Urinary System - PowerPoint PPT Presentation
1 / 52
Title:
Urinary System
Description:
Chapter 26 Urinary System ... (Fig. 26.17of Seeley) ... The descending portion of the loop of Henle reabsorbs additional 20% of water by osmoais and small amounts of ... – PowerPoint PPT presentation
Number of Views:337
Avg rating:3.0/5.0
Title: Urinary System
1
Chapter 26
- Urinary System
2
Urinary System Functions
- Filtering of blood
- Regulation of
- blood volume
- concentration of blood solutes
- pH of extracellular fluid
- blood cell synthesis
- Synthesis of Vitamin D
- Increased PTH promotes Vitamin D
formation in the kidneys
3
1. Overview The urinary system is the system
responsible for removing organic wastes from the
body in a liquid form. By doing so in an
appropriate manner, the urinary system
contributes to the homeostasis of the body.
They regulateBlood volume, blood pressure,
plasma electrolytes, pH, blood glucose and, blood
amino acids, etc. It is also important to note
how the urinary system is isolated from the
circulatory system to avoid contamination.
4
The manner how the urinary system works is
unique. It first filters out water, electrolytes
and small organic molecules into the capsular
space, then one by one reabsorb those which are
needed back from the tubules and ducts. If the
urinary system fails to properly filter and
reabsorb these vital ions and molecules, they may
be wasted into the urine. Thus, by observing
what you find in the urine you may be able to
judge the health of a subject. An adult produces
about 1.4 L of urine per day. Note each adult
consume about 2L of liquid each day. Where did
the rest go?
5
Urine Formation
6
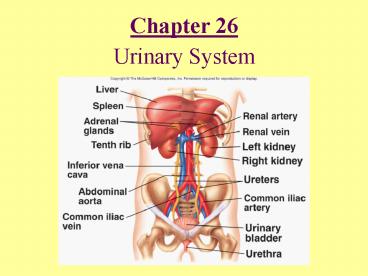
Urinary System Anatomy
7
Internal Anatomy of Kidneys
- Cortex Outer area
- Renal columns
- Medulla Inner area
- Renal pyramids
- Calyces
- Major Converge to form pelvis
- Minor Papillae extend
- Nephron Functional unit of kidney
- Juxtamedullary
- Cortical
8
The Nephron
9
(No Transcript)
10
i. Overall Functions of the nephron The basic
functional units of the kidney are shown in Fig.
26-6. The formation of urine starts with the
filtrates from arterial blood, which will be
released into the renal corpuscle. In the renal
corpuscle, blood pressure in the renal arterioles
pushes water, electrolytes and small organic
molecules into the capsular space ( Bowmans
space) across the glomerular walls. Small
important substance, which have passed through
the pores of the membrane must be reclaimed,
while keeping the wastes in the collecting duct..
11
i. The blood supply to the kidneys 1200 ml/min
through the kidneys Consumes 20 - 25 of the
cardiac output! Study Fig. 26-7b,2 and Fig. 26.6
of Seeley, and follow the direction of blood
vessels. Note the afferent and efferent
arterioles. Where are the peritubular
capillaries What are vasa recta?
12
(No Transcript)
13
a. The basic principles of urine production The
reason for urine production is to maintain the
homeostasis of the blood. The urine collects
metabolic waste products.
14
i. There are three major waste products in
urine Table 26-2 (a) Urea form the breakdown
of amino acids. 21 g/day. (b) Creatinine from
the breakdown of creatine phosphate, recall
muscle contraction. 1.8 g/day. (c ) Uric acid
from RNA. 0.48 g/day. These wastes filter
through glomerular membranes with a large
quantity of water and ions. In other words, the
concentrations of these ions and molecules in the
in the filtrate and plasma are the same.
15
i. The majority of water must be reclaimed to
avoid dehydration. Water is first filtered
through the pores of glomerular membrane by the
blood pressure into the Bowmans
space. Resorption for reclaiming water,
electrolytes, small organic molecules either by
simple diffusion or with the carrier proteins at
the proximal tubule starts immediately. Fig.
26.8 of Seeley Resorption of water continues at
the descending limb of the loop of Henle. Fig.
26-13b
16
Urine Formation
17
Fig. 26-13b Water uptake at descending loop of
Henle
18
Fig. 26-8 The renal corpuscle
19
Fig. 26-10 Glomerular filtration
20
Filtration Pressure
21
- Filtration at the glomerulus
- (a) The glomerular filtration pressure (Fig.
26-8, 10, Fig. 26.9) - The driving force at the glomerular is the
difference between the blood pressure and osmotic
pressure. - The net filtration pressure is about 7 mmHg and
is very small. - Thus, slight change in blood pressure could
change the magnitude of this driving force and
can impair the function of the kidneys. - Note that the muscles of arterioles can easily
change the diameters, thus the regional blood
pressure.
22
(a) The glomerular filtration rate (GFR) The
filtration surface area of each kidney is 6 sq
m. GFR is 125 ml/min for each kidney or 250
ml/min for the both kidneys. Since a 1,200
ml/min of blood is supplied to the kidneys, and
about a half of it are fluid, more than 40 of
fluid in the blood are filtered. 360 liters (100
gallons) are filtered through per day. But 99
of the filtrates are reabsorbed. The GFR may be
regulated with hormone.
23
(a) The proximal (convoluted) tubule
(PCT) Transports across the nephron cells in
this region starts with two basic driving forces
(Fig. 26-12) 1. Osmosis Having higher
concentration of water in the filtrate than in
the interstitial fluid. 2. Active Na/K
exchange pump at the site of basal membrane to
force Na out of the cell to the interstitial
fluid. Thus, water will go back to the nephron
blood vessels, peritublar capillary, by
osmosis. Na gets out from the nephron cells to
the interstitial fluid by the Na/K exchange
pump.
24
Fig. 26-12 Transport at the PCT
25
Most of the ions, glucose and amino acids from
the filtrate will enter the nephron cells in the
form of Na cotransport, since the intracellular
Na concentration is constantly being lowered by
Na/K exchange pump. At the site of the basal
membrane, they will diffuse out, sometimes
facilitated, according to the concentration
gradients. Reclaims 60 - 70 of water and most
of the glucose (diabetes mellitus?), amino acids
and other organic substances. Urea, uric acid
and creatinine are not absorbed, thus increasing
their concentrations in the tubule.
26
(a) The loop of Henle (Fig. 26-13) The
descending portion of the loop of Henle reabsorbs
additional 20 of water by osmoais and small
amounts of ions may be returned to the
filtrate. On the contrary, the ascending portion
of the loop of Henle, which is impermeable to
water, reabsorbs 25 of sodium and chloride ions.
by the Na/K exchange pump locate in the basal
membrane - similar to the proximal tubule. In
fact, the sodium and chloride ions absorbed back
into the interstitial fluid contribute to extract
more water from the descending portion of the
loop. NOTE Pumping of ions across a cell
27
Fig. 26-13 The loop of Henle
28
Fig. 26-13b,c
29
We have already seen that cell membrane may have
a sodium pump which is energized with ATP. If
the cell membrane is uniform over the entire
cell, sodium may simply pumped out from the cell,
but the sodium ion cannot run across the
cell. To transport Na across a cell, requires a
cell with asymmetirc membrane. Proximal tubules
and ascending loop of Henle are surrounded with
such cells. In the membrane towards the
interstitial space, sodium ion is actively
transported out from the cell into the
interstitial space. While on the tubular side of
the membrane, in which no active sodium pump is
found, sodium ion, along with the others,
passively enters into the cell. The over all
movement of sodium ion is to actively transport
from the tubular to interstitial fluid across the
cell.
30
The results of active pumping of the salts in the
ascending loop of Henle are in two fold(1)
The salt concentrations in the upper end of the
tubule go down.(2) The salt concentrations in
the upper region of medulla will go up due to the
released salts. The consequence of increased
salt concentrations in medullar will result in
more effective osmotic release of water from the
tubule. By the time the urine leaves the loop
of Henle, it has much lower concentrations of Na
and Cl-. By this time 80 of water and 85 of
the solutes have been reabsorbed. The waste
products are not reabsorbed.
31
(a) The distal convoluted tubule (DCT) and the
collecting system The DCT and collecting duct
are impermeable to solutes. Requires active
reabsorption or secretion for transport. Active
reabsorption of Na is exchanged for K or H in
response to aldosterone. Fig. 26-14, 15
32
Fig. 26-14 The DCT
33
Fig. 26-14c The DCT
34
The water reabsorption is controlled by
antiduretic hormone (ADH). (Fig. 26.17of Seeley)
ADH activate ADH receptor and in turn activates
G-proteins for cAMP production, which opens up
the water channel in the membrane, thus removes
water out of the urine. At the end of the
distal collecting duct, the solution osmolarity
could increase from 100 mOSM at the entrance to
1200 mOSM
35
Effect of ADH on Nephron
36
a. The control of kidney function By adjusting
the diameters of the afferent and efferent
arterioles. Activities of the sympathetic
division of the ANS. Via hormonal control.
37
i. The local regulation of kidney function By
automatic changes in the diameters of the
arterioles and the glomerular capillaries -
change in the blood pressure. ii. Sympathetic
activation and kidney function By adjusting the
flow of blood to the kidneys. Sympathetic
activation results in constricting the afferent
arterioles - reduced blood flow to the glomerular
capillaries. Sympathetic activation of the
vasomotor center changes the regional pattern of
blood circulation - reduced GFR.
38
ADH The function of ADH has been discussed
earlier. (Fig. 26.17 of Seeley) Insufficient
release of ADH may result in diabetes insipidus,
large quantity of clear urine accompanied with
dehydration and abnormal electrolyte balance.
In contrast, diabetes mellitus may result in
large quantity of urine with high concentration
of glucose.
39
Renin -Angiotensin II- Aldosterone system for
Na, Cl- and K balance. (Fig. 26.18 of
Seeley) Decrease in the concentration of Na in
the interstitial fluids increase the rate of
aldosterone secretion initiating the release of
Na from the distal tubule.
40
Aldosterone Effect on Distal Tubule
41
Fig. 26-16 Summary
42
Fig. 26-16b summary
43
Table 26-6 Urine composition(Review)
44
Fig. 26-19c Urinary Bladder
45
Micturition Reflex
46
1. Urine transport, storage and
elimination c. The micturition reflex and
urination The process of urination is
coordinated by the micturition reflex. Fig.
26.20 Note the stretch receptor - sensory fiber
- parasympathetic motor neurons etc. 200 ml of
urine in the bladder sends the urge starting from
the stretch receptors. Contraction and
relaxation of the internal and external
sphincters decide the release of urine.
47
CHAPT 27 Water, Electrolytes and acid base
balance Extensive discussion on fluid,
electrolytes and acid-base balance are presented
in this chapter. We will focus only on acid base
balance based on carbonic acid.
48
1. Acid and base Most commonl definition of acid
is its ability to produce H. There are strong
and weak acids. Strong acids dissociate
completely to ions and produce H and the counter
ions. Examples are HCl -- H Cl- H2SO4
- 2H SO4 On the other hand, weak acids
dissociate partially and establish equilibrium.
Examples are acetic acid and carbonic acid.
49
(No Transcript)
50
2. Buffers and acid base balance Buffers are
substances which resist the change of pH a
solution and a weak acid is a good candidate. In
human body, proteins and carbonic acid take the
major role as buffers. The buffering action of
proteins depend ionization of groups, which may
be ionized at physiological range of pH, 7.2 -
7.4. Such compounds are the alpha amino group
and histidine of proteins. R-NH3 R-NH2
H
51
Carbonic acid may be formed when carbon dioxide
is released in solution slowly or quickly with
the aid of an enzyme, carbonic anhydrase and
reacts with water. It further dissociates to
ionic forms, proton and bicarbonate. CO2 H20
H2CO3 H HCO3- As we have seen the
production of bicarbonate during respiration,
release of protons into the tubular lumen also
involves the above reaction. Knowing that the
membrane at the side of tubular lumen is
impermeable to bicarbonate , but permeable to
carbon dioxide, the transport of proton is
possible to tubular lumen. The acid forming
proton is now neutralized by reaction with
bicarbonate.
52
(No Transcript)