Patient-Centered Outcomes Research Institute ( - PowerPoint PPT Presentation
1 / 13
Title:
Patient-Centered Outcomes Research Institute (
Description:
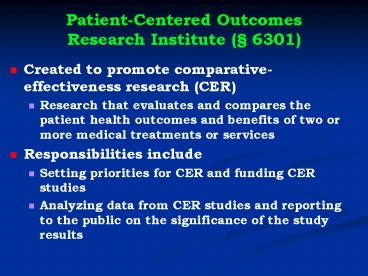
Patient-Centered Outcomes Research Institute ( 6301) Created to promote comparative-effectiveness research (CER) Research that evaluates and compares the patient ... – PowerPoint PPT presentation
Number of Views:143
Avg rating:3.0/5.0
Title: Patient-Centered Outcomes Research Institute (
1
Patient-Centered OutcomesResearch Institute (
6301)
- Created to promote comparative-effectiveness
research (CER) - Research that evaluates and compares the patient
health outcomes and benefits of two or more
medical treatments or services - Responsibilities include
- Setting priorities for CER and funding CER
studies - Analyzing data from CER studies and reporting to
the public on the significance of the study
results
2
Patient-Centered OutcomesResearch Institute (
6301)
- The Institute may not recommend coverage changes
or other policies based on its analyses, but - Medicare and Medicaid may consider the
Institutes analyses in determining coverage
policies as long as - No denial of coverage solely on the basis of
CER - Coverage decisions do not treat the lives of
elderly, disabled or terminally ill persons as
having lower value
3
Can the CER institute become our NICE?
- NICE evaluates the cost-effectiveness of medical
therapies and approves those that are
sufficiently cost-effective for Britains
National Health Service - Treatments are cost-effective if they provide 1
QALY for no more than 20,000 (now 31,250) - Sometime, NICE approves treatments up to 30,000
(46,900) per QALY - Rarely, NICE approves treatments beyond 30,000
per QALY - NICE has approval authority, while the CER
institute can only issue reports (though NICE
authority supposed to be eliminated) - CER institute shall not develop or employ a
dollars-per-quality adjusted life year . . . as a
threshold nor shall HHS employ such a measure as
a threshold for coverage.
4
Whats a good buy?
Expensive more than 100,000/QALY Reasonable
50,000/QALY (UK upper limit
47,000) Very Efficient less than
25,000/QALY Most writers use 50-100,000 as
upper limit of good value, but public preferences
suggest upper limit over 200,000 Hirth RA, et
al., Medical Decision Making. 200020332-342
5
Some sample QALYs (2002 dollars)Harvard Public
Health Review (Fall 2004)
- lt 0 (If the cost per QALY is less than zero, the
intervention actually saves money) - Flu vaccine for the elderly
- Under 10,000
- Beta-blocker drugs post-heart attack in high-risk
patients - 10,000 to 20,000
- Combination antiretroviral therapy for certain
HIV patients - 15,000 to 20,000
- Colonoscopy every five to 10 years for women age
50 and up - 20,000 to 50,000
- Antihypertensive medications in adults age 35-64
with high blood pressure but no coronary heart
disease - Lung transplant in UK (Anyanwu AC et al. J Thorac
Cardiovasc Surg 2002123411-420) - 50,000-100,000
- Dialysis for patients with end-stage kidney
disease - Antibiotic prophylaxis during dental procedures
for persons at moderate to high risk of bacterial
endocarditis (88,000) (Med Decis Making.
200525(3)308-20) - Over 500,000
- CT and MRI scans for kids with headache and an
intermediate risk of brain tumor
6
COST/QALY Selected Medicare services
7
Cost of treatment for metastatic colon
cancer(Schrag D. NEJM. 2004351317-319)
8
Examining the cost and cost-effectiveness of
adding bevacizumab (Avastin) to chemo in
metastatic colon cancer
- Randomized trial compared chemotherapy alone vs.
chemotherapy bevacizumab - Bevacizumab regimen prolonged median survival
from 15.6 to 20.3 months (plt0.001) - Cost of extra 4.7 months?
- 101,500 (assuming 5,000 per month for
bevacizumab) - 259,149 per year of life gained (not quality
adjusted) - NICE decided not to recommend for NHS coverage
9
Examining the cost and cost-effectiveness of
adding bevacizumab (Avastin) to chemo in advanced
non-small cell lung cancer
- Randomized trial compared chemotherapy alone vs.
chemotherapy bevacizumab - Bevacizumab regimen prolonged median survival
from 10.2 to 12.5 months (p0.007) - Cost of extra 2.3 months?
- 66,270-80,343
- 345,762 per year of life gained (assuming
66,270 cost) - Grusenmeyer PA, Gralla RJ. J. Clin. Oncology.
200624(18S)6057.
10
Can we make QALY-based decisions?
- Cost-effectiveness decisions are controversial
- Prohibited under PPACA from being used as sole
basis for denying coverage in federal programs
(6301) - Oregon Health Care Plan
- Ended up with fairly generous basic coverage
- Mammography screening guidelines in 2009 (even
though cost wasnt a factor) - US Preventive Services Task Force recommended
that routine screening begin at age 50 instead of
age 40 - The tragic choices problem
- Its difficult to make life-and-death decisions
openly
11
Cost containment strategies
- If main drivers of high costs are physician
incentives to provide excessive care and patient
incentives to demand excessive care, we should
employ policy changes to remove these incentives - Changes in physician incentives
- Salary or capitation for physicians (combined
with quality measures to avoid under-provision of
care)could increase physician pay and still
lower overall costs - Capitation would address problem of too many
prescriptions for expensive drugsCER institute
important here too - Limits on hospital beds, surgical suites, MRI
scanners and other facilities
12
Financial incentives for patients?
- If people are not sufficiently sensitive to costs
because of insurance, should we use health
savings accounts or other mechanisms to give
patients more skin in the game? - Raising out-of-pocket costs reduces patient
demand for care, but - Patients do not always distinguish between
necessary and unnecessary care - Caps on out-of-pocket costs prevent patient
sensitivity to costs of high-cost services (e.g.,
heart surgery, cancer chemotherapy) - Buntin et al. 2006
13
What is a QALY?
0
1
Perfect health
Dead