RHINITIS - PowerPoint PPT Presentation
1 / 107
Title:
RHINITIS
Description:
Affecting 25-30% of the population. Increasing in prevalence ... (tetanus, pertussis, diphteria; alum as adjuvant) Romagnani, 2000. Mast Cell Activation ... – PowerPoint PPT presentation
Number of Views:442
Avg rating:3.0/5.0
Title: RHINITIS
1
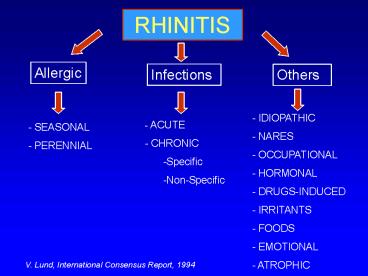
RHINITIS
Allergic
Infections
Others
- IDIOPATHIC
- NARES
- OCCUPATIONAL
- HORMONAL
- DRUGS-INDUCED
- IRRITANTS
- FOODS
- EMOTIONAL
- ATROPHIC
- - ACUTE
- CHRONIC
- Specific
- Non-Specific
- SEASONAL
- PERENNIAL
V. Lund, International Consensus Report, 1994
2
Allergic rhinitis epidemiology
- Heterogenous disorder
- Affecting 25-30 of the population
- Increasing in prevalence
3
Prevalence of allergic rhinitis
Shiffer et al., 1995
4
Prevalence of asthma
Shiffer et al., 1995
5
Indonesia
Indonesia -
- India
India
Albania -
- Estonia
Iran -
- Romania
Panama -
- Portugal
China -
- Latvia
Ethiopia -
- Georgia
Russia -
- Singapore
Spain -
- Italy
Hong Kong -
- Uzbekistan
Costa Rica -
- Marocco
Mexico -
- Korea (South)
Brazil -
- Madeira
Chile -
- Ohman
France -
- Argentina
Canada -
- Germany
Poland -
- Greece
Malaysia -
- Austria
Kenya -
- Nigeria
Japan -
- Belgium
Kuwait -
- New Zealand
Australia -
- Lebanon
USA -
- Pakistan
Finland -
- Sweden
Algeria
- Taiwan
Ireland -
- Thailand
Uruguay -
- U.K.
South Africa -
- Malta
Peru -
- Philippines
Paraguay -
0
10 20 30 40 50
Prevalence of allergic rhinitis ()
6
Prevalence of seasonal allergic rhinitis
(Switzerland)
16
SAR
14
12
10
8
6
4
2
0
1926
1958
1985
1993
Wütrich et al.(SAPALDIA study), 1995
7
Prevalence of asthma (USA)
6,00
Asthma
5,00
4,00
3,00
2,00
1,00
0,00
1980
1981-83
1984-86
1987-89
1990-92
1993-94
Mannino et al., 1998
8
Prevalence of allergic disease in 18 year old
conscripts 1973-1993
9
Allergic rhinitis symptoms
- Inflammation induced by IgE-mediated immune
response to specific allergens pollen, dust
mites, moulds ... - Sneezing
- Itching
- Rhinorrhea
- Nasal obstruction
10
ARIA Classification
Persistent . gt 4 days per week . and gt 4 weeks
Intermittent . 4 days per week . or 4 weeks
- Moderate-severe
- one or more items
- . abnormal sleep
- . impairment of daily activities, sport, leisure
- . abnormal work and school
- . troublesome symptoms
Mild normal sleep no impairment of daily
activities, sport, leisure normal work and
school no troublesome symptoms
in untreated patients
11
Allergic rhinitis mechanisms
- Inflammatory infiltrate made up of different
cells - Chemotaxis, selective recruitment,
transendothelial migration of cells - Localisation of cells within different
compartiments of nasal mucosa - Activation and differentiation of various cell
types
12
Allergic Rhinitis An inflammatory disorder of
the nasal mucosa involving
- Mast cells
- Basophils
- Eosinophils
- T-lymphocytes
- Endothelial cells
- Epithelial cells
- Langerhans cells
13
Cellular Numerical Changes in Allergic Rhinitis
Basophils
Eosinophils
Langerhans
Epithelium
Cells
Mast cells
Lamina propria
Eosinophils
14
Inflammatory process underlying the expression of
allergic rhinitis
- Allergen
mediator release (histamine, tryptase, prostagland
ins, leukotrienes)
symptoms
mast cells
mediator release
Dendritic cell (immune antigen presenting cell)
Tissue recruitment
Endothelial cell activation
T cell
Cytokines (TH2 profile)
Basophils
Eosinophils
B cell
Epithelial cells Chemokine expression
IgE production
15
T-Lymphocytes
- Principal factors for regulation and coordination
of immune responses in allergic diseases - Th1-lymphocytes
- Th2-lymphocytes
16
CD4 T-lymphocyte Cytokines
- TH1
- IL-3
- GM-CSF
- TNF?
- IL-2
- IFN-?
- Lymphotoxin
TH2 IL-3 GM-CSF TNF? IL-4 IL-5 IL-6 IL-10 IL-13
TH0 IL-2 IFN-? IL-4 IL-5
17
(No Transcript)
18
Th1-lymphocytes
- Involved in delayed hypersensitivity immune
reactions - Th1 cytokines
- Activation phagocytes
- Production of opsonizing and complement-fixing AB
by B-Lymphocytes
Romagnani, JACI, 2000
19
Th2-lymphocytes
- Th2 cytokines
- Differentiation, activation and in situ survival
of eosinophils - Stimulate production of AB by B-lymphocytes
- Stimulate growth of mast cells and basophils
Romagnani, JACI, 2000
20
eosinophil
IL-4, IL-13
IL-3, IL-5, GM-CSF
B-cell
GM-CSF
T-cell (Th2)
macrophage
IL-3, IL-4, IL-10
Basophil, mast cell
IgE
Bousquet et al., JACI, 2001
21
- Changes of the commensal flora due to
- - Consumption of semi-steriele foods
- - Use of cleaner water
- Reduced exposure to and/or severity of
- natural infections due to
- - Reduced family size
- - Less crowded accomodation
- - Vaccinations
- - Antimicrobial treatment
- (GERM FREE LIKE STATE)
Risk for atopy
Th2
Th1
- Increased exposure to some allergens (mites,
cat pets, neoallergens) - Th2-biasing
vaccinations (tetanus, pertussis, diphteria
alum as adjuvant)
Romagnani, 2000
22
Mast Cell Activation
Allergen
Ig E
Mediators
Histamine
Tryptase
Prostaglandin D
2
Leukotriene C , D
4
4
Kinins
Cytokines
IL-4
IL-5
IL-6
GM-CSF
TNF
?
23
Nasal Allergen Challenge Lavage
Histamine (nmol)
Time (mins)
24
Mast cells
Chemotactic mediators, Th2 cytokines
Histamine, CysLT, pro-inflammatory cytokines
Other cells
Mucous glands, blood vessels
Nerve stimulation
eos
M?
lymph
Late phase reaction
Hyperreactivity
Bousquet et al., JACI, 2001
25
Basophils
- Absent in normal nasal mucosa
- Demonstrated in nasal mucosa and secretions of pt
with AR - Histamine-containing cell during late-phase
reactions - IL-3 developmental factor
26
The Basophil
Mediators Histamine LTC4/LTD4
Cytokines IL-4 IL-13
27
Eosinophils
H2O2
ECP
MBP
Th2 cytokines
CysLT
PAF
Vasoactive properties
cytotoxic
Enhanced inflammation, decreased apoptosis
Chemo-attractant
Bousquet et al., JACI, 2001
28
The eosinophil
Mediators LTC4 LTD4 PAF
Growth factors TGF-?
Basic proteins ECP EPX MBP
Enzymes Arylsulphatase Histaminase MMP-9
Cytokines/chemokines IL-4 IL-5 RANTES Eota
xin
29
Macrophages / Dendritic cells
- Mucosal environment (place of allergic reaction)
rich in M? and DC - Both significantly increased in the nose in AR
- M? production of growth factors and cytokines
- Langerhans cells important group of DC in AR
- Airway mucosal DC important role in the primary
sensitisation or tolerance to antigens
30
Allergic rhinitis IgE-production
- Allergy overproduction of IgE in response to
common allergens - IgE production complex interaction between
B-cells, T-cells, mastcells and basophils - Involves series of surface molecules as well as
presence of IL-4 and IL-13 cytokines
31
Allergic rhinitis 2 phases
- Early phase
S/ sneezing, itching, clear rhinorrhea (and nasal
congestion) few minutes after exposure Allergen
exposure ? IgE-coated mast cells ? through
epithelium ? recognition antigen ?
degranulation
32
(No Transcript)
33
Late phase
S/ nasal obstruction, sneezing, itching,
rhinorrhea 4 to 8 hours after
exposure Cytokines play more important
role promotion infiltration of mucosa with ?
eosinophils ? neutrophils ? basophil ?
T-lymphocytes ? macrophages
34
Cytokines and Tissue Eosinophilia
Epithelial
cells
GM-CSF
Inhibit
apoptosis
IL-3
T-lymphocytes
IL-5
Weak
GM-CSF
chemotactic
activity
IL-5
GM-CSF
Blood
vessel
Stimulate
Mast cells
progenitor cells
and enhance
Prime eosinophils
maturation
35
Endothelial cell interactions in allergic
inflammation
Endothelial cells
FLOW
Selectins (PE)
Chemokine exposure
ICAM-1 VCAM-1
Rolling margination
Ligand expression
Firm adherence
Diapedesis
36
Tissue cell recruitment
Post capillary venule
Separation of interendothelial pores
Exudation of fluid
Emigration of leucocytes
37
Cell mediators and symptoms of rhinitis
38
Development of Allergic Rhinitis
Structural
Tissue cell
Symptom
Immune
cell
recruitment
development
activation
activation
and activation
Mast cells
Mast cells
Neural and
Endothelial cells
Langerhans cells
Eosinophils
vascular
Epithelial cells
T-lymphocytes
Basophils
interactions
B-lymphocytes
39
Wat is de etiologie van de toename in prevalentie?
- Genetische en familiale factoren
- Risicofactoren in het vroege leven
(prematuriteit, geen borstvoeding,...) - Etnische afkomst (Aziaten in Engeland)
- Aantal broers en zussen, rangorde van het kind
- Buiten- en binnenpollutie
- Roken
- Sociale klasse
40
(No Transcript)
41
(No Transcript)
42
Infection theory
- Infections in early childhood may prevent
allergic sensitisation
43
Allergy and siblings, day-care
30 20 10 7
P0.02
One or no sibling and no day care Two or more
sibling or day care
N 1246 children
P0.02
P0.04
Percentage of Children with Frequent Wheezing
1 2 3 4 5 6 7
8 9 10 11 12 13 14 YEAR
Ball TM et al., 2000
Ball TM et al., 2000
44
Allergy and farm environment
P-value
95 CI
Adjusted OR
P-value
95 CI
Crude OR
Preval.
Total
1.00
1.00
20.8
1248
Rural
lt 0.001
0.50-0.79
0.63
lt 0.001
0.49-0.77
0.61
13.9
1098
Farm
NS
0.92-1.26
1.08
NS
0.95-1.27
1.10
22.4
7307
Urban
Kilpeläinen M et al., 2000
45
Allergy and Hepatitis A
46
Early viral infections may increase allergy
- 1979 Frick et al.
- Anecdotal reports of children who developed
respiratory allergies temporally associated with
URTI - 1988 Holt et al.
- Animal models show that RSV can enhance allergen
sensitisation
47
Early viral infections may increase allergy
- Similar findings
- Chlamydia pneumoniae
- Mycoplasma pneumoniae
- Parainfluenzae virus
48
- Huisstofmijtallergie
- Uiterst kleine spinnen (0.3 mm)
- gtgt Dermatophagoïdes pteronyssinus,
Dermatophagoïdes farinae - Leven van huidschilfers en microscopische
schimmels - Uitwerpselen zijn sterk allergeen
- Leven voornamelijk in beddengoed (donkere, warme,
vochtige plekjes) - Per gram stof 2000 -15000 mijten
- Matras zorgt voor ideale temperatuur en
vochtigheidsgraad
49
(No Transcript)
50
(No Transcript)
51
Co-existence allergic rhinitis and asthma
AR Astma 38 ¹,³ Astma AR 78
¹, 93-99 ²
AR (atopici) Asthma OR 5.7 Rhinitis
(non-atopici) Asthma OR 3.5
1.Corren J Allergy Clin Immunol 1997 2.Kapsali
J Allergy Clin Immunol 1997 3.Scadding Clin Exp
Allergy 1997 4.Plashke Am J Respir Crit Care
Med. 2000
52
Bronchial involvement in allergic rhinitis
- Approximately 40 of patients with rhinitis
present with clinical asthma - Many patients with rhinitis present with
increased non-specific BHR - Endobronchial allergen challenge in rhinitis
patients leads to bronchial symptoms
Braman SS et al. Chest 1987
53
Allergic rhinitis precedes asthma The allergic
march
Populatie Outcome Odds ratio n
7225 Asthma at 7 years 7,1 Anderson UK n
770 Asthma at 5-9 years 2,9 Sherman
USA n 8585 Asthma at 7 years 3,9 Jenkins
Australie n 1021 Asthma
life 3 Settipane USA 23 years folluw-up
54
Allergic rhinitis as a risk factor for the
development of asthma
Incidence of asthma over a 23 year period
Total atrisk
New asthmacases
New asthma
Diagnosis at start of study
Allergic rhinitis 162 17 10.5 No allergic
rhinitis 528 19 3.6
No present or past history of asthma at the time
of original evaluation
plt0.002 comparing the incidence of asthma in the
two subject groups
Settipane G et al. Allergy Proc 1994
55
10-year prognosis for childhood allergic rhinits
(aged 3-17 y)
O Linna, J. Kokkonen, M Lukin 1992
56
Basisprincipes van de diagnose en behandeling van
allergische rhinitis
57
DIAGNOSIS OF AR
SYMPTOMS
- Nasal itching
- Sneezing
- Rhinorrhea
- Nasal congestion
- Conjunctivitis
MEDICAL HISTORY
58
(No Transcript)
59
(No Transcript)
60
EXAMINATION OF THE NOSE
- anatomical structure of the nose
- colour of nasal mucosa
- amount and aspect of mucus
anterior rhinoscopy nasal endoscopy
61
ALLERGY DIAGNOSIS
62
SKIN TEST
Skin testing methods
- Scratch test
- Poor reproducibility
- Possible systemic reaction
- Prick test
- Diagnosis of immediate type allergy
- High degree of correlation between
symptoms and provocative challenge
63
SKIN TEST
Skin testing methods
- Prick test
- Standarised methods (trained investigator)
- 2 cm apart
- Intradermal skintest (weak allergen solution)
- Less sensitive
- False positive reactions
- Correlate less well with symptoms
- Less safe (?-blocker)
64
Allergy skin prick testing
- Skin prick test / positive result
65
FACTORS AFFECTING SKIN TESTING
- Quality of allergen extract
- Age
- Drugs
66
CLINICAL VALUE OF SKIN TESTS
A positive skin test alone does not confirm a
definite clinical reactivity to an allergen !
67
IgE
Serum total IgE
Serum specific IgE
- lt allergic / parasitic diseases other
conditions - barely predictive for allergy screening in
rhinitis
High predictability in diagnosis of immediate
type allergy
68
NASAL CHALLENGE
- Research
- Less in clinical practice
- important in diagnosis of occupational
allergic rhinitis
69
NASAL CHALLENGE
NASAL CHALLENGE WITH ALLERGEN
- Indications
- Allergen provocations
- Discrepancy between history of AR and tests or
between tests - Diagnosis of occupational AR
- Before immunotherapy
- As research tool
70
NASAL CHALLENGE
- Lysin-aspirin nasal provocation substitute
for oral provocation in aspirin-intolerance - To test non-specific hyperreactivity
- Cold air, histamine, ...
- Not for clinical practice
- Used in research
71
NASAL CHALLENGE
- Assessment of nasal response symptom score
objective measures - Counting sneezes / attacks of sneezes
- Measuring volume / weight of nasal secretions
- ? of nasal patency / airflow / airflow
resistence
72
OTHER ENT DIAGNOSTIC TOOLS
- Imaging
- Sinus radiographs not for AR
- CT scan after specialist advice
- To eliminate other conditions
- To exclude chronic sinusitis
- To eliminate complications of sinusitis
- In pt who do not respond to treatment
- In pt with unilateral sinusitis
- MRI rarely (fungal sinusitis)
73
CONCLUSION
- The diagnosis of allergic rhinitis is based on
several milestones - Symptoms of AR
- Medical history
- Examination of the nose
- SPT
- IgE
- Nasal challenge
74
Treatment of allergic disease First generation
oral antihistamines
- Chlorpheniramine, diphenydramine, promethazine,
tripolidine - Use limited by sedative and anticholinergic
effects
75
Treatment of allergic disease properties
required of ideal second/third generation
antihistamines
- Pharmacological
- potent, non-competitive H1-receptor blockade
- additive anti-allergic activities
- no interference of activity by foods
- known therapeutic dose
- Pharmacokinetics
- rapid onset and 24 hour duration of action
- once daily administration
- no tachyphylaxis
76
Treatment of allergic disease properties
required of ideal second/third generation
antihistamines
- Lack of unwanted effects
- no sedation
- no anticholinergic effect
- no weight gain
- no cardiac toxicity
77
Treatment of allergic disease Second generation
oral antihistamines
Acrivastine, (astemizole), azelastine,
(levo)cetirizine, ebastine, epinastin,
fexofenadine, ketotifen, levocetirizine,
(des)loratadine, (terfenadine), mizolastine
- Greatly reduced unwanted effects
- First line treatment for intermittent or mild
persistent AR
Withdrawn from some markets because of rare
cardiotoxic effects when taken in association
with azolic antifungal agents and macrolide
antibiotics
78
Treatment of allergic rhinitis Topical
antihistamines
Azelastine and levocabastine
- Rapid onset of action (15 minutes)
- Twice daily administration
- Recommended for organ-limited disease
- May be used on-demand in addition to a
continuous medication - Good safety profile
79
Treatment of allergic disease Topical
corticosteroids
- Beclomethasone dipropionate
- Budesonide
- Flunisolide
- Fluocortinbutyl
- Fluticasone propionate
- Mometasone furoate
- Triamcinolone acetonide
80
Treatment of allergic rhinitisTopical
corticosteroids - 1
- Potent anti-inflammatory agents
- Effective in treatment of all nasal symptoms
including blockage - Once or twice daily administration
- Superior to antihistamines for all nasal symptoms
- First line pharmacotherapy for moderate-severe
persistent allergic rhinitis
81
Treatment of allergic rhinitis Topical
corticosteroids - 2
Safety
- Occasional unwanted effects
- Rarely affect HPA axis (some exceptions)
- Anecdotally, perforation of the nasal septum has
been reported - One study reports decrease in growth in children
taking Beclomethasone dipropionate
82
Treatment of allergic rhinitis Systemic
corticosteroids
- Short courses of oral corticosteroids (lt 3 weeks)
can be prescribed for severe refractory symptoms - Can be repeated every 3 months
- May be used with caution in children and in
pregnancy, if no alternative available - Intramuscular injection of corticosteroid
suspensions should be avoided
83
Specific immunotherapy (SIT)
- Interference with basic pathophysiological
mechanisms of allergic disease - Effective treatment for seasonal and perennial
allergic rhinoconjunctivitis and asthma - Prevention of the development of new
sensitisations and asthma in patients with
allergic rhinitis
WHO position paper, 1998
L. De Schryver
84
Mechanisms of immunotherapy
IFN-?
IgG
Th1
IL-4
IgE
Allergen
APC
IL-5
Eosinophils
Immune deviation Anergy of TH2/TH0 cells ?
Increase in Th0/Th1
cells ?
Durham and Till, JACI 1998
L. De Schryver
85
Mechanisms of immunotherapy
- Decrease in inflammatory mediators during both
early- and late-phase responses - Reduction of mast cell numbers with a consequent
reduction in immediate allergic sensitivity - Decrease in eosinophil counts and eosinophil
cationic protein concentrations in
bronchoalveolar lavage fluid
Durham and Till, JACI 1998
L. De Schryver
86
- Statement of evidence Category of evidence
- Shekelle et al, BMJ 1999
- Ia evidence for meta-analysis of randomised
controlled trials - Ib evidence from at least one randomised
controlled trial - IIa evidence from at least one controlled study
without randomisation - IIb evidence from at least one other type of
quasi-experimental study - III evidence from non-experimental descriptive
studies, such as comparative studies,
correlation studies and case-control studies - IV evidence from expert committee reports or
opinions or clinical experience of respected
authorities, or both
87
- Statement of evidence Strength of evidence
- Shekelle et al, BMJ 1999
- directly based on category I evidence
- directly based on category II evidence or
extrapolated recommendation from category I
evidence - directly based on category III evidence or
extrapolated recommendation from category I or
II evidence - directly based on category IV evidence
88
- Strength of evidence for treatment of rhinitis
ARIA - Intervention SAR PAR
adult children adult ch
ildren - oral anti-H1 A A A
A - intranasal anti-H1 A A A
A - intranasal CS A A A A
- cromones A A A A
- anti-leucotriens A
- subcutaneous SIT A A A A
- sublingual/nasal SIT A A A
- allergen avoidance D D D D
89
Medications of allergic rhinitis - ARIA
- sneezing rhinorrhea nasal
nasal eye - obstruction itch
symptoms - H1-antihistamines
- oral 0 to
- intranasal
0 - intraocular 0 0 0 0
- Corticosteroids
- Cromones
- intranasal
0 - intraocular 0 0 0 0
- Decongestants
- intranasal 0 0 0
0 - oral 0 0 0
0 - Anti-cholinergics 0 0
0 0 - Anti-leukotriens 0
0
90
(No Transcript)
91
Stepwise approach
92
Seasonal allergic rhinitis
Need for therapy ?
Mild disease or occasional symptoms
Moderate disease or long duration
Severe disease
Nasal Corticosteroids Oral or
Nasal Antihistamines
Nasal Corticosteroids
Oral or Nasal Antihistamines (Cromones)
Inadeq. control
Inadeq. control
Inadeq. control
For eye symptoms topical antihistamines or
cromones
Add further symptomatic treatment Short-course
Oral Steroids Consider Immunotherapy
93
Perennial allergic rhinitis in adults
Avoidance
Need for therapy ?
Environment control
Mild disease or occasional symptoms
Moderate disease or long duration
Severe symptoms
Nasal Corticosteroids Antihistamines
Inadeq. control
Inadeq. control
Oral or Nasal Antihistamines
Nasal Corticosteroids
Inadeq. control
Further examinations
94
Perennial allergic rhinitis in adults
RESISTANT CASES
Nasal blockage
Resistant rhinorrhea
Short Course of Topical Decongestants/ Oral
Decongestants/ Oral Steroids
Nasal Ipratropium bromide
Immunotherapy
If resistant
Surgical turbinate reduction
95
Perennial alllergic rhinitis in young children
Avoidance
Need for therapy ?
Environmental control
Oral or Nasal Antihistamines (Cromones)
Nasal Corticosteroids in adequate dose
Add Antihistamines
Consider Immunotherapy
96
Rhinitis guidelines validation study
Jean Bousquet Paul van Cauwenberge Valerie J. Lund
Multicentre, multinational, open label,
randomised, parallel group Comparing two
therapeutic strategies (recommended and free
choice) in seasonal allergic rhinitis (SAR)
patients
- Study period May 1998 September 1998
- 600 adult outpatients in 328 GP centres in
Belgium, France and UK - Three weeks duration
97
Study plan
Investigators randomised to
A
B
Treat patients according Treat patients
according to guidelines to usual practice
225 patients with SAR 244 patients with
SAR screened and enrolled screened and enrolled
- Patients treated for 3 weeks
- Recorded
- Reflective symptoms twice daily
- Medicine utilisation daily
- RQLQ and SF-36 at day 7 and day 20
- Global evaluation at day 21
98
Allocation of treatments according to baseline
symptoms
- Conjunctivitis Rhinitis symptoms
- symptoms Mild rhinitis Mod/severe rhinitis
- None/mild Oral anti-H1 Oral anti-H1 and
- conjunctivitis topical nasal steroid
- Mod/severe Oral anti-H1 Oral anti-H1 and
- conjunctivitis and topical topical nasal
steroid - ocular and topical
- cromone ocular cromone
Oral anti-H1 ebastine Topical nasal steroid
triamcinolone acetonide Topical ocular cromone
nedocromil
99
Strategy A Strategy B Diff. between
LS LS mean SE LS mean SE Mean group
A/B (n 207) (n 224) (SE of
diff.)Stuffiness 1.48 (0.09) 2.02 (0.08)
-0.54 (0.12)Rhinorrhea 1.03 (0.07)
1.63 (0.07) -0.61 (0.10)Sneezing 0.73
(0.07) 1.32 (0.06) -0.60
(0.09)Itching 0.67 (0.07) 1.05 (0.06)
-0.39 (0.09)Eye symptoms 1.02 (0.08)
1.45 (0.07) -0.42 (0.10)Total
score 4.93 (0.28) 7.48 (0.28) -2.55
(0.38)
Mean symptom score over the treatment period
p lt 0.001
100
Total symptom scores (SE) over 21 days
Group A Treatment according to guidelines
Group B Treatment according to free choice
Least square means (SE)
10
7.48 (0.276)
8
4.93 (0.282)
6
4
2
0
Strategy A
Strategy B
101
Individual symptom scores over 24 hours days
17
Group A Treatment according to guidelines
Group B Treatment according to free choice
Least square means
2.5
1.5
0.5
Rhinorrhoea
Stuffiness
Sneezing
Itching
Eye
symptoms
plt0.001 Group A vs Group B
102
Strategy A Strategy B Diff. between LS LS
mean LS mean SE Mean group A/B SE (n
189) (SE of diff.)Activities 0.73
(0.09) 1.27 (0.09) -0.54 (0.12)Sleep 0.53
(0.10) 1.14 (0.10) -0.61 (0.13)Non hay fever
S/ 0.71 (0.08) 1.07 (0.07) -0.36
(0.10)Practical Problems 0.78 (0.11) 1.55
(0.10) -0.78 (0.14)Nasal symptoms 0.82
(0.10) 1.45 (0.09) -0.63 (0.13)Eye
symptoms 0.61 (0.09) 1.04 (0.09) -0.43
(0.12)Emotion 0.64 (0.08) 1.02 (0.07) -0.38
(0.07)Total score 0.69 (0.07) 1.19
(0.07) -0.50 (0.10)
RQLQ Mean change from baseline
p lt 0.001
103
RQLQ (disease specific QOL scale) day 21
Group A Treatment according to guidelines
Group B Treatment according to free choice
Least square means
1.6
1.2
0.8
0.4
0
Total
Sleep
Activities
Emotions
Eye symptoms
Nasal symptoms
Practical problems
Non-hay fever symp.
plt0.001 Group A vs Group B
104
Patient and investigator opinion
- Opinion Patient Investigator
- A B A B
- Greatly improved 55 38 69 54
- Somewhat improved 18 30 20 33
- No change 7 9 6 7
- Somewhat worsened 0.5 0.5 1.5 1
- Greatly worsened 0.5 0.5
0.5 0 - Not recorded 19 23 7 11
Statistically significant differences between
groups A B For patients opinion
(p0.016) For investigators opinion (p0.026)
105
Study medication usage moderate/severe rhinitis
and moderate/severe conjunctivitis
No of patients ()
Strategy A (n134)
80
Strategy B (n150)
SA - systemic antihistamine TE - topical eye
cromone NC - nasal corticosteroid
60
40
20
0
SA
SA TE
SA NC
NC
Other combinations
SA NC TE
106
Results from guidelines study
- Treating seasonal allergic rhinitis based on the
International Rhinitis Guidelines has proved
beneficial in terms of both symptom scores and
QOL compared with a non-guided therapeutic
strategy - When a non-guided strategy is used, often the
medication chosen is inappropriate or not
sufficiently efficacious
107
- Recommendations
- 1- Patients with persistent rhinitis should be
evaluated for asthma - 2- Patients with persistent asthma should be
evaluated for rhinitis - 3- A strategy should combine the treatment of
upper and lower airways in terms of efficacy and
safety