BASIC OUTLINE - PowerPoint PPT Presentation
1 / 45
Title:
BASIC OUTLINE
Description:
ACUTE RENAL FAILURE IN PREGNANCY BASIC OUTLINE Investigations MANAGEMENT PRINCIPLES Prerenal Vs ATN Vs ACN ROLE OF Nutrition Volume & metabolic control – PowerPoint PPT presentation
Number of Views:306
Avg rating:3.0/5.0
Title: BASIC OUTLINE
1
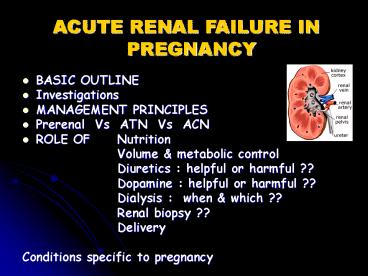
ACUTE RENAL FAILURE IN PREGNANCY
- BASIC OUTLINE
- Investigations
- MANAGEMENT PRINCIPLES
- Prerenal Vs ATN Vs ACN
- ROLE OF Nutrition
- Volume metabolic control
- Diuretics helpful or harmful
?? - Dopamine helpful or harmful
?? - Dialysis when which ??
- Renal biopsy ??
- Delivery
- Conditions specific to pregnancy
2
DEFINITIONS OF ARF
- The syndrome is characterised by a sudden in
parenchymal function (UOPlt400ml/d30ml/hr) which
is usually but not always reversible - This produces disturbance of water, electrolyte,
acid base balance and nitrogenous waste products
blood pressure.
3
Normal Physiologic Alterations of Pregnancy
4
Physiological changes in normal gestation
- Kidney weight and size increase
- Dilation of renal calyces, pelves, and ureters
- Urinary stasis
- Glomerular filtration, effective renal plasma
flow, fractional clearance of urate increase - Bicarbonate reabsorption threshold decreases
5
Clinical relevance
- Concentrations of serum creatinine, urea N, and
uric acid of 0.9, 14, and 5.6 mg/dl, normal in
nonpregnant subjects, are already suspiciously
high in gravid women. - Asymptomatic bacteriuria - frank pyelonephritis.
- PP reduction in size should not be mistaken for
parenchymal loss - Post renal failure difficult to diagnose
- S.bicarb lower,PCO2 10 mmHg lower
6
Causes Early in Pregnancy
- Most common cause is pre-renal failure due to
hyperemesis gravidarum - ATN due to septic abortion
7
Causes - ARF Late in Pregnancy/Postpartum
- Thrombotic microangiopathy
- TTP-HUS
- Severe preeclampsia usually with HELLP syndrome
- Renal Cortical Necrosis
- Placenta previa
- Prolonged intrauterine fetal death
- Amniotic fluid embolism
- Intrinsic renal disease/autoimmune diseaes
8
ARF Late in Pregnancy/Postpartum
- Acute pyelonephritis
- ATN from septicemia or hypotension
- ARF from microabscesses
- Acute fatty liver of pregnancy
- ARF in up to 60 of cases
- Preeclampsia hypoglycemia, hypofibrinogenemia,
LFT abnormalities, prolonged PTT - Obstructive uropathy
- Mild-moderate hydronephrosis is normal
- Occasionally, degree of obstruction sufficient to
cause ARF. - Nephrolithiasis if solitary functioning kidney
9
Causes - Severe Preeclampsia/HELLP
- Typically develops late in 3rd trimester a few
percent of cases can happen up to 48 hours
post-partum. - Preceded by hypertension, proteinuria, and severe
edema - ARF not typical unless marked DIC
10
Severe Preeclampsia/HELLP
- But, there are cases reported in which renal
abnormalities begin post-partum WITHOUT prior
proteinuria - Typically, spontaneous recovery 2-3 days
post-partum complete recovery typical by 8 weeks
post-partum. - Corticosteroids have been utilized but no large
randomized clinical trials
11
Causes - TTP-HUS
- Thrombocytopenia microangiopathic hemolytic
anemia ARF - Traditionally, TTP if neurologic symptoms are
abundant HUS if ARF is dominant. BUT,
distinctions are often unclear and may not be
important for management decisions
12
TTP-HUS
- Timing variable
- 25 before mid-pregnancy
- 65 peri-partum
- 20 postpartum may follow normal pregnancy or
be preceded by findings indistinguishable from
preeclampsia - Can relapse if TTP-HUS occurred once prior to
pregnancy can occasionally relapse in
subsequent pregnancy
13
TTP-HUS
- Plasma infusion /- plasma exchange
(plasmapheresis) - In one series of 11 women
- 2 died
- 4 with residual CKD
- 5 recovered completely
- Prior to use of plasmapheresis, 90 mortality
rate reported
14
Causes - Renal Cortical Necrosis
- Bilateral cortical necrosis
- Severe renal ischemia or DIC with resultant
endothelial damage - Abruptio placenta, placenta previa, prolonged
intrauterine death, amniotic fluid embolism - THEN, patient develops acute onset of oliguria or
anuria, gross hematuria, flank pain, and
hypotension - ANURIA, GROSS HEMATURIA, FLANK PAIN triad that
is unusual in other causes of renal failure
15
Renal Cortical Necrosis
- US or CT can be suggestive
- Biopsy can demonstrate necrosis
- No specific therapy many patients require
dialysis but 20-40 have partial recovery with
CrCl between 15 and 50 mL/min.
16
To summarise Causes
- Bimodal distribution -peaks in the first
trimester (related to unregulated and/or septic
abortion,hyperemesis) and the late third
trimester (related to obstetric complications
APH,PPH,Preeclampsia, Chorioamnionitis,AFE etc).
17
ATN CORTICAL NECROSIS THOMBOTIC
MICROANGIOPATHIES
18
(No Transcript)
19
- The RIFLE classification (ADQI group) of
ARF - Risk (R) - Increase in serum creatinine level X
1.5 or decrease in GFR by 25, or UO lt0.5 mL/kg/h
for 6 hours - Injury (I) - Increase in serum creatinine level X
2.0 or decrease in GFR by 50, or UO lt0.5 mL/kg/h
for 12 hours - Failure (F) - Increase in serum creatinine level
X 3.0, decrease in GFR by 75, or serum
creatinine level gt 4 mg/dL UO lt0.3 mL/kg/h for
24 hours, or anuria for 12 hours - Loss (L) - Persistent ARF, complete loss of
kidney function gt4 wk - End-stage kidney disease (E) - Loss of kidney
function gt3 months
20
PHASES
- OLIGURIA
- POLYURIA
- RECOVERY
21
Investigations
- BLOOD
- CBC
- Urea,creatinine,uric acid
- Electrolytes
- LFT
- S.proteins
- Coagulation profile
- ABG
- RBS
- Osmolality
- URINE
- sp.gravity
- osmolality
- electrolytes
- proteins
- pigment casts
- c/s
- ECG
22
Management
- Restore or maintain fluid balance
- The maintenance of electrolytes and acid base
balance - The maintenance of nutritional support
- Prevention of infection
- Avoid renal toxins (including NSAIDS)
- Instigate renal replacement therapies
23
Prerenal failure
- Adequately replace blood fluid losses,maintain
BP. - Control continuing blood loss
- Mannitol (100ml, 25) trial to d/d b/w reversible
prerenal failure established ATN (provided
oliguria lt48 hrs UP osmolality gt 1.05) - If diuresis (gt50ml/hr or doubling) established
within 3 hrs,maintain NS infusion acc to UOP
replace electrolytes acc to urinary loss
estimations. - If unsuccessful objective is to support the
functionally anephric pt till kidneys recover.
24
Volume control
- IP/OP charting daily
- State of hydration-wt,hct,protein
- Input Output/24hrs 500ml(nonfebrile)
- 200 ml/ deg C of inc. in Tem
- Balance 0.3-0.5kg wt loss/d
- Avoid overhydration Rx diuretics,dialysis
- CVP monitoring (b/w 10-15cm H2O)
25
Diuretics
- Diuretics commonly have been given
in an attempt to convert the oliguric state to a
nonoliguric state. However, diuretics have not
been shown to be beneficial, and they may worsen
outcomes. - In the absence of compelling contradictory data
from a randomized, blinded clinical trial, the
widespread use of diuretics in critically ill
patients with acute renal failure should be
discouraged. - Useful only in management of fluid-overloaded
patients
Cantarovich F, Rangoonwala B, Lorenz H, Verho M,
Esnault VL. High-dose furosemide for established
ARF a prospective, randomized, double-blind,
placebo-controlled, multicenter trial. Am J
Kidney Dis 200444402-9. Kellum JA.
Systematic review The use of diuretics and
dopamine in acute renal failure a systematic
review of the evidence. Critical
Care19971(2)539.
26
DOPAMINE
- Dopamine traditionally has been used to promote
renal perfusion(1-5 mcg/kg/min ) - However, systematic reviews of dopamine
treatment in critically ill patients and in
patients with sepsis do not support the use of
dopamine to prevent renal insufficiency,
morbidity, or mortality. In the majority of ARF
studies, dopamine was associated only with an
increase in urine output.
Kellum JA, Decker MJ. Use of dopamine in acute
renal failure a meta-analysis. Crit Care Med
2001291526-31. Denton MD, Chertow GM, Brady
HR. "Renal-dose" dopamine for the treatment of
acute renal failure scientific rationale,
experimental studies and clinical trials. Kidney
Int 1996504-14.
27
Nutrition
- INTAKE
- 1500 cal (protein free)
- Oral/parenteral
- If vol limitation-50D via central vein
- Essential L-aminoacids K,Mg,PImprove wound
healing, hasten recovery - Protein intake of 0.6 g per kg per day
28
Electrolyte acid-base correction
- Hyperkalemia, which can be life-threatening,
should be treated by - decreasing the intake of potassium,
- delaying the absorption of potassium,
- exchanging potassium across the gut lumen using
potassium-binding resins, - controlling intracellular shifts
- dialysis.
- Acidosis- sodabicarb ,dialysis
29
- Treat coagulopathy with FFP for a prolonged aPTT,
cryoprecipitate for a fibrinogen level less than
100 mg/dL, and transfuse platelets for platelet
counts less than 20,000/mm3 - Timely identification of UTI, proper treatment
prevention using prophylactic antibiotics
30
Should we Initiate Dialysis in Pts w/Low Cr
Clearance?
- Hou, S., Pregnancy in Women on Hemodialysis,
1994, revealed better outcomes of pregnancy in
women w/ significant residual renal function or
who initiate pregnancy before they need dialysis. - May reduce incidence of polyhydramnios, lower
urea and lowers water load, also reducing risk of
dialysis-induced hypotension
31
Hou, et al, 1998
32
Hou, et al, 1998
33
Hou, et al, 1998
34
Indications for Kidney Replacement Therapy
- Acidosis unresponsive to medical therapy
- Acute, severe, refractory electrolyte changes
(e.g., hyperkalemia) - Encephalopathy
- Significant azotemia (blood urea nitrogen level
gt100 mg per dL 36 mmol per L) - Significant bleeding
- Uremic pericarditis
- Volume overload
35
Early Prophylactic Dialysis
- Allows more liberal fluid, protein salt intake.
- Prevent hyperkalemic emergencies.
- infectious Cx.
- Improves comfort survival
36
Hemodialysis Vs Peritoneal
dialysis
- Limited usefulness if hypotension
- C/I in actively bleeding pt.
- Controlled anticoagulation reqd
- Volume shifts-careful
- Faster correction
- Can be used in preg/PP pt.
- Easily available
- Simple,inexpensive
- Lower Cx rate
- Minimises rapid metabolic pertubations fluid
shifts - Insert cath high direct vision
37
Delivery
- Development of ARF in obs pt is indication of
delivery in majority cases. - Deliver if UOPlt20 ml/gt2hrs despite adequate vol
expansion immediate delivery not expected - Redistribution of CO better renal perfusion.
- Remove fetus from hostile environment.
- Neonate urea osmotis diuresis -dehydration
38
Renal biopsy
- Potentially v.risky in pregnancy
- Defer until postpartum even if ACN( for
prognostication). - Rare indication sudden renal failure before 32
wks with no obvious cause.
39
Preeclampsia
- A decrease in the GFR occurs secondary to
intrarenal vasospasm. This may manifest as a
"prerenal" picture. Acute renal failure (ARF) may
develop, and acute tubular necrosis (ATN) may
ensue if this hypoperfusion persists.
40
Pre-eclampsia ManagementRenal problems
- Hyperuricaemia and proteinuria are NOT
indications for delivery per se - Consider delivery for progressive renal
impairment (creatinine gt0.09 mmol/L) - Care with fluids (pulmonary oedema can kill!)
- Kidney Function is Criticalfor Drug Elimination
41
Pre-eclampsiaInvasive monitoring
- CVP monitoring may NOT be helpful!
- poor correlation between CVP and PCWP
- PA catheters have risks!
- rare indications
- pulmonary oedema resistant to diuretics
- oliguric renal failure despite volume expansion
42
Idiopathic postpartum renal failure
- Associated primarily with microangiopathic
processes - Postpartum hemolytic-uremic syndrome.
- These were often irreversible and were
associated with substantial mortality. - Now improved outcome with plasma
exchange,dialysis,prostacyclin infusion,
correcting coagulopathy
43
ACUTE FATTY LIVER OF PREGNANCY
- Associated with acute renal failure in up to
60 percent of cases. - The diagnosis should be suspected in a woman
with preeclampsia who has jaundice,hypoglycemia,
hypofibrinogenemia, and a prolonged PTT in the
absence of abruptio placentae.
44
KEY RECOMMENDATIONS FOR PRACTICE
- Identify prevent at prerenal phase as early as
possible - Dopamine should not be used to prevent
- acute renal failure. (Evidence level A)
- Diuretics should not be used to treat oliguria in
patients with acute renal failure unless volume
overload (Evidence level B) - Early prophylactic dialysis should be strongly
considered. - The maintenance of electrolytes,acid base balance
nutritional support plays vital role.
45
- THANK YOU