Existing Restoration - Clinical Status PowerPoint PPT Presentation
1 / 44
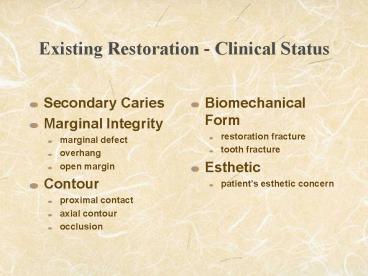
Title: Existing Restoration - Clinical Status
1
Existing Restoration - Clinical Status
- Secondary Caries
- Marginal Integrity
- marginal defect
- overhang
- open margin
- Contour
- proximal contact
- axial contour
- occlusion
- Biomechanical Form
- restoration fracture
- tooth fracture
- Esthetic
- patients esthetic concern
2
Marginal Defect - Amalgam Restoration
It is the second most common reasons given for
replacing an amaglam restoration
3
Reasons for replacing an existing restoration
with defective margin- Survey of 124 dentists
- It is a plaque trap, thus increasing the chance
of developing secondary caries (37) - More likely to find secondary caries on the
cavity wall below the defect (25)
Tooth
Amalgam
4
Reasons for replacing an existing restoration
with defective margin
- It is a plaque trap, thus increasing the chance
of developing secondary caries. - Is this hypothesis supported by scientific facts?
Tooth
Amalgam
5
Reasons for replacing an amalgam restoration with
defective margin
Are there direct scientific data showing a
relationship between marginal defect and the
development of secondary caries?
NO
6
Indirect/Empirical Evidence
- We are seeing the majority of the disease in a
small population of our patients therefore not
everybody is equally susceptible to the disease. - If physical barrier for oral hygiene is a
problem, why do some pits and fissures never
develop into lesions. - Assuming these defects on the margin of an aging
restoration has been there for years why no
lesion has been developed in all these years.
7
Reasons for replacing an existing restoration
with defective margin- Survey of 124 dentists
More likely to find secondary caries on the
cavity wall below the defect Is this
hypothesis supported by scientific facts?
Tooth
Amalgam
8
Reasons for replacing a restoration with
defective margin
- There is scientific evidence showing that there
is NO relationship between marginal defect and
the presence of secondary caries on the cavity
wall below the defect
9
30 extracted teeth with occlusal amalgam
restorations were sectioned. Caries were
identified by imbibing the section in with
quinoline and examined in polarized light
10
How should we make the decision on when to
replace??
- Replacement decision should not be based on the
quality of the margin ALONE - Instead
- Replacement decision should be based on risks
and/or the presence of pathology
11
Replacement Decisions
- Risk Factors
- Risk factors related to dental caries and
periodontal diseases. - Presence of pulpal pathology (e.g. sensitivity to
temperature change, sweet). - Patients complaint (esthetic concern).
12
Contour
- Status
- Proximal contact - open, rough, location
- Axial contour - over/undercontour, location
- Occlusion
- Diagnosis is based on visual, patients chief
complain and radiographs
13
No Proximal Contact - Treatment Decision
- No treatment indicated if it is physiologic (e.g.
natural spacing between teeth) - Replace if patient has esthetic concern or
complain about food impaction, and/or in the
presence of periodontal diseases. - Grey area
- Complaining about food impaction between 2 teeth
that have no existing restoration, no evidence of
periodontal diseases. - Complaining about food impaction - occlusal
contact OK, but gingival embrasure area open
because of gingival recession.
14
No Proximal Contact - Treatment Options
- Anteriors
- Direct composite, indirect porcelain veneers,
full veneer crowns. - Choices depend on patients expectation/ability
to pay and other clinical concerns (e.g. shade
match problem, discolored tooth) and dentist
skill. - Posteriors
- Direct restoration - know the clinical and
mechanical limitations of the restorative
materials direct composite restorative may be
contra-indicated deep gingival seat - clinical
limitation. - Indirect restoration - may be the only viable
option.
15
ContourReplacement Decision
- Rough Proximal Contact
- Smooth or replace only if patient complain about
not being able to floss - Proximal Contact at Non-physiologic Location
- Use the same criteria as no proximal contact (no
treatment indicated in the absence of pathology,
patients complain and esthetic concern)
16
ContourReplacement Decision and Options
- Axial contour
- Undercontour - e.g. porcelain fracture from PFM
crown - Overcontour - e.g. buccal or lingual axial
surfaces overcontour - Recontour or replace if patient has esthetic or
functional concern presence of periodontal
pathology
17
ContourReplacement Decision and Options
- Occlusion
- Dx usually based on patients complain
- Hyper-occlusion/interference - adjust
- Hypo-occlusion - replace
18
Biomechanical Form
- Status
- Tooth with bulk fracture or fracture line
- Restoration with bulk fracture or fracture line
- Diagnosis
- Visual, patients complain, differential loading
19
Differential loading using tooth slooth
20
Tooth Fracture - AnteriorTreatment Options
- Based on the size of the fracture
- Small - recontour, direct composite
- Moderate - direct composite, composite/porcelain
veneers full crown (PFM, all porcelain) - Large - direct composite, composite/porcelain
veneers, full crown, RCT/core buildup/crown
21
Tooth Fracture - AnteriorSmall -Treatment Options
- Recontour or monitor - should be given as an
option when the fracture is minor and only limit
to the incisal edge area - Reason
- The most common reason for patient fracturing the
incisal edge (minor) is excessive bruxism. These
patients usually grind the incisal edge of their
Mx anteriors to thin edges and eventually part of
the enamel will fracture off. The prognosis of
restoring these fractures with composite is at
best questionable (due to the limitation of the
mechanical properties of the material). If you
are going restore these lesion, you need to
inform patient that the restoration is for
cosmetic purpose only.
22
Tooth Fracture - AnteriorModerate -Treatment
Options
- Direct composite - Disadvantages questionable
prognosis due to the possibility of fracture
esthetic result? Advantages cost, conservation
of tooth structure - Full crown - Disadvantages cost, not
conservative Advantages good prognosis good
esthetic result - Composite veneers - Disadvantages cost no
advantage over direct composite - Porcelain veneers - Disadvantages cost
Advantages good prognosis, conservation of tooth
structure good esthetic result
23
Tooth Fracture - AnteriorLarge -Treatment Options
- Direct composite Advantages cost, conservation
of tooth structure Disadvantages very
questionable prognosis - Full crown may not be an option due to
inadequate retention and resistance form - Composite/Porcelain veneers may be your best
option without involving RCT - RCT/core buildup/crown may be your best option
depending on the amount of tooth structure left
Disadvantages cost
24
Tooth Fracture - AnteriorLarge -Treatment Options
Remaining tooth structure following crown prep.
- Why a full crown may not be an option for
restoring a large anterior fracture? - Inadequate retention and resistance
Fractured Area
25
Tooth Fracture - PosteriorTreatment Options
- Indirect restoration is the most common
restorative options for restoring fractured
posterior teeth. - Different material/procedures are available each
with their own characteristic, advantages and
disadvantages partial veneer restorations (gold,
composite, porcelain, CAD/CAM) full veneer
restorations (gold, PFM, all porcelain). - Choice should be based on patients preference
(esthetic) dentist clinical judgment on what is
the best restoration in a specific clinical
situation.
26
Tooth Fracture - PosteriorTreatment Options
- Repair - should no be overlooked as an option
e.g. Patient presents with fractured DL cusp on
tooth 14, which already has an extensive amalgam
covering all the cusps except DL cusp. Patient
cannot afford to have a crown.
27
Tooth Fracture - PosteriorTreatment Options
- Direct restoration - when indirect restoration is
not an option for financial reason. Material of
choice (amalgam vs composite) should be based on - Patients preferences (cost, esthetic)
- Conservation of tooth structure
- Clinical expertise of the dentist to manipulate
the material in a specific clinical situation - Clinical properties of the material that will
allow the dentist to restore the tooth to a more
ideal form e.g. amalgam will have an advantage
over composite to establish proximal contact
28
Basic Principles in Determining What
Material/Procedure To Use
- The basic principle should be centered around -
What is the most conservative way to restore the
tooth to its original (or as close to)
biomechanical form. - Some material needs bulk to resist fracture (e.g.
amalgam, porcelain) - concern when dealing with a
tooth with short clinical crown length. - Mode of retention - mechanical vs bonding
mechanical retention need more tooth reduction -
concern when dealing with a tooth with extensive
structural damage. - Bonding to sclerotic/secondary dentin is somewhat
unpredictable - Rely on bonding to provide resistance form
(prevent fracture of tooth structure) is somewhat
unpredictable - Isolation (for bonding) may be a concern for
certain patient and in the more posterior part of
the mouth
29
Other Considerations in Restoring a Fractured
Tooth
- A fractured tooth or a tooth with a large
existing restoration may need a foundation
restoration before a crown can be fabricated. - The need for a foundation restoration will depend
on the depth of the pulpal floor of the existing
restoration, and to a lesser extent the
buccal-lingual width of the existing restoration. - Retention of the crown will depend on the amount
of tooth structure left around the pulpal area.
30
What is your treatment recommendation?
Mn first molar with an existing Class I amalgam
restoration (pulpal depth of 2 mm). Fractured ML
cusp from mid MMR to Li groove area at the level
of the pulpal floor.
31
Incomplete Tooth Fracture (fracture line) -
Treatment decision and Options
- Diagnosis
- patients complain
- Sensitivity on function
- Treatment Options
- Direct bonded restoration
- Indirect bonded restoration
- Full veneer crown
32
Incomplete Tooth FractureCase Report 1
- 1995
- cc LR occasional sensitivity to chewing
- 2002
- cc the sensitivity is getting worst
- Dx - incomplete fracture on 30
- Tx - 30 full gold crown
33
Incomplete Tooth FractureCase Report 1
- 2003
- cc no improvement, still sensitive to chewing
- Dx - evidence of fracture line on DMR of 31
- Tx - DO composite
- 2004
- Buccal fistula, gutta percha used to trace the
lesion to the apex of the D root
34
Incomplete Tooth FractureCase Report 1
- 31 extraction
- Final diagnosis - 31 DMR fracture line extended
down onto the D root - Prognosis - unrestorable
- Complete relieve of symptom following the
extraction
35
Incomplete Tooth FractureCase Report 2
- Undiagnosed fractured of the DMR extending to the
apex of the D root (18) - 19 (has an extensive MOD amalgam restoration) -
was crowned along the way
36
Incomplete Tooth FractureCase Report 3
- cc pain on chewing
- Dx - incomplete tooth fracture on MMR and DMR
37
Incomplete Tooth FractureCase Report 3
- Fracture line extended onto the pulpal floor.
- Tx - porcelain inlay using CAD/CAM technology
- Today - symptom is gone
38
Incomplete Tooth FractureCase Report 4
- 41-yo male with cc low grade TA on LR
- No pathology found except 5 mm pocket on M of
31. Patient is a bruxer with heavy wear facets
on all teeth. Prophy was done - Report to the clinic the very next day
complaining the pain is becoming more intense
pain relieved by drinking cold water - Re-probe 31 and getting probing depth of at
least 8 mm - Careful exam reviewed a fracture line on MMR
- Dx Tooth fracture to apex of M root confirmed
by endodontist. Tooth was extracted
39
Restoration Fracture/Incomplete
FractureTreatment decisions and Options
- Treatment decisions and options similar to tooth
fracture - Try to identify the reason(s) for the fracture
- Inadequate bulk - most common reason for amalgam
restoration need to correct the preparation if
amalgam is used again - Exceeding the physical properties of the material
- should consider alternative procedure/material
40
Replacement Decisions
- Start out with the least invasive option always
ask yourself the question will the proposed
option improve the health of the tissue/oral
health? - Will the new restoration improve
function/esthetics? - Will the new restoration addresses the chief
complaint of the patient? - Will the new restoration prevent further
destruction of the surrounding hard/soft tissue
41
Decision to repair/replace a cast gold
restoration with a perforation on the occlusal
surface
What rationale can you give to repair/replace a
cast gold restoration with a perforation on the
occlusal surface? (Assuming there is no complaint
from patient and you cannot find a cement line)
42
Esthetic
- Status
- Poor color match
- Poor contour
- Diagnosis
- Should be based on patients complain
43
EstheticReplacement Decision
- Listen to patients REAL concern, try to
understand EXACTLY what they want and expect - Choose a procedure(s) that has the potential of
matching patients expectation (end result vs
patients ability to pay), and satisfy our
criteria of conservation and optimal oral health
following the procedure - Important to understand the limitations of each
of the esthetic procedure match patients
concern with the limitations of the procedure in
mind
44
EstheticTreatment Options
- Recontour - least invasive, limited to minor
alternation - Bleaching - non-invasive unpredictable result
relatively inexpensive - Composite Veneer - limited ability to mask dark
stain longevity technically more challenging - Porcelain Veneer - more invasive, limited ability
to mast dark stain more expensive better
esthetic - Porcelain fused to metal crown - invasive, metal
collar - All Porcelain crown - most invasive most
expensive best color