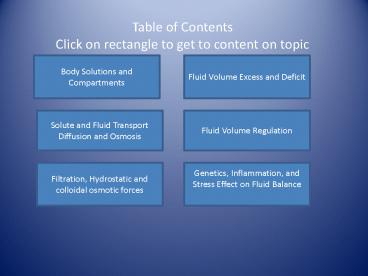
Table of Contents Click on rectangle to get to content on topic PowerPoint PPT Presentation
1 / 50
Title: Table of Contents Click on rectangle to get to content on topic
1
Table of ContentsClick on rectangle to get to
content on topic
Body Solutions and Compartments
Fluid Volume Excess and Deficit
Solute and Fluid Transport Diffusion and Osmosis
Fluid Volume Regulation
Genetics, Inflammation, and Stress Effect on
Fluid Balance
Filtration, Hydrostatic and colloidal osmotic
forces
2
Objectives
- Identify body fluid composition and compartments
- Review basic pathophysiology around water and
solute movement - Identify altered fluid balance states
- Discover age, genetic, stress, and inflammation
factors that have an effect on fluid balance - Recognize outcomes and interventions for fluid
volume excess and fluid volume deficit
3
The Ins and Outs of Fluid Balance
- Mary Farrington
- MSN Student-MSN 621
- April 2010
4
Question
- Edema is present when one of the following
compartments is expanded by 2.5 to 3 liters. - In which body fluid compartment does edema
reside?
Intravascular
Interstitial
Trancellular
Drag on cylinder to see if you are right
5
The Goal of Human Fluid Balance
- To reach euvolemia where loss and intake of
fluids is balanced - Pathology that can alter fluid balance
Surgical disturbances Organ failure
Inflammation Renal dysfunction
Loss of extracellular fluid Liver failure
Evaporation and loss of fluid Heart failure
Hemorrhage Pancreas
Restricted fluid before surgery Skin
6
Compartments Where Fluid Resides
- Extracellular fluid compartment (ECF)surrounds
the cell - Intracellular fluid compartment (ICF) contained
within cell
Think about these electrolytes importance in your
patient assessment
ICF Major Ion Potassium
ECF
Cell
ECF Major Ion Sodium Chloride
Cell membrane
ICF
7
Body Fluid Composition and Compartments
Body fluid composition is water and dissolved
substances consisting of solutes and electrolytes
The 60-40-20 Rule 60 of body weight is
water 40 of body weight is intracellular
fluids 20 of body weight is extracellular fluid
Intracellular
Cell
Extracellular
8
Extracellular Fluids
9
Body Fluid CompartmentsClick on Box to see if
your are right.
- What are the major compartments for body fluids?
Extracellular
Intravascular
Transcellular
Intracellular
10
Cell Membrane
- Primary barrier to movement of substances between
ECF and ICF
Extracellular compartment Volume (ECF)
Cell membrane
Cell
Intracellular compartment Volume (ICF)
11
Cell Membrane Transport
- Molecules and Ions depend on transport mechanisms
to go from ECF to ICF
Extracellular compartment Volume (ECF)
Cell membrane
Cell
Intracellular compartment Volume (ICF)
Pot
12
Solute Movement
- Solutes move by
- Diffusion
- Mediated passive transport (No energy required)
- Mediated active transport (Energy required)
Cell
Cell membrane
Extracellular compartment Volume (ECF)
Intracellular compartment Volume (ICF)
13
Passive Transport Diffusion
- Molecules move along concentration gradient
across cell membrane until there is a balanced
concentration and gradient is gone. Example
diffusion of oxygen in alveoli allowing
replenishment
(ECF)
Permeable cell membrane
(ICF)
M
M
Cell
M
Equal concentration
Cell
Low concentration
Permeable cell membrane
(ICF)
(ECF)
Equal concentration
High concentration
14
Mediated Passive Transport (Facilitated Diffusion)
- Large molecules moves along concentration
gradient and are assisted by the carrier protein
to cross cell membrane. Example glucose
High concentration
Semi permeable Cell membrane
Cell
(ECF)
(ICF)
Carrier protein
glucose
Low concentration
15
Active Transport
- Requires energy (ATP) to move molecule with
carrier protein - Involves action against the cells electrical or
chemical gradient - Molecules need to move uphill thus require
energy
M
ATP
CP
Cell
Semipermeable Cell membrane
(ECF)
High concentration gradient on membrane
(ICF)
Porth p.75
16
Active Transport Sodium Potassium Pump
- Maintains the differences between intracellular
extracellular Na K. (Very active in the heart)
ATP
(ECF)
CP
k
Cardiac Cell
k
Na
Na
(ICF)
Na
17
Quiz Is it A, B, or CClick on Shape to See if
You Are Right
Protein Carrier
A concentration difference between high level of
concentration and low level of concentration
B
Diffusion
B necessary for active transport and facilitated
diffusion
C
Concentration Gradients
C particles or molecules move area of high
concentration to low concentration until BALANCED
A
18
Water Movement
- Osmotic forces
- Osmosis
- Osmotic Pressure
- Oncotic Pressure
- Isotonic
- Hypotonic
- Hypertonic
- Filtration Hydrostatic pressure
Cell membrane
Intracellular compartment Volume (ICF)
Cell
Extracellular compartment Volume (ECF)
19
Osmosis-Passive
- Movement of water across semipermeable membrane
from an area of lower solute concentration to
higher solute concentration
Notice Osmosis is movement of water to lower
volume of water and greater number of
solutes. Diffusion is movement of solutes to
higher volume of water and lower number of solutes
Extracellular compartment Volume (ECF)
water
Intracellular compartment Volume (ICF)
Cell
Cell membrane
Greater number of particles-Less water
Fewer particles-More water
20
Osmosis Pressure
- Hydrostatic pressure (HP) required to stop
osmotic flow of water
water
HP
Extracellular compartment Volume (ECF)
water
water
Cell
Intracellular compartment Volume (ICF)
Greater number of particles-Less water
Semipermeable Cell membrane
Fewer particles-More water
21
Osmolarity
- Measure of solutions ability to create osmotic
pressure of force and affect water movement
Serum Osmolality
Number of solutes per KG of water IN the
body Serum Isotonic concentration275-295
mOsm/Kg Serum Hypotonic concentrationlt275
mOsm/Kg Serum Hypertonic concentrationgt295
mOsm/Kg
22
Osmolality of Solutions
- Isotonic-same osmolality as body
- fluids
- Hypotonic-osmolality less then body
- fluids
- Hypertonic-osmolality greater than
- body fluids
0.9 NACL
0.45 NACL
D5LR
Do you know a example of IV solution for each
osmolality. Click on word osmolality to see if
you are right.
23
Capillary
- Capillary Membrane separates Intravascular
Space(IVS) from Interstitial Space - Capillary Interstitial Fluid Exchange is transfer
of water between vascular and interstitial
compartments
Capillary
Capillary Membrane
24
FiltrationMovement of water and solutes from
area of higher hydrostatic pressure to an area of
low hydrostatic pressure. Pushes fluid out of
arterial end of capillary to interstitial space.
30mmHg
10mmHg
IF pressure -3 mm Hg
25
Hydrostatic PressurePressure created by weight
of fluid and is impacted by distance from heart
pump and amount of fluid. Moves fluid out of
capillary bed
30mmHg
10mmHg
Interstitial Fluid pressure -3 mm Hg
26
Colloidal Osmotic PressureResponsible for moving
fluid back to capillary with colloids. Assists in
retaining fluids in plasma
Click here to return to FVE
28mmHg
28mmHg
IF pressure 8 mm HG
27
Lymph SystemExcessive interstitial fluid that
can be returned to circulatory system
Excessive fluid and proteins not absorbed in
capillary
28
Quiz Is it A, B, or CClick on Rectangle to See
if You Are Right
Filtration A
Pressure created by weight of fluid. Impacted by
distance from heart and amount of fluid.
B
Hydrostatic Pressure B
Excessive fluid and proteins not absorbed in
capillary
C
Movement of water and solutes from an area of
high hydrostatic pressure to an area of low
hydrostatic pressure
Lymphatic Drainage C
A
http//quizlet.com/1916557/ fluid-balance-flash-ca
rds
29
Fluid Volume Excess(FVC)-Increase In ECF
Compartment Volume
- Why it happens-Movement of water exceeds the
Compartment space - Excessive fluid intake
- Over-hydration
- Excessive sodium intake
- Water retention caused by disease states
- Renal dysfunction
- Liver dysfunction
- Congestive heart failure (Remember hydrostatic
and colloid forces) - Increased corticosteroid level
Click here
Porth p 778-779
30
Fluid Volume Excess Assessment and Management
Porth p 778-779
31
FVE Outcomes/Interventions
Patient demonstrates adequate fluid volume status Normotensive blood pressure (BP) Below 120/80 Heart rate (HR) 100 beats/min Respiratory rate 20 or below Clear lung sounds Pulmonary congestion absent on x-ray Consistency of weight( absence of upward trend from baseline) Resolution of edema or decrease in edema Instruct patient to follow fluid and restriction intake as prescribed by physician team. This helps decrease extracellular fluid volume In case of organ dysfunction etiologies of FVE instruct patient to take daily weight for detecting fluid volume increase Monitor intake and output Instruct to elevate edematous extremities to promote venous return of fluid decreasing edema Instruct on medications and dietary recommendations for sodium and potassium Hospitalized patient considerations concentrate IV fluids and prepare for possible ultra filtration or hemofiltration Assess degree of edema and cardio respiratory status Communicate patient changes to physician
Outcomes Interventions
http//www1.us.elsevierhealth.com/MERLIN/Gulanick/
Constructor/
32
Fluid Volume Deficit-Decrease In ECF Compartment
Volume
- Why it happens? Remember Solute and Fluid
Transport - Dehydration
- Decreased fluid intake
- NPO
- Swallowing problems
- Malaise malnutrition
- GI loss
- Nausea vomiting
- Diarrhea
- GI suction
- Fluid loss via integumentary system
- Fever
- Severe wounds form burns
- Renal loss
- Effect of drugs
- Kidney disease
- Endocrine imbalance
- Third space fluid loss
Porth p 778-779
33
Fluid Volume Deficit(FVD) Assessment and
Management
Porth p 778-779
34
FVD Outcomes/Interventions
Patient demonstrates adequate fluid volume status Urine output greater than 30 ml/hr Normotensive blood pressure (BP) Below 120/80 Heart rate (HR) 100 beats/min Respiratory rate 20 or below Consistency of weight( absence of lower trend from baseline) Normal skin turgor. Encourage patient to drink prescribed fluid amounts. Assess for patients preference and keep in reach Remind to drink and assist to drink as needed for cognitive and mobility dysfunction Deliver parenteral fluid replacement as ordered if volume deficit severe If deficit causes hemodynamic instability anticipate need for large bore intravenous catheter for rapid infusion of crystalloid and possible colloids if loss of intravascular fluids Assess for sighs and symptoms of fluid overload. If present, stop fluid and support body position for optimization of thoracic cavity to promote breathing Monitor I/O and daily weights Communicate patient changes to physician team
Outcomes Interventions
http//www1.us.elsevierhealth.com/MERLIN/Gulanick/
Constructor/
35
Regulation of Body Fluid Volume
- Major organ in water sodium balance is kidney
- Kidneys conserve water by concentrating urine
relative to plasma - Kidneys rid body of excessive water by dilute
urine relative to plasma - Control of water excretion in kidney is regulated
by anti-diuretic hormone (ADH) The hormone is
secreted by hypothalamus. - ADH aids in water absorption at kidney collecting
ducts - Hypothalamus and atria of heart have stretch
receptors sensitive to plasma osmolality
http berkley.edu course kidney fluid2010
Microsoft clip art
36
Regulation of Fluid Volume Excess
Increased vascular volume or increased blood
pressure leading to increased atrial stretch
Increased release of atrial natriuretic factor
Direct vasodilatation
Increased excretion of NA H2O by the kidney
secondary to increased filtration
Decreased renin/angiotensin/aldosterone
Decreased release of ADH
Decreased vascular volume and or blood pressure
Heitz 18. microsoft clip art
37
Regulation of Fluid Volume Deficit
Loss of hypotonic fluid
Increased plasma osmolality
Decreased plasma volume
Increased thirst
Decreased cardiac output
Increased ADH Secretion
Decreased blood pressure
Decreased renal perfusion
Increased reabsorption of filtered water by the
kidney
Decreased water and sodium filtered by the kidney
Increased renin release
Increased angiotensin I/II
Increased aldosterone secretion by adrenal cortex
Decreased water excretion
Decreased sodium and water excretion
Increased water intake
Increased volume of sodium and water
Increased plasma volume and decreased osmolality
Heitz 16. microsoft clip art
38
Regulation of Fluid Volume Deficit-Hemorrhage
Hemorrhage
Decreased arterial pressure(decreased renal
perfusion)
Release of renin by the kidneys
Renin substrate
Angiotensin I converting enzyme ( lung)
Angiotensin II
Release of aldosterone
Vasoconstriction
Retention of sodium and water
Increased vascular volume
Increased arterial pressure
Heitz 15. microsoft clip art
39
Quiz Name Regulatory Hormones for Water and
Sodium Balance by Function Defined
Receptors in hypothalamus note increasing plasma
osmolality resulting in stimulation of which
hormone? It causes water to be reabsorbed by
renal tubes.
- Regulates sodium balance thus water . Increases
Plasma volume. Increased BP, Decreased urine
ADH-Anti-Diuretic hormone
Aldosterone
Click on box for hormone name
http//quizlet.com/1916557/fluid-balance-flash-car
ds
40
Age Effect on Fluid Balance-Deficit
- Total body water decreases due to increased
adipose tissue. Adipose tissue has less water. - Unknown mechanism for decreased thirst in elderly
- Decreased thirst decreased water intake
Rolls 137. microsoft clip art
41
Age Effect on Fluid Balance-Excess
- Aged heart has less stretch and efficiency for
pumping - This puts aged at risk for heart failure and
fluid volume excess - Elderly are more at risk for fluid
overload due to decreased kidney function
Rolls 137. microsoft clip art
42
Genetics Effect on Fluid Balance
- Plasma renin, plasma aldosterone concentrations ,
blood pressure, renal excretion of K and NA
following volume expansion and contraction with
monozygotic and dizygotic twins studied for
trends - Conclusion genetic/ heredity influence K and NA
excretion - Current research with worms shows there are
genetic receptors on hypodermis that regulate
fluid balance homeostasis
Grim 583 Huang 2595. microsoft clip art
43
Genetics Effect on Fluid Balance
- Genetic origins for fluid balance pathologies
- Chronic kidney disease(CKD) in model of urinary
fibrosis caused by urinary obstruction - Two inbred genetic marked mice tested for CKD
after reversible unilateral ureteral obstruction
- C57BL developed CKD in 3 or more days
- BALB resistant to CKD up to ten days
Puri TS (2010) Microsoft clip art
44
Surgical Perioperative Considerations on Fluid
Balance
- Pre-existing conditions such as diabetes, renal
insufficiency can exacerbate with stress of
surgery - Patient may start at negative fluid balance due
to NPO, preps that cause GI and urine loss
Heitz p.207 microsoft clip art
45
Stress Response Influence on Fluid Balance
- A Stress state causes the body to adapt to reach
homeostasis - Fluid regulatory hormones and neurotransmitters
are released to aid in adaptation of fluid
balance from stress response (Remember slides
35-38) - ADH reabsorbs water in kidney tubules due to
circulating volume decrease - Stress response of surgery can increase ADH to
cause retention of water 48-72 hours.
Porth 205 772 microsoft clip art
46
Inflammation Response Fluid Balance
- Inflammation process causes plasma and leukocytes
to move from intravascular space to injured
tissue resulting in swelling (edema), increased
temperature-redness (blood flow) and pain
47
Surgical Inflammation Response Fluid Balance
- Release of Injury to skin and tissue (surgical
incision) causing inflammation which results in
loss of ions and protein from plasma - Increase in tissue catabolism (breakdown) results
in reactive oxidation greater amount of water
from reactive oxidation process - Potential for third spacing to occur with loss of
plasma proteins and colloid to cause leaking in
transcellular space
48
Case Study I
- 76 year old female admitted to hospital for TAH,
BSO, and bilateral oopherectomy. hysterectomy
and colon resection due to suspected cancer.
Patients medical history includes weight loss,
heart failure, and decreased appetite. - What baseline assessment would be helpful in
managing the patient fluid balance in
perioperative operative care? Click below for
answer - 2. Would urine osmolality increase or decrease if
patient dehydrated? - Click for answer
- 3. What monitoring will be important for the
patient in post operative period? - Click for answer
Assess if weight loss or gain, assess for signs
of dehydration, check preop and daily
electrolytes to see if correction required,
specific gravity(1.010-1.020)
Increase
Consideration of preop fluid status, Surveillance
of cardio respiratory status, Surveillance of
urine output, goal of IO, Daily weight.
49
Case Study II
- A forty two year old woman Gravida 3 Para 2. Last
delivery resulted in gynecological and
urological damage with stress incontinence.
Patient has decided to have elective bladder neck
suspension, including colposuspension, and
closure of a fistula involving the bladder neck
and urethra plus vaginal reconstruction.
Preoperative assessment of nutrition and weight
within normal limits.
- What monitoring will be important for the patient
in the post operative period? Click for answer - 2. If urine output drops what assessment
information would you want to report to
physician? Click for answer
Surveillance if IO with consideration of preop
fluid status, Surveillance of cardio respiratory
status, Surveillance of urine output Use bladder
scan to confirm low urine output, Daily weights
Previous interventions related to IV fluids and
IV bolus and response of urine output, total
intake and output, vital signs, unexpected bloody
drainage, cardio respiratory status changes,
Trend of vital signs compared to baseline,
Excruciating pain
50
References
- Gulanick, M. (2007). Nursing Care Plans Nursing
Diagnosis Intervention, 6 ed. Retrieved from
http//www1.us.elsevierhealth.com/MERLIN/Gulanick/
Constructor/ - Heitz, U.E., Horne M.M.(2001). Pocket guide to
fluid, electrolyte and acid-base balance . - St.Louis Mosby.
- Huang P., Stern MJ. (2004). FGF signaling
function in the hypodermis to regulate fluid
balance in C. elegans. Abstract. NIH grant
support , Yale University School of Medicine.
Retrieved from http//www.ncbi.nlm.nih.gov/pubmed
- Patlak, J. (1999), Fluid compartments in the
body. Department of Physiology, - University of Vermont. Retrieved from
http//physioweb.med.uvm.edu/bodyfluids / March
21, 2010 - Porth, C.M., (2005). Pathophysiology, 7th
edition. Philadelphia Lippincott. - Puri, TS., Shakib, MI., Mathew, L., Olayinka, O.,
Minto, AW., Sarav, M. Et.AL. (2010). Chronic
kidney disease induced in mice by reversible
unilateral ureteral obstruction is dependent on
genetic background. Amer Journal of Physiology.
Renal Physiology 298 (4) 1024-1032 - Undisclosed (2005-2010) Fluid balance flashcards.
retrieved from http//quizlet.com March 2010 - Undisclosed Department of molecular and cell
biology.(2010) Fluid and electrolyte balance.
Retrieved http//mcb.berkeley.edu/courses/mcb135e
/kidneyfluid.html April 2010