Cervical Region: Considerations for HVLA PowerPoint PPT Presentation
1 / 78
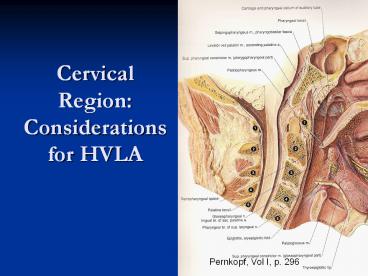
Title: Cervical Region: Considerations for HVLA
1
Cervical Region Considerations for HVLA
Pernkopf, Vol I, p. 296
2
1 of 2
- Ground Rules for todays session
- If you have not had an introduction to HVLA, you
will not be performing cervical HVLA today. - If your partner does not give his/her consent for
HVLA for a diagnosed dysfunction in his/her neck,
you will not be performing HVLA on that
individual.
3
2 of 2
- Ground Rules for todays session
- However, you will get experience in localizing
forces to a dysfunctional cervical segment - Then using Incremental Mobilization or Muscle
Energy treatment - Which can ultimately be preparatory for HVLA.
4
Clinical
- Etiology of cervical somatic dysfunction
- Postural imbalance
- Tightness prone/weakness prone
- Traumatic cranial somatic dysfunction
- Cervical trauma- whiplash
- Chronic inflammatory conditions
- Repetative injury
- EENT pathology
- Visceral-C2 -vagus
- Diaphragm-C3-5- phrenic
- Superior Thoracic Aperture Dysfunction
- Sacro-pelvic dysfunction
5
Clinical Syndromes
- Cervicocephalic-Pain and motion restriction upper
C-spine and associated superficial and deep pain
in head - Visual changes, vertigo, dizziness, nystagmus
- Cervical-Painful stiffness of neck
- Mild to acute spastic torticollis
- Cervicobrachial-Painful stiffness C-spine with
symptoms in shoulder girdle and upper extremity - Upper Extremity-brachial plexus, arterial,
venous, lymphatic - Thoracic Inlet-1st 2nd ribs, T-spine, ribs, T5-6
6
American Osteopathic Association Position Paper
On Osteopathic Treatment of the Cervical Spine
- Conclusion
- it is the position of the AOA that all
modalities of osteopathic manipulative treatment
of the cervical spine, including HVLA, should be
taught at all levels of education, and that
osteopathic physicians should continue to offer
this form of treatment.
Adopted by the AOA House of Delegates, July 17,
2004
7
Benefits
- Vagus nerve visceral component
- Phrenic nerve diaphragm
- Vertebral artery
- Lymphatic drainage
- Head region dysfunction
8
Complications
- RARE
- Usually reported in connection with HVLA
- Neurovascular accidents
- Aggravation of disc problem
- Fractures
- Vertigo
- Reasons
- Lack of skill
- Diagnostic error
- Inappropriate use of force
- Avoiding Complications
- Avoid overextension
- Diagnose accurately
- Dont force beyond tolerance
- Re-evaluate diagnosis and treatment method
9
Contraindications
- Muscle Energy
- Low vitality
- Unable to follow commands
- Mobilization with Impulse
- Absolute
- Osteoporosis/Osteomyelitis/Fracture
- Rheumatoid Arthritis/Downs
- Weakness transverse ligament
- Relative
- Acute Whiplash
- Pregnancy
- Post OP
- Herniated Nucleus Propulsus
- Anticoagulants
- Vertebral Artery Ischemia
10
Anatomic Considerations for Cervical Treatment
11
Autonomics
- Superior cervical ganglion
- Sympathetic control cervical blood flow
- Bound by deep connective fascia
- Cervical nerves 1-8
- Exit above the vertbra for which they are named
Except CN8, which leaves the spinal canal below
C7 - C2-Small branch connects to Vagus
- Internal visceral disease
- C3-5-Phrenic
- Diaphragm Dysfunction
- Brachial and cervical plexuses
- Mechanoreceptors/Nociceptors/Muscle spindles
- Postural proprioceptors
12
Cervical Anatomy
- It is the one to two segment muscles, in
particular, (along with the function of the
zygapophyseal joint and the capsular structures)
we wish to influence with articular dysfunction
in the cervical spine
Hollingshead, p.136
13
Deep muscles posterior
- Rectus capitis posterior major
- Rectus capitis posterior minor
- Obliquus capitis superior
- Obliquus capitis inferior
- Interspinalis
- Intertransversii
Notice that these muscles controlling the
individual motions in the cervical spine are
small and short.
14
Deep muscles anterior
- Obliquus caqpitis superior
- Obliquus capitis inferior
- Longus colli
- Rectus capitis lateralis
- Rectus capitis anterior
15
Intermediate muscles
Multi-Joint Muscles If these Muscles are
Tight/Tender, Some of the Regional Stretches May
Prepare the Patient for Local Treatment
16
Superficial Muscles
Multi-Joint Muscles If these Muscles are
Tight/Tender, Some of the Regional Stretches May
Also Prepare the Patient for Local Treatment
17
These muscles are often forgotten.
18
Cervical Review
- Facet surfaces always in contact unless traction
applied - No physiologic neutral facets not engaged
- Movement determined by plane and contour of facet
surfaces
19
- Articular pillars
- With Superior Facets facing Backward Upward and
Medial Rotation Requires Sidebending to the Same
Side (and Visa Versa)
CIBA, vol. 8, part 1, p.10
20
Determinates of Motion
- Joint configuration and intervertebral disc
- Allow movement in all directions
- Load bearing
- Facing of zygapophysial joints
- Plane and contour of facet surfaces
- Characteristics of vertebral bodies and discs
- Fryettes Third Principle
- Initiation of motion of a vertebral segment in
any plane of motion will modify the movement of
that segment in other planes of motion
21
Uncovertebral Joints-Joints Of Luschka
- Posterolateral corner vertebral bodies
- Function in gliding movements/limit lateral
translation
Cailliet, Functional Anatomy of the
Musculoskeletal System
22
Cailliet, Functional Anatomy of the
Musculoskeletal System, p. 99
23
1 of 2
- Planes of facets not parallel
- Meet near tip of SP of C7
- Angles of planes increase upward
- 10-60 degrees-avg. incline of 45 degrees
CIBA, Vol. 8, p. 11
24
C2-7
- Facet joints support 1/3 weight of head
- Bodies articulate through intervertebral disc and
synovial joints - Unless traction applied- no pure rotation or
sidebending - Sidebending and rotation occur to same side
25
C2-7
- Flexion
- Inferior facet slides superior and anterior on
superior facet of vertebra below - Anterior translation of body
- Extension
- Inferior facet slides inferior and posterior on
superior facet below - Posterior translation of body
- A-P lordotic curve
26
Palpatory Exercise
- Feel the motion of the facets contacting your own
neck with fingers on several consecutive levels. - Cervical Flexion
- Feel how the facet of the superior vertebra lifts
superior and forward - Cervical Extension
- Feel how the facet of the superior vertebra drops
inferior and posterior
27
Clinical
- Etiology of cervical somatic dysfunction
- Postural imbalance
- Tightness prone/weakness prone
- Traumatic cranial somatic dysfunction
- Cervical trauma- whiplash
- Chronic inflammatory conditions
- Repetative injury
- EENT pathology
- Visceral-C2 -vagus
- Diaphragm-C3-5- phrenic
- Superior Thoracic Aperture Dysfunction
- Sacro-pelvic dysfunction
28
- Cervical treatment is not necessarily the first
step for a cervical complaint. - Superior Thoracic Aperture Dysfunction may be
part of the source of cervical complaints - Thoracic
- Upper Rib
- Upper Extremity should be evaluated
- Sacral Dysfunction may also contribute
29
Diagnosis Lateral Translation
- Test for SB mobility
- Passively move superior vertebrae
- Translation Opposite SB
- Flexion- translation resistance-impaired joint
opposite side of SB resistance - Extension- translation resistance- impaired joint
on same side of SB resistance
30
Lateral Translation Test
- Patient supine
- Physician seated at head of table
- Support occiput on palms
- Place index fingers on C2 to start
- Finger pads contact articular pillars
- Maintain the neck without introducing flexion or
extention
31
- Planes visualized with spine in the supine
position
- Fingerpad contact on the lateral aspect of the
articular pillar
CIBA, Vol. 8, p. 11
32
Lateral Translation for Sidebending Mobility
0
- Translate L and R
- Passively move superior vertebrae
- By pushing the vertebra with each finger pad
contact sequentially - Monitor distance-
- compare sides
- Repeat in flexion
- and extension
- may use proximal
- phalanges for ext.
- Repeat at each
- cervical level
Mitchell, ME Manual Vol.1
33
Lateral Translation Test Results
- Equal ROM no restriction or b/l rest.
- Rare both restricted
- FRSR or FRSL
- ERSR or ERSL
For Optimal Treatment of these two, it is
important to determine which facet joint is stuck.
34
Why is the knowledge of which facet joint is
stuck important?
- For the purposes of treatment it helps the
physician interpret the resistance felt. - This helps the localization process and setting
up the vector for the activating force. - For Incremental Mobilization, this provides a
better focus of attention for the response to the
palpating fingers movement input. - For HVLA, this means less force is required when
the thrust is performed.
35
Which facet joint is restricted?
- C2-7 Lateral Translation Test Translation
Resistance Left or Right with the Head in Flexion
or Extension gt Diagnosis (FSleftRright,
ESleftRright, etc.) - Example C4 ERSR (ERSright)
- See next slide.
36
Step 1 Make your Diagnosis
- Resists Translation from the left toward the
right while the head is flexed. - Therefore it resists Left sidebending
- Which tells the position of ease for the
diagnosis Sidebent Right - Sidebent Right at the C2-7 requires Rotation
Right.
Adapted from Mitchell, Vol. I, p.195
- Therefore the diagnosis is C4 ERSR (ERSright)
37
Which facet joint is restricted?
- Which direction do the facets of the superior
vertebra have to go with the head/neck
positioned into the resistance (restriction)?
Superior-Anterior or Inferior-Posterior - Example continued C4 ERSR (ERSright)
- See next slide.
38
Step 2 Direction of Facet Motion with Head in
Position of Translation Resistance
Adapted from Mitchell, Vol. I, p.195
- Example Diagnosis C4 ERSR (ERSright)
- Flexion is the Head/Neck Position in which
Translation Resistance Was Encountered at C4.
- Facets of the superior vertebra have to go
superior-anterior
39
Which facet joint is restricted?
- Use the diagnosed direction of rotation to
determine which facet of the superior vertebra
must move to create that motion. - Example continued C4 ERSR (ERSright)
- See next slide.
40
Step 3 Direction of Facet Motion with Head in
Position of Translation Resistance
Adapted from Mitchell, Vol. I, p.195
- Example Diagnosis C4 ERSR (ERSright)
- According to the Diagnosis C4 rotates Right
- Which Facet of the Superior Vertebra Must Move
For This To Happen? - In Head/Neck Flexed Position the facets of the
superior vertebra are moving Anterior. - The Left Facet must move anterior for Right
Rotation to occur.
- Therefore, the Right facet joint is the
restricted joint. It is stuck inferior-posterior.
41
Which facet joint is restricted?
- C2-7 Lateral Translation Test Translation
Resistance Left or Right with the Head in Flexion
or Extension gt Diagnosis (FSleftRright,
ESleftRright, etc.) - Which direction do the facets of the superior
vertebra have to go with the head positioned
into the resistance (restriction)?
Superior-Anterior or Inferior-Posterior - Use the diagnosed direction of rotation to
determine which facet of the superior vertebra
must move to create that motion.
42
Lateral Translation Test Results
- Restriction with Extension
- Facet joint stuck on same side as translation
resistance - Will not translate right/sidebend left when
extended.
X
FRSR
Mitchell, Vol. I, p.195
43
Lateral Translation Test Results
- Restriction with Flexion
- Facet joint stuck on opposite side as restricted
translation- cant glide anterior - Will not translate right/sidebend left when
flexed.
X
ERSR
Mitchell, Vol. I, p.195
44
Test with Head Neck Flexed
- If cannot translate vertebra L, then
- Diagnosis- ERSleft
- Cannot sidebend R
- L facet cannot slide forward, so rotation L
occurs - L facet posterior
- Free movements
- Extension,Left sidebending rotation
- If cannot translate vertebra R, then
- Diagnosis- ERSright
- Cannot sidebend L
- R facet cannot slide forward, so rotation R
occurs - R facet posterior
- Free movements
- Extension, Right sidebending rotation
45
Test with Head Neck Extended
- If cannot translate vertebra L, then
- Diagnosis- FRSleft
- Cannot sidebend R
- R facet cannot slide backward, so L rotation
occurs - R facet anterior
- Free movements
- Flexion,Left sidebending rotation
- If cannot translate vertebra R, then
- Diagnosis- FRSright
- Cannot sidebend L
- L facet cannot slide backward, so R rotation
occurs - L facet anterior
- Free movements
- Flexion, Right sidebending rotation
46
Implications for Treatment
- FRSR Rotational Activating forces need to be
directed toward the left facet and articular
pillar from a right sided contact. - Rotational Force Directed Toward the Facet
Opposite the Sidebending Preference - Side Bending Force
- The left facet joint needs to be closed.
MCP
FRSR
Mitchell, Vol. I, p.195
47
Implications for Treatment
- FRSR Side Bending Activating forces need to be
directed toward the left facet and articular
pillar from a left sided contact. - Side Bending Force Directed Toward the Facet
Opposite the Sidebending Preference - The left facet joint needs to be closed. You are
pushing the bottom facet back under the top
facet.
MCP
FRSR
Mitchell, Vol. I, p.195
48
Implications for Treatment
- ERSR Rotational Activating forces need to be
directed toward the right facet and articular
pillar - Rotational Force Directed Toward the Facet On
the Same Side As the Sidebending Preference - The right facet joint needs to be opened.
MCP
ERSR
Mitchell, Vol. I, p.195
49
Implications for Treatment
- ERSR Side Bending Activating forces need to be
directed toward the right facet and articular
pillar from a left sided contact. - Side Bending Force Directed Toward the Facet On
the Same Side As the Sidebending Preference from
the Opposite Side
MCP
ERSR
- The right facet joint needs to be opened.
Mitchell, Vol. I, p.195
50
Lateral Translation Test Results
- Restriction with Extension
- Facet joint stuck on same side as translation
resistance - Will not translate right/sidebend left when
extended.
X
FRSR
51
Lateral Translation Test Results
- Restriction with Flexion
- Facet joint stuck on opposite side as restricted
translation- cant glide anterior - Will not translate right/sidebend left when
flexed.
X
ERSR
52
TREATMENT
53
Incremental Mobilization I
- Use the cephalad hand to gently cup the occiput
- Cervical spine held in neutral
- Use the thumb and index (or middle finger) to
contact the articular pillars starting at C2 - Cephalad Hand add cephalad traction down into
the dysfunctional segments facet articulations
(to disengage the facets)
54
Incremental Mobilization I
- Caudad Hand introduce rhythmic translatory
motion left and right - Visualize the angle of the plane of the facets at
that level - Visualize the vector of force going through the
plane of the facets. - Visualize the activating force going into the
stuck facet joint - Repeat with cervical spine flexed, then extended
- Repeat with C3, C4, etc.
55
- Planes visualized with spine in the supine
position
- Fingerpad contact on the lateral aspect of the
articular pillar
CIBA, Vol. 8, p. 11
56
HVLA (Mobilization with Impulse)
- Progress through the steps of preparation and
localization. - Have an instructor confirm your localization
- If your patient and instructor agree, proceed
with mobilization - If you have not used HVLA before, use only
incremental mobilization.
57
Preparation for HVLA in the Cervical Region
- Regional Soft tissue
- Indirect Techniques
- Muscle Energy
- Incremental Mobilization
- One or several may be necessary or may be
desirable. - Use of these will allow easier localization and a
lesser activating force.
58
Contact for HVLA
- The Metacarpophalangeal joint/proximal phalanx of
the index finger is used to contact - AA, C2-7 the vertebra of interest
- OA the occiput
59
Direction of Force
- C2-7
- C2-4 Rotary impulse
- C4-7 Side Bending impulse
- AA Rotary impulse
- OA Impulse directed toward the opposite orbit
- The forearm elbow are lined up with the
direction of force (like the shaft of the arrow,
pointing in the direction of the thrust).
60
HVLA Principles
- Check your body position/comfort.
- Engage the resistance gently.
- It should feel like the tension is focused in an
area no larger than the size of a nickel. If
that is not the case - Get further patient relaxation.
- More soft tissue preparation?
- Recheck diagnosis
- Refine the localization.
- Thrust.
- Recheck.
61
Patient Relaxation
- Patients rarely relax fully before a thrust in
the cervicals. - Localize approximately, then
- Instructions that are helpful
- Ask the patient to take a deep breath in, then
slowly let it out. - As the patient lets the breath out ask him/her to
let the head and neck drop toward the table - Fine Tune the localization, then thrust (Low
Amplitude quick, but gentle.
62
Patient Relaxation
- During the patients relaxation response it is
helpful to dance up to the localized barrier
and dance back from it. - Find the barrier, but dont stay on it.
- You now know where it will be found with the next
relaxation cycle. - With the next relaxation breath and head release
toward the table the thrust can then be done with
more precision
63
Patient Relaxation
- It may be helpful for localization to have the
patient nod the chin or raise the chin just a
little. - This can improve patient relaxation.
- It can help focus localization so that less
activating force is necessary.
64
Unsuccessful Correction of Somatic Dysfunction in
the Cervical Region
- Practitioner Error
- Wrong Diagnosis
- Insufficiently localized
- Insufficient tissue preparation
- Inappropriate force
- Inter-regional Considerations
- Superior thoracic aperture dysfunction (S.D.) may
be primary - Thoracic S.D. may be primary
- Upper Extremity tensions dysfunction may be
influencing the area - Upper cervical segments can be influenced by
sacral dysfunction or cranial base dysfunction.
65
SUMMARY
66
References
- Mitchell, Jr. Fred L. The Muscle Energy Manual,
Volume One. East Lansing, Michigan MET Press
1995 pp158-201
67
References
- Greenman P. Principles of Manual Medicine. 3rd
ed. Philadelphia Lippincott Williams Wilkins
2003 195-199, 202-223. - Mitchell F. The Muscle Energy Manual, Vol. 1.
East Lansing, MI MET Press 1995 143-153,
192-211. - DiGiovanna E, Schiowitz S, Dowling D. An
Osteopathic Approach to Diagnosis and Treatment.
3rd ed. Philadelphia Lippincott-Raven
Publishers 2005 127-128, 138-139,169-172. - Kimberly P. Outline of Osteopathic Manipulative
Procedures The Kimberly Manual. Millennium ed.
Marceline Walsworth Publishing Co 2000 37-40,
73-80. - Cailliet R. The Illustrated Guide to Functional
Anatomy of the Musculoskeletal System. AMA Press
2004 85-111.
68
American Osteophathic Association Position Paper
On Osteopathic Treatment of the Cervical Spine
1 of 9
- Conclusion
- Therefore, it is the position of the AOA that
all modalities of osteopathic manipulative
treatment of the cervical spine, including HVLA,
should be taught at all levels of education, and
that osteopathic physicians should continue to
offer this form of treatment.
Adopted by the AOA House of Delegates, July 17,
2004
69
AOA Position Paper- Cervical Spine Treatment
2 of 9
- Acknowledged Benefits
- Relief of acute neck pain
- Reduction of subacute or chronic neck pain
- Short-term relief of tension headache
- Relief of cervicogenic headache
- Relief of acute migraine symptoms
70
AOA Position Paper- Cervical Spine Treatment
3 of 9
- Potential Harm
- Neck strain
- Estimated Risk of Major Impairment Following
Cervical Spine Manipulation 6.39 per 10 Million
(est. 33 million manip/yr) - Cervical disc herniation
- Vertebrobasilar accident
71
AOA Position Paper- Cervical Spine Treatment
4 of 9
- Potential Harm
- Vertebrobasilar accident
- Spontaneous occurrence nearly twice the risk from
cervical manipulation
72
AOA Position Paper- Cervical Spine Treatment
5 of 9
- Comparison with Alternative Treatments
- NSAIDS 2500 deaths per year d/t GI
complications 15th most common cause of death - Epidural Steroid Injections .6-10 complication
rate
73
AOA Position Paper- Cervical Spine Treatment
6 of 9
- Provacative Tests
- Unreliable for demonstrating reproducibility of
ischemia or risk of injuring the vertebral
artery.
74
AOA Position Paper- Cervical Spine Treatment
7 of 9
- Risk Factors
- Most Common Risk Factors for VBA
- Migraine
- Hypertension
- Oral Contraceptives
- Smoking
75
AOA Position Paper- Cervical Spine Treatment
8 of 9
- Risk Factors
- Cervical Extension has not proven to be a
prominent risk factor, as previously
hypothesized. - It is still important to minimize extension
elements in treatment. - See next slide
76
Vertebral Artery
9 of 9
- Risk at acute angulation at C6-7
- Changes at intertransverse foramen C7-1
- OA junction changes
- Can narrow 90 on contralateral side with
rotation - Caution- Down syndrome, RA, agenesis odontoid
process, fx odontoid, congenital asymmetry,
atresia
77
Vertebral Artery
- Foraminal passage for the vertebral artery is
decreased by as much as 35 when the cervical
column is extended - Avoid overextension when palpating, diagnosing
and manipulating the cervical spine
78
Articulation of the Cervical Spine
- Figure of 8 Articulatory Technique
- Kimberly, Paul E. Outline of Osteopathic
Manipulative ProceduresThe Kimberly Manual.
Millennium ed. Marceline Walsworth Publishing
Company 2000 p 73-74