PSORIASIS ETIOPATOGENESIS AND PHARMACOTHERAPY PowerPoint PPT Presentation
1 / 47
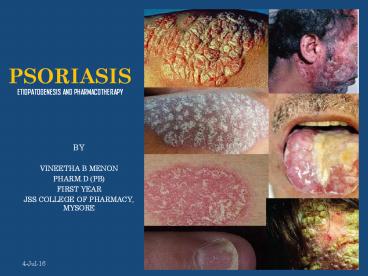
Title: PSORIASIS ETIOPATOGENESIS AND PHARMACOTHERAPY
1
PSORIASIS ETIOPATOGENESIS AND PHARMACOTHERAPY
- BY
- VINEETHA B MENON
- PHARM.D (PB)
- FIRST YEAR
- JSS COLLEGE OF PHARMACY, MYSORE
2
CONTENTS
- INTRODUCTION
- EPIDEMIOLOGY
- AETIOLOGY
- PATHOGENESIS
- DIAGNOSIS
- CLINICAL FEATURES
- TREATMENT
3
INTRODUCTION
- Psoriasis is a chronic inflammatory condition
that may affect the skin and joints
4
- EPIDEMIOLOGY
5
EPIDEMIOLOGY
- Psoriasis affects both sexes equally
- Can occur at any age, although it most commonly
appears for the first time between the ages of 15
and 25 years
6
- AETIOLOGY
7
AETIOLOGY
- Genetic predisposition DR7 CW6
- Non-hereditary factors
- Infection
- Koebner phenomenon
- Lithium, chloroquine, ß-blockers
- Stress
- Smoking Alcohol
8
- PATHOGENESIS
9
PATHOGENESIS
- Many changes occur in the skin
- Epidermis Acanthosis, Parakeratosis
- Dermis capillaries are dilated, twisted, closer
to the surface of the skin
10
- Large number of inflammatory cells are present in
all layers of the skin- granulocytes are
predominant and form micro-abscessess in the
epidermis - Langerhan cells and lymphocytes are also
increased - Main abnormality is the increased epidermal cell
turn over
11
Two hypothesis
- Hyperproliferation may be due to immunological
response. Cytokines released by lymphocytes and
langerhan cells may further stimulate the
inflammatory cells which cause epidermal cell
turn over at an increased rate
12
- 2. Epithelial cells themselves produce cytokines
which promote proliferation of epithelial cells
and attract lymphocytes
13
- DIAGNOSIS
14
DIAGNOSIS
- A diagnosis of psoriasis is usually based on the
appearance of the skin - There are no special blood tests or diagnostic
procedures - Skin biopsy, may be needed to rule out other
disorders and to confirm the diagnosis - Skin from a biopsy will show clubbed rete
pegs, if positive for psoriasis - Another sign of psoriasis is that when the
plaques are scraped, one can see pinpoint
bleeding from the skin below
15
- Rete pegs are the epithelial extensions that
project into the underlying connective tissue
16
- CLINICAL FEATURES
17
CLINICAL FEATURES
- Typical psoriatic lesion
- is red, scaly, sharply
- demarcated plaque
18
- It can be on any
- size and can affect
- any part of the
- body
19
- The scales are silvery and easily scraped off
revealing tiny bleed points - Psoriasis is not typically itchy, but it can
cause itching when severely inflammed and rapidly
spreading to the palms and soles
20
- Different patterns of psoriasis are
- Guttate psoriasis
- Chronic plaque psoriasis
- Psoriasis of scalp
- Psoriasis of nails
- Psoriasis of palms and soles
- Flexural psoriasis
- Erythrodermic and generalized pustular psoriasis
- Psoriatic arthropathy
21
GUTTATE PSORIASIS
- Multiple small plaques are seen all over the body
- Mainly seen in children after streptococcal sore
throat - Self limiting after a few weeks
22
CHRONIC PLAQUE PSORIASIS
- Medium and large plaques occur on the limb and
trunk - Very persistent
23
PSORIASIS OF THE SCALP
- May occur as demarcated plaques or may involve
the entire scalp extending to the hairline - Scales are white, thick and chalky
- Hair loss will occur if the scalp is thickly
scaled - Recover if the scales are cleared and kept under
control
24
PSORIASIS OF THE NAILS
- Pitting, onycholysis and hyperkeratosis under the
nail - Very resistant
25
PSORIASIS OF THE PALMS AN SOLES
- Sharp demarcation of the involved areas
- Affected areas are inflammed and scaly and may
contain sterile pustules of large pin head size.
These pustules dry up and form brown macules - Affected skin becomes hyperatotic and fissuring
- Secondary infection with itching and pain are
common
26
FLEXURAL PSORIASIS
- Psoriasis occurs in the axillae, submammary
areas, groin and genitalia - Demarcation is present, but the affected areas
are glazy rather than scaly and is bright red in
color
27
ERYTHRODERMIC AND GENERALIZED PUSTULAR PSORIASIS
- Severe and life threatening condition
- Uncommon
- Whole skin surface is involved and highly
inflammed and the patient is sick - Pustules are sterile and coalesce to form sheets
of pus
28
PSORIATIC ARTHROPATHY
- Occurs in 5 of the patients with psoriasis
- Similar to RA, but RF is negative
- Different patterns
- Distal Arthritis
- Large Joint Involvement
- Spodilitis/ Sacroiliitis
29
- TREATMENT
30
TREATMENTAimed at controlling the
current attack and not curing, and does not
influence future progress of the disease
- TOPICAL THERAPY
- Emolients
- Topical Steroids
- Dithranol
- Coal Tar
- Salicylic Acid
- Vitamin D Analogues
- UVB
- SYSTEMIC THERAPY
- PUVA
- Cytotoxic Drugs
- Immunosuppressant Drugs
- Acitretin
- Photodynamic Therapy
- Systemic Steroids
31
TOPICAL THERAPY
- EMOLIENTS
- Used alone in very mild cases
- Used along with other therapies for moderate to
severe disease
32
- 2. TOPICAL STEROIDS
- Most useful for acutely inflammed psoriasis
- Mild steroids are used on face and flexures
- Potent steroids are used on hands and feet in
combination with Clioquinol or Salicylic acid - Aq. and alcoholic solutions cause stinging and
burning, thus usually ointments, creams and
mousse are prefered - Use of potent steroids on large areas of
psoriasis may cause rebound flare when
discontinued
33
- 3. DITHRANOL
- Burns the skin
- Stains the skin, clothes and bath fittings
- Unsuitable for use on face and flexures and
acutely inflamed psoriasis - 2 regimens - Ingram regimen
- - Short contact regimen
34
- 4. COAL TAR
- Used in combination with emolients, topical
steroids, and salicylic acid - Used for guttate psoriasis, psoriasis of the
scalp, and localized pustular psoriasis of the
palms and soles - Efficiency of coal tar is enhanced when used with
UVB
35
- 5. SALICYLIC ACID
- Useful to remove the scales
- Used in preparation for other treatment
36
- 6. VITAMIN D ANALOGUES
- Efficacy of topical vit D analogues is enhanced
when used in combination with topical steroids
and UVB - Calciptriol Tacalcitol
- Calciptriol is more effective than coal tar and
dithranol. It cannot be used on face. - Tacalcitol is used for once daily treatment of
chronic plaque psoriasis. It can be used on the
face
37
- 7. UVB
- Short wavelength ultraviolet light is used in
combination with coal tar or dithranol - Narrow band UVB is more effective
38
SYSTEMIC THERAPY
- PUVA
- Used for the treatment of moderate to severe
chronic plaque psoriasis - PSORALENS drugs that are activated by UVA
(320-400nm), to interfere with the DNA synthesis
and reduce the epidermal cell turn over - Eg 5-methoxy psoralen 8-methoxy psoralen
- Can be administered orally or it can be applied
topically
39
- The time of exposure is calculated based upon the
previous light testing and the time interval is
increased if tolerated by the patient as the
treatment progresses - Treatment is given twice weekly for 6 weeks
- Unless the disease is severe, maintenance dose is
avoided to minimize the long term side effects - Adverse effects Nausea, pruritis, dry skin,
aging of the skin, melanoma and non-melanoma skin
cancer
40
- 2. CYTOTOXIC DRUGS
- Methotrexate hydroxycarbamide
- METHOTREXATE
- Most effective in the treatment of psoriatic
arthritis - Test dose- 2.5 mg
- Then 30 mg weekly
- Side effects nausea, fatigue, GI bleeding
41
- HYDROXYCARBAMIDE
- It should be used continuously as relapse will
occur when the drug is stopped - Causes bone marrow depression
42
- 3. IMMUNOSUPPRESSANT DRUGS
- CICLOSPORIN
- Severe psoriasis
- Dose is 2-5 mg/kg/day
- Relapse may occur when the drug is stopped but
intermittent therapy is preferred to maintenance
therapy - Avoid sun over exposure, PUVA UVB therapy
43
- 4. ACITRETIN
- Used for severe resistant psoriasis, acute
pustular psoriasis, and palmoplantar psoriasis - Has teratogenic effect
- Re-PUVA therapy acitretin PUVA
- It causes bone maturation abnormality, LFT and
serum lipid levels - Causes dry skin and hair loss
44
- 5. PHOTODYNAMIC THERAPY
- 5-aminolaevullinic acid (ALA) causes local
accumulation of proto porphyrin 9 which is
activated by irradiation with visible light and
causes tissue destruction - Used for localized plaque psoriasis
- Causes burning sensation at the site of treatment
45
- 6. SYSTEMIC STEROIDS
- Not commonly used
- May be used for the management of life
threatening erythroderma - Systemic steroids or their withdrawal may itself
provoke acute generalised pustular psoriasis
46
QUESTIONS???
47
THANK YOU