Stages of labor
1 / 44
Title: Stages of labor
1
Stages of labor
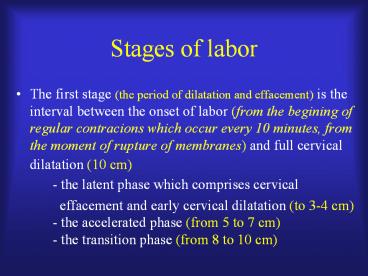
- The first stage (the period of dilatation and
effacement) is the interval between the onset of
labor (from the begining of regular contracions
which occur every 10 minutes, from the moment of
rupture of membranes) and full cervical
dilatation (10 cm)
- the latent
phase which comprises cervical - effacement and early cervical dilatation
(to 3-4 cm) - the accelerated phase (from
5 to 7 cm) - the
transition phase (from 8 to 10 cm)
2
Stages of labor
- The second stage (the period of expulsion) lasts
from complete cervical dilatation till the
delivery of the infant - The third stage (the placental stage) begins
immediately after delivery of the infant and ends
with the delivery of the placenta - The fourth stage is defined as the early
postpartum period of approximately 2 hours after
delivery of the placenta. During this period the
patient undergoes significant physiologic
adjustment and must be under close medical control
3
Abnormal labor - dystocia(difficult labor)
- It results when
- - anatomic or functional abnormalities of the
fetus - - abnormalities of the maternal bony pelvis
- - abnormalities of the uterus and cervix
- - or combination of these abnormalities
- interfere with the normal course of labor
- Abnormal labor describes complications of the
normal labor process slower than normal progress
or a cessation of progress
4
Abnormal labor (or dystocia) is divided into-
prolongation disorders - arrest disorders
5
Patterns of abnormal labor - dystociaA
prolonged latent phaseA latent phase of labor
is abnormal when it lastsgt 20 hours in
primigravid patientsgt 14 hours in multigravid
patientsThe causes of such situation-
abnormal fetal position- unripe cervix-
administration of excess anesthesia- fetopelvic
disproportion- disfunctional uterine
contractions
6
A prolnged latent phase does not itself pose a
danger to the mother or fetus.Some patients who
are initially thought to have a prolonged latent
phase turn out only to have false labor.
7
Patterns of abnormal labor - dystociaA
prolonged active phase
- An active phase is abnormal when it lasts longer
than - - 12 h in the primigravid patients
- - 6 h in the multigravid patients
- or when the rate of cervical dilatation is less
than - - 1,2 cm/h in primigravid patients
- - 1,5 cm/h for multiparas
- or when descend of the presenting part is less
than - - 1,0 cm/h for primigravidas
- - 1,5 cm/h for multiparas
8
Causes of prolonged active phase - abnormal
fetal position - fetopelvic disproportion -
excessive use of sedation - inadequate
contractions - rupture of fetal membranes before
the onset of active labor
9
Patterns of abnormal labor- dystociaArrest
disorders
- Secondary arrest of dilatation
- no cervical dilatation for gt 2 h in any
case in the active phase of labor - Arrest of descend
- no descent of the presenting part in gt
1 h in the second stage of labor
10
It occurs when- the contractions are no longer
sufficient to maintain the progress of labor
orthe labor arrests in spite of adequate
uterine contractions associated with- too large
fetus- fetal lie or position that prevents
progress in labor- too small or abnormally
shaped pelvis
11
Correct diagnosis and management of abnormal
labor requires evaluation of the mechanisms of
labor- the power (uterine contractions)- the
passenger (fetal factors - presentation, size)-
the passage (maternal pelvis)
12
Evaluation of the power includesstrenght,
duration and frequency of uterine contractions
- - manual palpation of the maternal abdomen during
- a contraction (subjective evaluation)
- - external tocography (more objective) - a
tocodynamometer is an - external strain gauge, which is placed on the
maternal abdomen, it records - when the uterus tightnes and relaxes but does
not directly measure how - much force the uterus is generating for a
given contraction - - internal tocography (the most objective) - an
intrauterine pressure - catether is placed into the uterine cavity and
it transmits the actual - intrauterine pressure to the external strain
gauge, which then records - duration and frequency as well as the strength
of the contractions
13
For cervical dilatation to occur, each
contraction must generate at least 25 mm Hg of
pressure. The optimal intrauterine pressure
during contraction is 50-60 mm Hg.In generating
a normal labor pattern the frequency of
contractions is also very important. A minimum
three contractions in a 10 minute window is
usually considered adequate.
14
During the first stage of labor arrest of labor
should not be diagnosed until the cervix is at
least 4 cm dilated (before ending the latent
phase of labor).During the second stage of
labor, the power include both, the uterine
contractile forces and the voluntary maternal
expulsive efforts (pussing)
15
Evaluation of the passenger
- This includes
- - estimation of the expected fetal weight
- clinical evaluation of fetal lie, presentation,
position - If the estimated fetal weight is gt 4000 g the
incidence of dystocia, including shoulder
dystocia or fetopelvic disproportion is greater. - Cephalopelvic disproportion is a disparity
between the size or shape of the maternal pelvis
and the fetal head
16
If the fetal head is extended a larger cephalic
diameter (gt 32 cm) is presented to the pelvis,
therby increasing the possibility of dystociaA
brow presentation (forehead - the largest
cephalic diameter is 36 cm) (1/3000 deliveries)
typically converts to either a vertex or face
presentation, but if persistent, causes dystocia
requiring cesarean section.A face presentation
also requires cesarean section in most cases,
although a mentum anterior presentation (chin
toward mothers abdomen) sometimes may be
delivered vaginally.
17
Persistent occiput posterior positions are also
associated with longer labors (about 1 hour in
multiparous patients and 2 hours in nulliparous
patients)Fetal anomalies like hydrocephaly and
soft tissue tumors may also cause dystocia. The
use of prenatal ultrasound significantly reduces
the incidence of unexpected dystocia for these
reasons.
18
Evaluation of the passage
- Measurements of the bony pelvis are relatively
poor predictors of successful vaginal delivery.
It depends on the inaccuracy of these
measurements as well as case-by-case differences
in fetal accomodation and mechanisms of labor.
Only in rare cases, when the pelvis is
completely contracted (the pelvic diameters are
very small) manual evaluation of the diameters of
the pelvis can predict that the fetus will not
passage the birth canal.
19
In some cases the X-ray or computed tomographic
pelvimetry can be helpful, but the best test of
pelvic adeqacy is the progress or lack of
progress of descending of the fetal presenting
part in the birth canal.Except the bony pelvis,
there are soft tissues causes of dystocia, such
as -distended bladder or colon, -adnexal
mass-uterine fibroid
20
Management of abnormal labor
- Augmentation of labor is the stimulation of
uterine contractions that began spontaneously but
are either too infrequent or too weak, or both. - Induction of labor is the stimulation of uterine
contractions before the spontaneous onset of
labor, with the goal of achieving delivery.
21
Stimulation or induction of labor is usually
carried out with intravenous oxytocin (sometimes
prostaglandines) administrated by means of
metered pump.The incidence of prolongation of
the first stage of labor can be minimized by
avoiding unnecessary intervention, i.elabor
should not be induced when the cervix is not well
prepared or ripe (softened, anteriorly rotated,
partially effaced)
22
The Bishop score is used to quantify the degree
of cervical ripening and readiness for labor.
23
A score of 0 to 4 points is associated with the
highest likelihood of failed induction.A score
of 9 to 13 points is associated with the highest
likelihood of successful induction Induction of
labor is indicated if the anticipated benefits of
delivery exceed the risks of allowing the
pregnancy to continue
24
Indications
- Post-term pregnancy
- Maternal medical problems
- Pregnancy-induced hypertension
- Premature rupture of membranes
- Chorioamnionitis
25
Contraindications
- Placenta or vasa previa
- Cord presentation
- Abnormal/unstable fetal lie
- Prior two or more cesarean sections
- Prior classical uterine incision
- Prior uterine incision of unknown type
- Active genital herpes
26
When the cervix is unripe, Prostaglandin E2
(Prepidil, Propess) is administrated
intracervically or to the posterior fornix of the
vagina. In the majority of these cases labor
begins without the need of oxytocin stimulation.
27
A prolonged latent phase can be managed by
either rest or augmentation of labor with
intravenous oxytocin after excluding mechanical
factors.
28
If the patient is allowed to rest, one of
following will occur- the conractions can
stop, in which case the patient is not in labor
(false labor)- the contractions can become more
frequent and intensive, in which case the patient
will go into active labor- the contractions may
be as before, in which case oxytocine may be
administrated to augment the uterine contractions
29
The use of amniotomy (artificial rupture of
membranes) is also advocated with prolonged
latent phase. After amniotomy the fetal head
will provide a better dilating force than would
the intact bag of waters. Additionaly there may
be a release of prostaglandines, which could aid
in augmenting the force of contractions. The
risk of amniotomy is- an umbilical cord
prolapse (the presenting part should be firmly
applied to the cervix)- abruption of the
placenta- intrauterine infection
30
In the active phase of labor mechanical factors
such as abnormal position or presentation as well
as fetopelvic disproportion must be considered
before use of oxytocin. If the woman is tired
which results in secondary arrest of dilation,
rest followed by augmentation with oxytocin is
often effective. Artificial rupture of the
membranes is also recommended.
31
Risks of prolonged laborMaternal
Fetal
- asphyxia
- trauma
- infection
- cerebral damage
- infection
- maternal exhaustion
- lacerations
- uterine rupture
- uterine atony with possible hemorrhage
32
Prolonged labor is associated with the passage of
meconium into the amniotic fluid and subsequently
the risk of meconium aspiration syndrome (MAS).
Fetuses who inhale meconium-stained fluid
during labor may suffer this syndrom, which
includes both mechanical obstruction and chemical
pneumonitis from the meconium material.Pathologic
factors include- atelectasis- consolidation-
barotrauma- removal of pulmonary surfactant by
free fatty acids
33
Amniodilution is a method of intrapartum
treatment of meconium-stained amniotic fluid. A
normal saline solution is slowly infused through
a tube inserted in the uterus, washing
meconium-stained fluid out and replacing it with
the saline solution.As the fetal head is
delivered, but before delivery of the fetal
chest, suctioning of the nasopharynx should be
performed. After delivery of the fetus suctioning
out of meconium in the deeper parts of
respiratory tract (below the vocal cords) must be
done.
34
Techniques of operative delivery include-
obstetric forceps- vacuum extraction- cesarean
section
- The purpose of the forceps maneuver is to
- 1. augment the forces expelling the fetus when
the mothers voluntary efforts in conjunction
with uterine contractions are insufficient to
deliver the infant - and eventually to
- 2. rotate the fetal head in the birth canal, if
it isnt completely rotated
35
Necessary conditions to apply forceps
- Cervix Fully dilated
- Membranes Ruptured
- Position and station of fetal
head Known and engaged - Feto-pelvic
disproportion Excluded - Fetus Alive
36
Forceps Classification
- Outlet forceps - the fetal skull has reached the
perineal floor, the scalp is visable between
contractions, the sagittal suture is in the
anteposterior diameter - Low forceps - the leading point of fetal skull is
2 station or more - Midforceps - the head is engaged but the leading
point of the skull is above 2 station - High forceps - the head is high above inlet and
isnt engaged, the leading point of the skull
above 0 (not performed in current
obstetrics)
37
To avoid the potential risk of trauma to both
maternal and fetal parts application of obstetric
forceps should be performed by an experienced
clinician
38
Before application of the forceps the physician
should reassess the fetal position. The
neonatologist should be notified in advance,
before application of the forceps.Forceps
should be applied only after the cervix is
completely dilated and if there is no evidence of
cephalopelvic disproportion.Forceps sshould be
applied only (!!) after the biparietal diameter
has passed through the inlet, and the skull has
passed below the ischial spines.
39
After delivery the genital tract and infant
should be examined carefully.Potential risks-
lacerations of the cervix, vagina, perineum,
bladder and rectum- injuries of the fetus
intracranial hemorrhage, skull fracture, brachial
plexus injury, cephalhematoma, facial paralysis,
clavicular fracture
40
Vaccum extraction
- This maneuver is similar to forceps delivery.
- Its purpose is to augment the forces expelling
the fetus when the mothers voluntary efforts in
conjunction with uterine contractions are
insufficient to deliver the infant. - Advantages of the vacuum extractor include
- - less force applied to the fetal head
- - reduced anesthesia requirements
- - easier aplication
- - less perineal trauma
- the ability to permit the head to find its path
out - of the maternal pelvis
41
Disadvantages of the vacuum extractor include-
the application of traction only during
contractions- limitation of its use only to term
infant- prolonged delivery in comparison to
forceps deliveryThe head must be engaged and
the membranes must be ruptured. There is no
danger of catching vaginal mucosa or cervical
tissue between the vacuum and the fetal head.
Traction should be applied during the contraction
with the mother bearing down. A safety feature of
the vacuum cup is its inability to remain on the
fetal head during excess traction which may occur
during forceps delivery.
42
Cesarean section
- About 20-25 of gravidas are now delivered by
cesarean section. Appropximately two-thirds of
these procedures are perforemd after the onset of
labor.
43
In elective or not very emergency situations
such as - abnormal presentation- placenta
previa without bleeding- large fetus- abnormal
pelvis- some maternal diseases- prolonged
labor- begining of fetal depresiontransverse
abdominal incision in the lower part of abdomen,
just above the pubic bone, is performed (bikini
cut). In such situations there is sufficient time
to use regional anesthesia which allows the
mother to be awake without feeling pain (spinal
block or an epidural catheter).
44
In emergency situations such as- fetal
depresion- prolapsed umbilical cord- ruptured
uterus- severe abruptio placente- placenta
previa with extensive hemorrhagea midline
vertical abdominal incision (from the nevel to
the pubic bone) provides more rapid access to the
uterus. In such situations general anesthesia and
endotracheal intubation is the preferred
technique.