NEONATE BORN TO MOTHER WITH GRAVE - PowerPoint PPT Presentation
1 / 22
Title:
NEONATE BORN TO MOTHER WITH GRAVE
Description:
... Thyroid-stimulating immunoglobulins. Maternal antibodies wane over 2-3 months MATERNAL TBII TSH binding inhibiting immunoglobulin Levels 70% predictive ... – PowerPoint PPT presentation
Number of Views:52
Avg rating:3.0/5.0
Title: NEONATE BORN TO MOTHER WITH GRAVE
1
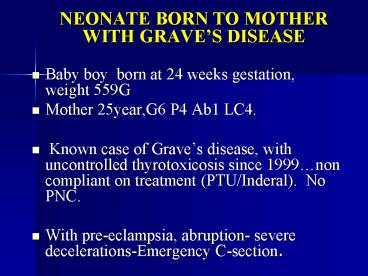
- NEONATE BORN TO MOTHER WITH GRAVES DISEASE
- Baby boy born at 24 weeks gestation, weight 559G
- Mother 25year,G6 P4 Ab1 LC4.
- Known case of Graves disease, with uncontrolled
thyrotoxicosis since 1999non compliant on
treatment (PTU/Inderal). No PNC. - With pre-eclampsia, abruption- severe
decelerations-Emergency C-section.
2
NICU COURSE
- Maternal TSI on Sept 2003 212
- (Normal 0 - 129)
- Resuscitated at birth Apgars 3,6 8.Ventilated
.given curosurf and transferred to ICN on
portable ventilator - On exam, baby 24 weeks gestation AGA
- Systemic exam WNL. No evidence of
goiter/exophthalmos. Initially had heart rates in
160-170 but later normalized.
3
MANAGEMENT IN NICU
- Hypoperfusion/hypotension/metabolic acidosis
needing NS bolus x 2 and inotrope support. - D2-3 echo showed PDAtreated with Indomethacin
- Head sonono IVH. Drug screen normal
4
THYROID CHEMISTRIES
Infant values Day -1 Day -7
T4,free (0.6-1.70) 1.26 0.45
TSH (0.4-5) 0.07 0.01
T3,total (70-204) 124 97
5
- PRESENT CONDITION
- Presently baby on IMV, being treated for evolving
lung diseasediuretics and steroid nebulization - On TPN and NG feeds.
6
OBSTETRIC HISTORY
- 7/96 40wks 9lbs NSVD Dallas
- 9/97 40wks 7lbs NSVD Mexico
- 11/01 31wks 2lbs NSVD Thomason
- 9/03 36wks 3lbs NSVD Thomason
- 12/00 15wks miscarriage
- 7/04 24wks 1.2lbs CS Thomason
7
BABY WITH NEONATALTHYROTOXICOSIS
- Baby No.3 was born at Thomason in 2001
- Preterm 31 wks SGA , BW1130 G
- No prenatal-care. Presented 1 hour prior to
delivery. - Had fetal bradycardia/abruptio.
- Ventilated
8
CLINICAL FEATURES/COURSE
- IUGR. Microcephaly, Bone age noted to be
advanced. - Had persistent tachycardia
- Baby had fluctuating levels of T4 and T3.
- Treated with Lugols iodine, Inderal and PTU
9
THYROID CHEMISTRY
2001 Day 1 Day 10 Day 14
T4 0.7 gt6 2.6
TSH lt 0.1 lt0.1 lt0.1
T3 264 570 81
10
COURSE AFTER DISCHARGE
- Discharged at 2 m with T4 0.6 and T3 69.
Stopped meds prior to discharge. - Had initially weight loss which later improved.
- At 2 m age had seizures. F/Up thyroid tests were
normal. - Head scan/MRI July 2004 showed non communicating
hydrocephalus
11
THYROTOXICOSIS IN NEONATE
- Typically a transient hyperthyroidism
- 1 in 70 Graves affected pregnancies.
- Mortality up to 25
- Etiology
- Placental transfer Thyroid-stimulating
immunoglobulins. Maternal antibodies wane over
2-3 months
12
MATERNAL TBII
- TSH binding inhibiting immunoglobulin
- Levels gt 70 predictive neonatal
thyrotoxicosis - Role of stimulatory and inhibitory
immunoglobulins - Duration of disease depends on concentration,
degradation rate and presence or absence of
inhibitory Ab
13
(No Transcript)
14
BABIES AT RISK
- Raised level of TBII in pregnancy
- TBII not assessed
- Thyotoxicosis in 3rd trimester
- Thionamide required in 3rd trimester
- Family H/O TSH receptor mutation
- Evidence of fetal thyrotoxicosis
15
POINTS TO CONSIDER
- Mother with Graves disease may not have
thyrotoxicosis and may be euthyroid or
hypothyroid. - Exposure to anti-thyroid drugs in-utero may delay
symptoms - Newborn Screening with T4-radioimmune assay, can
detect raised levels of T4 - Positive assay for Thyroid stimulating
immunoglobulins.confirmatory - Consider narcotic withdrawal
16
CLINICAL FEATURES OF NEONATAL THYROTOXICOSIS
- Hyperirritability
- Tachycardia
- Goiter
- Exophthalmos
- LBW and weight loss
- CHF
- Craniosynostosis/ advanced bone
age/microcephalypsychomotor retardation - Jaundice/thrombocytopenia
17
APPROACH TO BABY OF MOTHER WITH GRAVES DISEASE
18
- TREATMENT
- Should biochemical abnormality in absence of
symptoms be treated? - Thionamides block hormone synthesis
- PTU 5-10mg/kg/d in 3 divided doses
- Carbimazole 0.5-1.5mg/kg/d
- Lugols iodine (8mg/drop) 1-3 drops/D
- Iopanoic acid/sodium ipodate, Propanolol,
Prednisolonein refractory cases
19
TREATMENT (CONTINUED)
- Exchange transfusionsto reduce TSI levels
- Baby on treatment for thyrotoxicosis is reviewed
weekly until stable, then every 2 weeks and drug
dose reduced. - Usually treated for 4-8 weeks.
- Thyrotoxicosis secondary to mutations of TSH
receptor require ablative treatment with surgery.
20
SUMMARY
- Possibility of fetal thyrotoxicosis must be kept
in all mothers with a history of Graves disease
regardless of thyroid status/treatment. - Thyroid stimulating immunoglobulins (TSI)
persist even after thyroid surgery/radioablation
in mother. - Neonatal thyrotoxicosis secondary to TSIs is a
transient disorder, limited by clearance of
maternal antibodies
21
SUMMARY (CONTINUED)
- In neonates signs of thyrotoxicosis may be
delayed due to effect of maternal anti-thyroid
drugs or effect of blocking antibodies. Cases
reported as late as 45 days. - TSH binding inhibitor Ig levels from mother and
from neonate correlate well with neonatal
thyrotoxicosis.
22
(No Transcript)