osteoarthritis to examine the effect of ASA. In 4
separate analyses patients reported dyspeptic
symptoms and GI ulcers at semiannual intervals
for up to three years. Dyspeptic symptoms
included epigastric pain, nausea and heartburn.
At the start of each of the 4 analyses patients
were free of epigastric pain, nauseas, heartburn
and ulcers, respectively. Estimates of the effect
of ASA were performed using COX proportional
hazards regression. For each event of interest we
calculated a separate propensity score for the
risk of low dose aspiring prescription. Among the
variables included in the various propensity
scores were sex, age, pain, prednisone, proton
pump inhibitors, other GI drugs, ulcer history,
COX-2 and non-COX-2 NSAIDs, anxiety, sleep,
fatigue, sleep disturbance and the presence of
cardio-vascular disease. RESULTS 16 of
patients reported epigastric pain. For 4,240
COX-2 () patients without epigastric pain at
study onset, the Hazard Ratio (HR) for the effect
of ASA on the development of epigastric pain was
1.11 (95 CI 0.97 to 1.29) after adjustment for
age and sex. For heartburn, the rate in the data
bank was 27. For 4,240 COX-2 () patients
without heartburn at study start, the age and sex
adjusted HR for the effect of ASA on the
development of heartburn was 1.00 (95 CI 0.88 to
1.15). For nausea, the rate in the data bank was
12, and for the 4,240 COX-2 () patients without
nausea at onset, the age and sex adjusted HR for
the effect of ASA on the development of heartburn
was 1.32 (95 CI 1.13 to 1.54). We also analyzed
the effect of ASA on the risk of developing
ulcers in COX-2 treated patients, restricting
analyses only to ulcers that were completely
validated. The HR in this analysis was 1.27 (95
CI 0.78 to 2.05). These results represent the
risks of therapy as actually experienced in the
study population. Causal models also account for
the factors associated with the risk of
prescription of ASA, in an attempt to control for
confounding by indication and channelling bias.
To obtain insight into the causal relationship
between ASA and GI outcomes, we computed a
propensity score for the risk of ASA prescription
and included it into the analyses described
above. The results for ASA effect became less
significant for all GI variables epigastric pain
(HR 1.05, 95 CI 0.91, 1.21), heartburn (HR 0.95,
95 CI 0.83, 1.09), nausea (HR 1.19, 95 CI
1.01-1.40) and ulcer (HR 1.15, 95 CI 0.70, 1.88).
Table 3. Annual incidence rates for GI events and
ulcers among COX-2 specific NSAID users.
CONCLUSION
ACKNOWLEDGEMENTS
- In actual practice, Low does aspirin had no
effect on epigastric discomfort, heartburn or GI
ulcers in unadjusted analyses as well as analyses
adjusted for PPI use or by a propensity score. - However, low dose aspirin was associated with
nausea with hazard ratios ranging from 1.19 to
1.32. Controlling for low dose aspirin
prescription by propensity score or controlling
for the effect of PPIs only slightly reduced the
effect of low does aspirin. - These risks occur within the setting of prior GI
symptoms, prior GI events and the use of PPI, and
represent the real, practice risk for ASA.
We would like to acknowledge TAP pharmaceuticals
for their support in this project