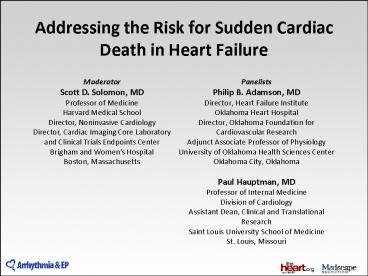
Addressing the Risk for Sudden Cardiac Death in Heart Failure
Title:
Addressing the Risk for Sudden Cardiac Death in Heart Failure
Description:
Addressing the Risk for Sudden Cardiac Death in Heart Failure Panelists Philip B. Adamson, MD Director, Heart Failure Institute Oklahoma Heart Hospital –
Number of Views:148
Avg rating:3.0/5.0
Title: Addressing the Risk for Sudden Cardiac Death in Heart Failure
1
Addressing the Risk for Sudden Cardiac Death in
Heart Failure
- Panelists
- Philip B. Adamson, MD
- Director, Heart Failure Institute
- Oklahoma Heart Hospital
- Director, Oklahoma Foundation for Cardiovascular
Research - Adjunct Associate Professor of Physiology
- University of Oklahoma Health Sciences Center
- Oklahoma City, Oklahoma
- Paul Hauptman, MD
- Professor of Internal Medicine
- Division of Cardiology
- Assistant Dean, Clinical and Translational
Research - Saint Louis University School of Medicine
- St. Louis, Missouri
Moderator Scott D. Solomon, MD Professor of
Medicine Harvard Medical School Director,
Noninvasive Cardiology Director, Cardiac Imaging
Core Laboratory and Clinical Trials Endpoints
Center Brigham and Womens Hospital Boston,
Massachusetts
2
Learning Objectives
- Identify persistent treatment gaps for people
with HF - Evaluate potential mechanisms underlying the risk
for SCD and HF - Assess the role of ICDs and WCDs to address the
risk of SCD in patients with ischemic and
nonischemic HF
3
Who Is at Risk of SCD?
- Patients with low EF
- Family history
- Risk stratification can help delineate high,
moderate, and low risk - Patients with preserved left ventricular function
may have lower risk of SCD but still have high
mortality risk - Hypokalemia and metabolic abnormalities
- Symptomatology often has inverse relation to SCD
4
VALIANT Patients With a First or Subsequent
Acute MI Complicated by HF, Left Ventricular
Systolic Dysfunction, or Both
- n 14,609
- 1067 had an event (median, 180 days after MI)
- 903 died suddenly
- 164 were resuscitated after cardiac arrest
- The risk was highest in the first 30 days after
MI
Solomon SD, et al.1
5
Causes of Sudden Death in HF
- Lethal arrhythmias
- Cerebrovascular accidents
- Pulmonary embolism
- Myocardial rupture
- Aneurysms
6
Breakdown of Sudden Unexpected Death by Autopsy
Results in VALIANT
N 105
Other CV death 2
Non-CV death 3
Pump failure 4
Myocardial ruptures 12
Presumed arrhythmic death (n 52) 49
Myocardial infarction 30
- 3 of index MI
- 27 of recurrent MI
Pouleur AC, et al.2
7
Cause of Death
Type of Death DINAMIT (n 342)
Sudden, presumed arrhythmic 29 (54)
Cardiac, non-arrhythmic 17 (31)
Noncardiac 8 (15)
Total 54 (16)
Dorian D, et al.3
8
Implications of ß-Blocker Use Prior to Device
Implantation
- ß-Blockers decrease risk of SCD
- This is relevant to time prior to and after
device implant - ß-Blockers may increase ejection fraction
- Patient may no longer be a candidate for primary
prevention according to the guidelines - Underuse of ß-Blockers may reflect poor
adherence, a key factor in the successful
application of device therapy
9
Types of Arrhythmias
- 2 to 5 are probably unrecoverable
- 85 to 90 are tachyarrhythmias
- Electromechanical disassociation PEA-type
- Sustained bradyarrhythmias account for maybe 10
10
CMS, the National Coverage Determination
- Waiting period before ICD implantation in
patients with cardiomyopathy is 9 months after
first diagnosis of nonischemic cardiomyopathy - However, there are 2 types of patients who
present de novo - Those who have truly de novo cardiomyopathy and
HF - Those who have established cardiomyopathy but a
de novo presentation of HF
11
Decision-Making Process for the Patient at Risk
for SCD
- ACC/AHA guidelines
- ACC appropriateness paper across 369 different
indications - CMS, national coverage determination
- Clinical judgment
- Patient preference
- Risk management
Centers for Medicare and Medicaid
Services.9 Russo AM, et al.10 Zipes DP, et
al.11
12
HAT- Home Use of Automated ExternalDefibrillators
for Sudden Cardiac Arrest
- Overall, 450 patients died
- 228 of 3506 patients (6.5) in the control group
- 222 of 3495 patients (6.4) in the AED group
- 160 deaths (35.6) were considered to be sudden
cardiac arrest from tachyarrhythmia - 117 occurred at home
- 58 at-home events were witnessed
- AEDs were used in 32 patients
- 14 received an appropriate shock
- 4 survived to hospital discharge
Bardy GH, et al.12
13
Length of Time Patients Wore the WCD
Chung MK, et al.14
14
Thank you for participatingin this
activity. To proceed to the CME/CE posttest,
click the Earn CME Credit link on this page.