Communication PowerPoint PPT Presentation
Title: Communication
1
Case Study
Step 3 Develop From Established Principles
- Having established that both Higher Education,
Clinical and Professional Practice were now on
the same side, the initial issues of concern
were quickly resolved - Is this OK ? This is OK because it follows
the current guidelines, published by - How deep should the student go ?
- The first year student requires a solid
understanding of the basic concepts of upon
which, their future practice can be developed.
You can determine this by - Theory Practice cest quoi ?
- My experience and opinion is valuable, but I
need to measure and account for it. Information
that supports me might be found at - H.E. I dont understand
- In fact many of the basic principles are
comparable to professional practice. Once you
see past the jargon, then you can work-out the
bells whistles for yourself It helps to
have some help with the paperwork though. - Final consensus concluded that the paperwork
was not in fact, the main concern rather,
demonstrating the underlying principle.
(Students) and staff were subsequently able to
achieve this by mutually accessing auditable
evidence and independently validating their
rationales for practice and theory. - Feedback and Communication
- (Single Placement Case-Study Only 12.04.07)
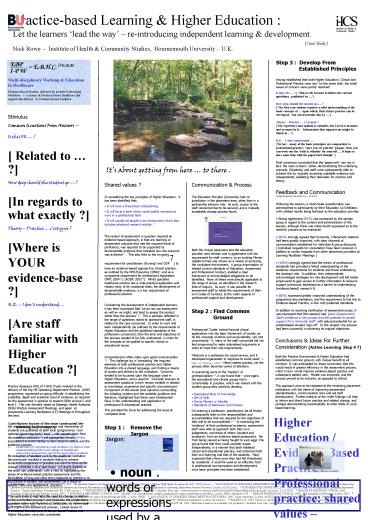
Stimulus Common Questions From Assessors Is
this OK ? Related to ? How deep should
the student go ? In regards to what exactly
? Theory Practice cest quoi ? Where is
YOUR evidence-base ? H.E. I dont understand
Are staff familiar with Higher Education
? Practice Assessors (PA) of 3 NHS Trusts
involved in the delivery of the Dip HE Operating
Department Practice (ODP) programme, expressed
on-going difficulty in establishing the
suitability, depth and academic level of
evidence, as required for the assessment in
practice of student ODPs at level C and level I.
This was formally raised at Strategic Health
Authority (SHA) Practice Assessment Meetings, and
again at programme Learning Facilitators (LF)
Meetings of throughout the year. Set
requirements for the assessment and mentorship of
students are published at both local (programme)
1 and national (governing body) level 2, with
support given from the academic institution 3,
yet approaches remain inconsistent and
detrimental to both student welfare and the
academic process. Re-evaluation of student
work by the academic institution has previously
resulted in students failing to achieve evidenced
competency in practice and was the stimulus for
change, reflected in this case-study. An urgent
address of the issue was undertaken, with a view
to highlighting the issues of evidence-based
practice assessment and the formulation of long
and short term measures to prevent a
re-occurrence of student non-achievement (as a
result of failures within the assessment
process). This work looks to highlight the need
for change in relation to the events that
occurred, and illustrates the collaborative
approach taken with Partnership Institutions, to
inform staff and improve the assessment process.
Linked issues of Professional Development,
Evidence-Based Practice and Higher Education were
also considered. Approach Methodology
Design Retrospective linked questioning helped
to establish the locality, process and
involvement of the problem, relative to its
initiating incident. Analysis of current core
documentation relating to the Nursing and ODP
professions was undertaken to establish the
professional and working requirements of each
group. Topical academic consultation was sought,
in conjunction with healthcare providers. The
search strategy for information was conducted by
accessing a variety of databases (BNI, Blackwell
Synergy, CINAHL, MEDLINE) in relation to Nursing
and Allied Health Professions. This was widened
to include the British Education Index, and
supplemented by manual meta-search engine
employment (Ixquick). Key words relating to the
identified issues were entered. Results were
filtered and appropriate results accessed and
reviewed. Manual review of institutional
resources and personal texts was also employed.
Non-statistical review of Likert Questionnaire
provided feedback for the single placement study
(500 bed District General Hospital) and
indication for future development.
bromine.servlet.net/.../ninarios/STEPPING.jpg
Its about getting from here to there .
Communication Process The Education Provider
(University) had no jurisdiction in the placement
area, other than in a partnership advisory role.
As such, access to the staff concerned had to be
secured, and a mutually acceptable change process
found. Both the clinical placement and the
education provider were familiar and in agreement
with the requirement for staff currency, so an
existing Mentor Update format was chosen as a
means of accessing the workplace environment. A
group examination of related current standards of
Education, Assessment and Professional Conduct,
enabled a clear framework of acknowledged
obligations to be identified. Many of these were
directly applicable to the range of issues, as
identified in the research lines of enquiry. As
such, it was possible for assessment staff to
relate the requirements of their own Codes of
Conduct, to the wider aspects of professional
support and development.
- Shared values ?
- In considering the key principles of Higher
Education, it has been identified that - It will have a theoretical underpinning,
- It will be at a level which would qualify
someone to work in a professional field - It will usually be taught in an environment
which also includes advanced research activity. 4 - The system of assessment in question required an
evidence-based approach, in that any learning or
assessment outcome that met the required levels
of proficiency, was required to be supported by
demonstrable evidence that indicated how the
outcome was achieved 5 . This also links to the
on-going requirement for practitioners (Nursing6
and ODP7) to have an evidence-based approach to
clinical practice, as outlined by the NHS
Executive (1996)8, and as a component requirement
for professional registration (NMC 2004 6),
(AODP, 2003 9). Whilst specialist healthcare
practice has a wide practical application and
retains many of its vocational traits, the
development of demonstrable evidence, is a key
requirement of professional practice. - Considering the development of independent
learners, it has been expressed that we do not
use assessment as well as we might, and tend to
assess the product rather than the process 10.
This is perhaps reflected in the range of
questions raised by assessment staff, in relation
to the case concerned. In order to work and
learn independently (as outlined by the
requirements of Higher Education and the
published standards of the professions
concerned), then the aims and objectives of the
process needed to be fully understood, in order
for the concepts to be applied to specific
clinical or educational issues. - Comprehension often relies upon good
communication 11. The challenge lay in
translating the required elements of both
professional practice and Higher Education into a
shared language, and finding a means of access
and delivery to the workplace. Concerns tended
to be focussed upon the language used in Higher
Education, and a need for concrete answers to
assessment questions (which remain variable in
relation to knowledge, experience and specific
circumstances). Comparison of the events (and
opinions) surrounding the initiating incident and
the available guidance and literature,
highlighted that there were fundamental flaws in
the understanding and application of professional
educational practice. - This provided the focus for addressing the issue
at workplace level. - Step 1 Remove the Jargon
- Step 2 Find Common Ground
- Professional Codes extend beyond clinical
applications into the basic framework of society,
as do the concepts of ethics and accountability,
yet (not uncommonly 12), many of the staff
concerned did not feel empowered to make
rationalised arguments in order to meet their
role requirements. - Medicine is a profession for social service, and
it developed organisation in response to social
need. (C. Mayo U.S. Physician 1931) Need
creates process, yet the process often becomes
centre of attention. - In examining some of the markers of
professionalism 14, it was found that once
again, the educational and clinical groups had a
commonality in purpose, which was shared with the
student group they aimed to develop. - Specialized Body of Knowledge
- Set of Skills
- Group Mission or Identity
- Standards of Behaviour and Practice
- On entering a profession, practitioners (at all
levels) subsequently take-on the responsibilities
and accountabilities that are required for the
objectives of that role to be accomplished 6,7.
In examining the evidence of their professional
existence, assessment staff were able to approach
both their own judgements, and those of others
(student and employer), from an evidence-based
perspective. Far from being viewed as being
taught to suck eggs, the group found that they
could consider issues independently, in a manner
that both validated clinical and educational
practice, and enhanced both their own learning
and that of the students. Many expressed that
where once they had felt threatened by
academia, it could be used as an effective
tool in professional communication and
development, once basic principles had been
established.
Conclusions Ideas For Further Consideration
(Active Learning Step 4 ?) Both the Practice
Environment Higher Education had established
common ground, with mutual benefit to all
involved. It was anticipated by those concerned,
that this would result in greater efficiency in
the assessment process, which in-turn would
improve evidence-based practice and subsequent
patient care. Morale was improved, and the
process proved to be inclusive, as opposed to
critical. This approach aims to be repeated at
the remaining placement institutions with the
intent of improving assessment standardisation,
communication links and aid staff development.
Further analysis of the wider findings will help
to inform and direct future practice and related
change, and perhaps demonstrating transferability
to other fields of work-based learning.
Higher Education / Evidence-Based Practice /
Professional practice shared values common
goals. If we fail to engage others, we
remain separated from the wider (healthcare)
community . Invite people on-board (but
preferably in a language they understand).
- Contributory factors of the issue constructed the
following lines of enquiry - Scope of application within professional body
publications What are the requirements
concerning practice assessment, and are they
being met ? - Definitions of competency and evidence Is there
a clear understanding of the basic pillars of
healthcare placement assessment, and of the
associated academic clinical descriptors
currently employed ? - Is the requirement for evidence-based practice
evenly applicable to pre and post registration
development, and how does it relate to assessment
practice ?
V. Volny, Vermilion Sea Institute.
References 1 BOURNEMOUTH UNIVERSITY, 2006.
The Essential Guide to Pre-Registration Operating
Department Practice - Clinical Staff Guide.
Bournemouth BU / ODP, version 3. 2 ASSOCIATION
OF OPERATING DEPARTMENT PRACTITIONERS, 2006.
Qualifications Framework for Mentors Supporting
Learners in Practice Standards and Guidance for
Mentors and Practice Placements in Support of
Pre-registration Diploma of Higher Education in
Operating Department Practice Provision. London
AODP, Issue 2. 3 BOURNEMOUTH UNIVERSITY, 2006.
The Essential Guide to Pre-Registration Operating
Department Practice - Clinical Staff Guide.
Bournemouth BU / ODP, version 3. 4
UNIVERSITIES SCOTLAND, 2004. What is Higher
Education ? Available from http /
www.universities-scotland.ac.uk/Facts20and20Figu
res/HigherEducation.pdf Accessed 01.05.2007.
5 HEALTH PROFESSIONS COUNCIL, 2005.
Standards of Education and Training. London HPC.
6 NURSING MIDWIFERY COUNCIL, 2004. The NMC
code of professional conduct standards for
conduct, performance and ethics. London NMC,
Standards.07.04. 7 HEALTH PROFESSIONS COUNCIL,
2004. ODP Standards of Proficiency. London HPC.
8 NHS EXECUTIVE, 1996. Promoting Clinical
Effectiveness A framework for action in and
through the NHS. London NHSE. 9
ASSOCIATION OF OPERATING DEPARTMENT
PRACTITIONERS, 2003. Scope of practice. London
AODP, Issue 1 Revised 2004. 10 Hoskins, S.
2004. Developing Independent Learners.
Available from http / www.business.heacademy.ac.
uk/resources/landt/learning/independant Accessed
01.05.2007. 11 GOLEMAN, D. 1996.
Emotional Intelligence. London Bloomsbury. 12
PARAHOO, K., 2000. Barriers to, and facilitators
of, research utilization among nurses in Northern
Ireland. Journal of Advanced Nursing 31(1),
89-98. 13 MAYO, CH, 1931. Collected papers
of the Mayo Clinic and Mayo Foundation, 231020.
Rochester, MN 14 PLAUT, M. 2006. What does
it mean to be a member of a profession ?
Available from http / www.medschool.umaryland.ed
u/Professionalism/professionalism_dmrt.pdf
Accessed 01.05.2007.