Atherosclerotic vascular disease - PowerPoint PPT Presentation
1 / 65
Title:
Atherosclerotic vascular disease
Description:
Atherosclerotic vascular disease AVD may manifest as: Coronary artery disease. Cerebrovascular disease. Peripheral vascular disease. Pathophysiology: – PowerPoint PPT presentation
Number of Views:322
Avg rating:3.0/5.0
Title: Atherosclerotic vascular disease
1
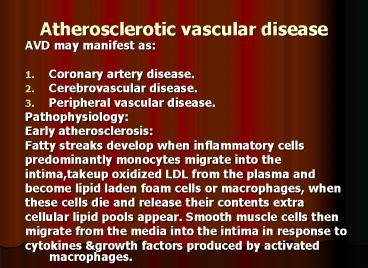
Atherosclerotic vascular disease
- AVD may manifest as
- Coronary artery disease.
- Cerebrovascular disease.
- Peripheral vascular disease.
- Pathophysiology
- Early atherosclerosis
- Fatty streaks develop when inflammatory cells
- predominantly monocytes migrate into the
- intima,takeup oxidized LDL from the plasma and
- become lipid laden foam cells or macrophages,
when - these cells die and release their contents extra
- cellular lipid pools appear. Smooth muscle cells
then - migrate from the media into the intima in
response to - cytokines growth factors produced by activated
macrophages.
2
- The lipid core will be covered by smooth muscle
cells and matrix, producing a stable
atherosclerotic plaque which is asymptomatic
until it becomes large enough to obstruct
arterial flow. - Advanced atherosclerosis
- In an established atherosclerotic plaque
macrophages mediate inflammation smooth muscle
cells promote repair, if inflammation
predominates, the plaque becomes active or
unstable may be complicated by ulceration
superadded thrombosis. Cytokines such as
interleukin-1, tumour necrosis-alpha, interferon
gamma, platelet derived growth factors, and
matrix metalloprotinases are released by
activated macrophages may cause the initial
smooth muscle
3
- Cells overlying the plaque to become senescent
resulting in thinning of the protective fibrous
cap, may lead to erosion, fissuring or rupture of
the plaque surface, exposing its content to
circulating blood, may trigger platelet
aggregation thrombosis, may cause partial or
complete obstruction resulting in infarction or
ischemia of the affected organ.
4
(No Transcript)
5
Risk Factors
- A. Fixed R. F
- Age
- Male sex
- Family history.
- B. Modifiable R.F
- Smoking - Sedentary lifestyle
- Hypertension - Obesity
- Lipid disoder. - Diet
- D.M
- Haemostatic variables
6
- Primary Prevention
- Population advice to prevent coronary disease
- Do not smoke.
- Take regular exercise (minimum of 20 minutes
three times a week). - Maintain ideal body weight .
- Eat a mixed diet rich in fresh fruit
vegetables. - Aim to get no more than 30 of energy intake from
saturated fat.
7
- Secondary prevention
- Patients who already have evidence of
atheromatous vascular disease e.g M.I, are at
high risk of another vascular event, can be
offered a variety of treatment and measures to
improve their outlook (secondary prevention). - Correction of risk factors
- Aspirin
- Beta blockers
- ACE Inhibitors
8
Coronary Heart Disease
- It is the most common form of heart disease.
- Most important cause of premature death.
- In UK 1 in 3 men 1 in 4 women die of CHD.
- Clinical manifestation
- Stable angina.
- Unstable angina.
- M.I
- Heart failure.
- Arrhythmia.
- Sudden death.
9
Stable angina
- Angina pectoris is caused by transient myocardial
ischemia. - It may occur whenever there is an imbalance
between myocardial oxygen supply demand. - Coronary atheroma is the most common cause.
- Other causes include aortic valve disease
hypertrophic cardiomyopathy.
10
- Clinical features
- The history is the most important factor in
making the diagnosis. - Central chest pain, discomfort or breathlessness
that is precipitated by exertion or other forms
of stress, (heavy meal, cold exposure, intense
emotion, lying flat/ decubitus, vivid dreams/
nocturnal angina), and relieved by rest. - Start up angina the pain comes when they start
walking that later it dose not return despite
greater effort. - Physical examination is frequently negative, but
should include - Evidence of valve disease, important risk
factors, left ventricular dysfunction, features
of arterial disease e.g carotid bruits and
untreated conditions that may exacerbate angina
e.g anemia, thyrotoxicosis.
11
- Investigations
- Resting ECG
- Evidence of previous M.I, but may be normal.
- Occasionally T wave flattening or inversion.
- The most important ECG changes is reversible ST
segment depression or elevation with or without T
wave inversion at the time the patient is
experiencing symptoms. - Exercise ECG
- Standard treadmill or bicycle ergometer protocol,
planar or down-sloping ST-segment depression of 1
mm or more is indicative of ischemia, up-sloping
is less specific often occurs in normal
individuals. - Exercise ECG is used to diagnose angina, assess
severity identifying high- risk individuals. - False ve Digoxin, LVH, LBBB, WPW syndrome, the
accuracy is lower in women than men.
12
(No Transcript)
13
(No Transcript)
14
(No Transcript)
15
- Risk stratification in stable
angina. - High Risk post infarct angina, poor effort
tolerance, ischemia at low workload, left main
or three vessel disease, poor LV function. - Low Risk
- Predictable exertional angina, good effort
tolerance, ischemia only at high workload,
single-vessel or minor two-vessel disease, good
LV function. - Other forms of stress testing
- Myocardial perfusion scanning useful when
exercise test is not diagnostic, or patient can
not exercise, its accuracy is higher than
exercise test. - The technique involve obtaining scintiscans of
the myocardium at rest and during stress after
administration of an i.v radioactive isotope e.g
thallium201, it is taken up by viable myocardium.
16
- A perfusion defect present during stress but not
rest indicates reversible myocardial ischemia,
whereas persistent perfusion defect indicates
previous M.I - Stress echocardiography
- It is alternative to perfusion scanning with
similar accuracy. - Uses transthoracic echo to identify ischemic
segments of myocardium area of infarction, the
latter do not contract at rest or during stress. - Coronary arteriography
- Shows the extent nature of coronary artery
disease, it may be indicated when other
investigations fail to diagnose the cause of
atypical chest pain.
17
(No Transcript)
18
- Management
- Assessment of the extent severity of arterial
disease. - Identification control of significant risk
factors - Measures to control symptoms.
- Identification of high risk patients
application of treatment to improve life
expectancy. - Antiplatelet therapy
- Aspirin 75-150 mg reduce the risk of MI,
Clopidogrel 75 mg daily equally effective but
more expensive can be used if the patient has
dyspepsia.
19
(No Transcript)
20
- Anti-anginal drugs
- Nitrates produces venous arteriolar dilatation
- Decrease myocardial oxygen demand (lower preload
afterload) increase myocardial oxygen supply. - Sublingual glyceryl trinitrate (GTN), as aerosol
400 microgm or tablet 300-500 micro-gm
sublingually usually relieve angina in 2-3
minutes, side- effects include headache,
symptomatic hypotension syncope, the tablet
should be replaced 8 weeks after - the bottle has been opened.
- Nitrates can be used prophylactically before
exercise. - GTN is subject to extensive first pass metabolism
in the liver, its ineffeective when swallowed. - Nitrate free period of 6-8 hr. every day to avoid
tolerance.
21
- Preparation Peak action
Duration - Sublingual GTN 4-8
mins 10-30 mins - Buccal GTN 4-10
mins 30-300 mins - Transdermal GTN 1-3 hrs
up to 24 hrs - Oral isosorbide dinitrate 45-120 mins
2-6 hrs - Oral isosorbide mononitrate 45-120 mins
6-10 hrs
22
- Beta-blockers
- Reduce myocardial oxygen demand by reducing heart
rate, BP, and myocardial contractility. - Non-selective BB may exacerbate coronary spasm by
blocking Beta 2 coronary adrenoceptors. - Give once daily cardioselective preparation,
atenolol 50-100 mg daily, slow release metoprolol
200 mg daily, bisoprolol 5-10 mg daily. - ?ß should not be withdrawn suddenly as this may
cause arrhythmia, more angina or MI.(ßß
withdrawal syndrome). - Calcium antagonists
- lower myocardial oxygen demand by reducing blood
pressure and myocardial contractility. - Dihydropyridine calcium antagonists, such as
nifedipine and nicardipine, often cause a reflex
tachycardia it is often best to use these drugs
in combination with a ß-blocker. - In contrast, verapamil and diltiazem are
particularly suitable for patients who are not
receiving a ß-blocker because they inhibit
conduction through the AV node and tend to cause
a bradycardia or even atrioventricular block in
susceptible individuals.
23
- The calcium antagonists may reduce myocardial
contractility and can aggravate or precipitate
heart failure. Other unwanted effects include
peripheral oedema, flushing, headache and
dizziness. - Potassium channel activators
- This class of drug has arterial and venous
dilating properties but does not exhibit the
tolerance seen with nitrates. Nicorandil (10-30
mg 12-hourly orally) is the only drug in this
class currently available for clinical use. - it is conventional to start therapy with low-dose
aspirin, sublingual GTN and a ß-blocker, and then
add a calcium channel antagonist or a long-acting
nitrate later, if necessary.
24
- The goal is the control of angina with minimum
side-effects and the simplest possible drug
regimen. There is little or no evidence that
prescribing multiple anti-anginal drugs is of
benefit, and revascularisation should be
considered if an appropriate combination of two
drugs fails to achieve a symptomatic response. - Invasive treatment The most widely used invasive
options for the treatment of ischaemic heart
disease include percutaneous coronary
intervention (PCI including percutaneous
transluminal coronary angioplasty, PTCA) and
coronary artery bypass graft (CABG) surgery.
25
- UNSTABLE ANGINA
- is a clinical syndrome that is characterised by
new-onset or rapidly worsening angina (crescendo
angina), angina on minimal exertion or angina at
rest. - The condition shares common pathophysiological
mechanisms with acute myocardial infarction, - the term 'acute coronary syndrome' is used to
describe these disorders collectively. - These entities comprise a spectrum of disease
that encompasses ischaemia with no myocardial
damage, ischaemia with minimal myocardial damage,
partial thickness (non-Q wave) myocardial
infarction, and full thickness (Q wave)
myocardial infarction .
26
- An acute coronary syndrome may present as a new
phenomenon or against a background of chronic
stable angina. - The culprit lesion is usually a complex ulcerated
or fissured atheromatous plaque with adherent
platelet-rich thrombus and local coronary artery
spasm . - Diagnosis and risk stratification
- The assessment of acute chest pain depends
heavily on an analysis of the character of the
pain and its associated features, evaluation of
the ECG, and serial measurements of biochemical
markers of cardiac damage, such as troponin I and
T.
27
- A 12-lead ECG is mandatory and is the most useful
method of initial triage. - Evolving transmural infarction is characterised
by persistent ST elevation, new Q waves or new
left bundle branch block - In patients with unstable angina or partial
thickness (non-Q wave or non-ST elevation)
myocardial infarction, the ECG may show ST/T wave
changes including ST depression, transient ST
elevation and T-wave inversion the T-wave
changes are sometimes prolonged. - Approximately 12 of patients with
well-characterised unstable angina or non-ST
segment elevation myocardial infarction progress
to acute infarction or death, and almost
one-third will suffer a recurrence of severe
ischaemic pain, within 6 months of the index
event.
28
- The risk markers that are indicative of an
adverse prognosis include - recurrent ischaemia,
- extensive ECG changes at rest or during pain,
- the release of biochemical markers (creatine
kinase or troponin), - arrhythmias and haemodynamic complications (e.g.
hypotension, mitral regurgitation) during
episodes of ischaemia - those who experience unstable angina following
acute myocardial infarction are also at increased
risk.
29
- Risk stratification is important because it
guides the use of more complex pharmacological
and interventional treatment .
30
- High risk
- Clinical
- Post-infarct anginaRecurrent pain at restHeart
failure - ECG
- ArrhythmiaST depressionTransient ST
elevationPersistent deep T-wave inversion - BiochemistryTroponin T gt 0.1 µg/l
31
- Low risk
- Clinical
- No history of MI
- Rapid resolution of symptoms
- ECG
- Minor or no ECG changes
- Biochemistry
- Troponin T lt 0.1 microgm/ l
32
- The initial treatment should include
- bed rest,
- antiplatelet therapy (aspirin 300 mg followed by
75-325 mg daily long-term and clopidogrel 300 mg
followed by 75 mg daily for 12 months, - anticoagulant therapy (e.g. unfractionated or
fractionated heparin) - ß-blocker (e.g. atenolol 50-100 mg daily or
metoprolol 50-100 mg 12-hourly - A dihydropyridine calcium antagonist (e.g.
nifedipine or amlodipine) can be added to the
ß-blocker, but may cause an unwanted tachycardia
if used alone verapamil or diltiazem is
therefore the calcium antagonist of choice if a
ß-blocker is contraindicated
33
- An intravenous infusion of unfractionated heparin
(with dose adjusted according to the activated
partial thromboplastin time) or weight-adjusted
subcutaneous low molecular weight heparin (e.g.
enoxaparin 1 mg/kg 12-hourly) should be given - If pain persists or recurs, infusions of
intravenous nitrates (e.g. GTN 0.6-1.2 mg/hr or
isosorbide dinitrate 1-2 mg/hr) or buccal
nitrates may help, but such patients should also
be considered for early revascularisation. - Refractory cases or those with haemodynamic
compromise should be considered for a
glycoprotein IIb/IIIa receptor antagonist (e.g.
abciximab, tirofiban or eptifibatide),
intra-aortic balloon pump or emergency coronary
angiography .
34
- Most low-risk patients stabilise with aspirin,
clopidogrel, heparin and anti-anginal therapy,
and can be gradually mobilised. If there are no
contraindications, - exercise testing may be performed prior to or
shortly following discharge. - Coronary angiography should be considered with a
view to revascularisation in all patients at
moderate or high risk, including those who fail
to settle on medical therapy, those with
extensive ECG changes, those with an elevated
plasma troponin and those with severe
pre-existing stable angina. - This often reveals disease that is amenable to
PCI however, if the lesions are not suitable
for PCI the patient should be considered for
urgent CABG.
35
(No Transcript)
36
- MYOCARDIAL INFARCTION
- Myocardial infarction (MI) is almost always due
to the formation of occlusive thrombus at the
site of rupture or erosion of an atheromatous
plaque in a coronary artery. - The thrombus often undergoes spontaneous lysis
over the course of the next few days, although by
this time irreversible myocardial damage has
occurred. - Without treatment the infarct-related artery
remains permanently occluded in 30 of patients. - The process of infarction progresses over several
hours and therefore most patients present when it
is still possible to salvage myocardium and
improve outcome.
37
(No Transcript)
38
- CLINICAL FEATURES
- Pain is the cardinal symptom of MI, but
breathlessness, vomiting, and collapse or syncope
are common features. - The pain occurs in the same sites as angina but
is usually more severe and lasts longer - It is often described as a tightness, heaviness
or constriction in the chest. At its worst, the
pain is one of the most severe which can be
experienced and the patient's expression and
pallor may vividly convey the seriousness of the
situation - Most patients are breathless and in some this is
the only symptom. Indeed, some myocardial
infarcts pass unrecognised.
39
- Painless or 'silent' myocardial infarction is
particularly common in older or diabetic
patients. - If syncope occurs, it is usually due to an
arrhythmia or profound hypotension. Vomiting and
sinus bradycardia are often due to vagal
stimulation and are particularly common in
patients with inferior MI. - Nausea and vomiting may also be caused or
aggravated by opiates given for pain relief. - Sometimes infarction occurs in the absence of
physical signs. - Sudden death, from ventricular fibrillation or
asystole, may occur immediately, and many deaths
occur within the first hour.
40
- If the patient survives this most critical stage,
the liability to dangerous arrhythmias remains,
but diminishes as each hour goes by. - The development of cardiac failure reflects the
extent of myocardial damage and is the major
cause of death in those who survive the first few
hours of infarction.
41
- Physical signs
- Signs of sympathetic activation
- Pallor, sweating, tachycardia
- Signs of vagal activation
- Vomiting, bradycardia
- Signs of impaired myocardial function
- Hypotension, oliguria, cold peripheries
- Narrow pulse pressure
- Raised jugular venous pressure
- Third heart sound
- Quiet first heart sound
- Diffuse apical impulse
- Lung crepitations
- Signs of tissue damage
- Fever
- Signs of complications, e.g. mitral
regurgitation, pericarditis
42
- INVESTIGATIONS
- Electrocardiography The ECG is usually helpful in
confirming the diagnosis however, it may be
difficult to interpret if there is bundle branch
block or evidence of previous MI. - Only rarely is the initial ECG entirely normal,
but in up to one-third of cases the initial ECG
changes may not be diagnostic. - The earliest ECG change is usually ST elevation
later on there is diminution in the size of the R
wave, and in transmural (full thickness)
infarction a Q wave begins to develop. - Subsequently, the T wave becomes inverted, this
change persists after the ST segment has returned
to normal.
43
- In contrast to transmural lesions, partial
thickness or subendocardial infarction causes
ST/T wave changes, without Q waves or prominent
ST elevation this is often accompanied by some
loss of the R waves in the leads facing the
infarct and is also known as non-Q wave or non-ST
elevation myocardial infarction. - The ECG changes are best seen in the leads that
'face' the infarcted area. - When there has been anteroseptal infarction,
abnormalities are found in one or more leads from
V1 to V4 - while anterolateral infarction produces changes
from V4 to V6, in aVL and in lead I.
44
- Inferior infarction is best shown in leads II,
III and aVF, while at the same time leads I, aVL
and the anterior chest leads may show
'reciprocal' changes of ST depression - Infarction of the posterior wall of the left
ventricle does not cause ST elevation or Q waves
in the standard leads, but can be diagnosed by
the presence of reciprocal changes (ST depression
and a tall R wave in leads V1-V4). - Some infarctions (especially inferior) also
involve the right ventricle this may be
identified by recording from additional leads
placed over the right precordium.
45
- The serial evolution of ECG changes in full
thickness myocardial infarction. A. Normal ECG
complex. B. Acute ST elevation ('the current
of injury'). C. Progressive loss of the R
wave, developing Q wave, resolution
of the ST elevation and terminal T wave
inversion. D. Deep Q wave and T wave
inversion. E. Old infarction
46
(No Transcript)
47
- Plasma biochemical markers
- The biochemical markers that are most widely used
in the detection of MI are creatine kinase (CK),
a more sensitive and cardiospecific isoform of
this enzyme (CK-MB), and the cardiospecific
proteins, troponins T and I - The troponins are also released, to a minor
degree, in unstable angina with minimal
myocardial damage Serial (usually daily)
estimations are particularly helpful because it
is the change in plasma concentrations of these
markers that is of diagnostic value.
48
- CK starts to rise at 4-6 hours, peaks at about 12
hours and falls to normal within 48-72 hours. - CK is also present in skeletal muscle, and a
modest rise in CK (but not CK-MB) may sometimes
be due to an intramuscular injection, vigorous
physical exercise or, in old people particularly,
a fall. - Defibrillation causes significant release of CK
but not CK-MB or troponins. The most sensitive
markers of myocardial cell damage are the cardiac
troponins T and I, which are released within 4-6
hours and remain elevated for up to 2 weeks. - Other blood tests A leucocytosis is usual,
reaching a peak on the first day. The erythrocyte
sedimentation rate (ESR) becomes raised and may
remain so for several days. C-reactive protein
(CRP) is also elevated in acute MI.
49
(No Transcript)
50
- Chest X-ray
- This may demonstrate pulmonary oedema that is not
evident on clinical examination The heart size
is often normal but there may be cardiomegaly due
to pre-existing myocardial damage. - Echocardiography
- This can be performed at the bedside and is a
very useful technique for assessing left and
right ventricular function and for detecting
important complications such as mural thrombus,
cardiac rupture, ventricular septal defect,
mitral regurgitation and pericardial effusion.
51
- EARLY MANAGEMENT OF ACUTE MYOCARDIAL INFARCTION
- Provide facilities for defibrillation
- Immediate measures
- High-flow oxygen
- I.v. access
- ECG monitoring
- 12-lead ECG
- I.v. analgesia (opiates) and antiemetic
- Aspirin 300 mg
52
- Reperfusion
- Primary PCI or thrombolysis
- Detect and manage acute complications
- Arrhythmias
- Ischaemia
- Heart failure
- Patients are usually managed in a dedicated
cardiac unit because this offers a convenient way
of concentrating the necessary expertise,
monitoring and resuscitation facilities. - If there are no complications, the patient can
be mobilised from the second day and discharged
from hospital on the fifth or sixth day.
53
- Analgesia
- Adequate analgesia is essential not only to
relieve severe distress, but also to lower
adrenergic drive and thereby reduce pulmonary and
systemic vascular resistance and susceptibility
to ventricular arrhythmias. - Intravenous opiates (initially morphine sulphate
5-10 mg or diamorphine 2.5-5 mg) and antiemetics
(initially metoclopramide 10 mg) should be
administered through an intravenous cannula.
54
- Acute reperfusion therapy
- Thrombolysis
- Coronary thrombolysis helps restore coronary
patency, preserves left ventricular function and
improves survival. - Successful thrombolysis leads to reperfusion with
relief of pain, resolution of acute ST elevation
and sometimes transient arrhythmias (e.g.
idioventricular rhythm). - The sooner the patient is treated, the better the
results will be any delay will only increase the
extent of myocardial damage-'minutes mean
muscle'.
55
- Clinical trials have shown that the appropriate
use of these drugs can reduce the hospital
mortality of myocardial infarction by 25-50 and
follow-up studies have demonstrated that this
survival advantage is maintained for at least 10
years. - The benefit is greatest in those patients who
receive treatment within the first few hours, and
choice of agent is less important than speed of
treatment. - Streptokinase, 1.5 million U in 100 ml of saline
given as an intravenous infusion over 1 hour, is
a widely used regimen. Streptokinase is antigenic
and occasionally causes serious allergic
manifestations. It may also cause hypotension,
which can often be managed by stopping the
infusion and restarting at
56
- slower rate.
- Circulating neutralising antibodies are formed
following treatment with streptokinase and may
persist for 5 years or more. - These antibodies can render subsequent infusions
of streptokinase ineffective so it is advisable
to use another non-antigenic agent if the patient
requires further thrombolysis in the future. - Alteplase (human tissue plasminogen activator or
tPA) is a genetically engineered drug that is not
antigenic and seldom causes hypotension. The
standard regimen is given over 90 minutes (bolus
dose of 15 mg, followed by 0.75 mg/kg body
weight, but not exceeding 50 mg, over 30 minutes
and then 0.5 mg/kg
57
- body weight, but not exceeding 35 mg, over 60
minutes). - There is evidence that tPA may produce better
survival rates than streptokinase, particularly
among high-risk patients (e.g. large anterior
infarct), but with a slightly higher risk of
intracerebral bleeding (10 per 1000 increased
survival, but 1 per 1000 more non-fatal stroke). - Newer-generation analogues of tPA have been
generated that have a longer plasma half-life and
can be given as an intravenous bolus. Large-scale
trial data have demonstrated that tenecteplase
(TNK) is as effective as alteplase at reducing
death and MI whilst conferring similar
intracerebral bleeding risks.
58
- Reteplase (rPA) is administered as a double bolus
and trial data indicate a similar outcome to that
achieved with alteplase, although some of the
bleeding risks appear slightly higher. The double
bolus administration may provide practical
advantages over the infusion of alteplase. - An overview of all the large randomised trials
confirms that thrombolytic therapy significantly
reduces short-term mortality in patients with
suspected MI if it is given within 12 hours of
the onset of symptoms and the ECG shows bundle
branch block or characteristic ST segment
elevation of greater than 1 mm in the limb leads
or 2 mm in the chest leads.
59
- Thrombolysis appears to be of little net benefit,
and may be harmful in other patient groups,
specifically those who present more than 12 hours
after the onset of symptoms and those with a
normal ECG or ST depression. - The major hazard of thrombolytic therapy is
bleeding.
60
- RELATIVE CONTRAINDICATIONS TO THROMBOLYTIC
THERAPY (POTENTIAL CANDIDATES FOR PRIMARY
ANGIOPLASTY) - Active internal bleeding
- Previous subarachnoid or intracerebral
haemorrhage - Uncontrolled hypertension
- Recent surgery (within 1 month)
- Recent trauma (including traumatic resuscitation)
- High probability of active peptic ulcer
- Pregnancy
61
- Primary percutaneous coronary intervention (PCI)
- In institutions that are able to offer rapid
access (within 3 hours) to a 24-hour catheter
laboratory service, percutaneous coronary
intervention is the treatment of choice. - In comparison to thrombolytic therapy, it is
associated with a 50 greater reduction in the
risk of death, recurrent myocardial infarction or
stroke.
62
- The widespread use of PCI has been limited by the
availability of the resources necessary to
achieve this highly specialized emergency
service. - As a consequence, intravenous thrombolytic
therapy remains the first-line reperfusion
treatment in many hospitals. - For some patients, thrombolytic therapy is
contraindicated or fails to achieve coronary
arterial reperfusion. Early emergency PCI (within
6 hours of symptom onset) may be considered under
such circumstances, particularly where there is
evidence of cardiogenic shock.
63
- Acute right
- Coronary art.
- Occlusion.
64
- Initial angio Filling defect
65
- Complete resolution of flow following insertion
of stent