CARIES RISK GUIDELINES (American Dental Association 1996) - PowerPoint PPT Presentation
1 / 35
Title:
CARIES RISK GUIDELINES (American Dental Association 1996)
Description:
CARIES RISK GUIDELINES (American Dental Association 1996) LOW: No carious lesions in last year Coalesced or sealed pits and fissures Relatively plaque free – PowerPoint PPT presentation
Number of Views:177
Avg rating:3.0/5.0
Title: CARIES RISK GUIDELINES (American Dental Association 1996)
1
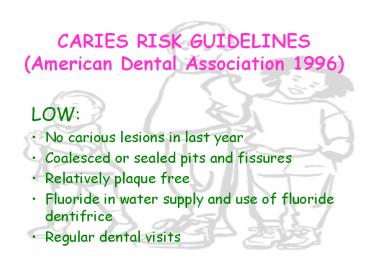
CARIES RISK GUIDELINES(American Dental
Association 1996)
- LOW
- No carious lesions in last year
- Coalesced or sealed pits and fissures
- Relatively plaque free
- Fluoride in water supply and use of fluoride
dentifrice - Regular dental visits
2
CARIES PREVENTION MODALITIES FOR CHILDREN BY RISK
CATEGORY(American Dental Association, 1996)
- LOW
- Educational reinforcement
- Plaque removal (oral physiotherapy)
- Fluoride dentifrice
- One year recall
3
CARIES RISK GUIDELINES(American Dental
Association, 1996)
- MODERATE
- One carious lesion in the last year
- Deep pits and fissures
- Some plaque accumulation
- No fluoride in water
- White spot lesions
- Irregular dental visits
- Orthodontic treatment
4
CARIES PREVENTION MODALITIES FOR CHILDREN BY RISK
CATEGORY(American Dental Association, 1996)
- MODERATE
- Pit and Fissure Caries
- Sealants
- Smooth Surface Caries
- Education
- Dietary Counseling
- Fluoride dentifrice (low potency fluoride)
- Fluoride mouthrinse (low potency fluoride)
- Professional topical fluoride (high potency
fluoride) - Six month recall
- Fluoride supplements (depending on age of child
and absence of water fluoridation)
5
CARIES RISK GUIDELINES(American Dental
Association, 1996)
- HIGH
- Two ore more carious lesions in last year
- Past smooth surface caries
- Elevated mutans streptococci count
- Deep pits and fissures
- No or little systemic and topical fluoride
exposure - Plaque accumulation
- Frequent fermentable carbohydrate intake
- Irregular dental visits
- Inadequate salivary flow
- Inappropriate nursing habits (infants)
6
CARIES PREVENTION MODALITIES FOR CHILDREN BY RISK
CATEGORY(American Dental Association, 1996)
- HIGH
- Pit and Fissure Caries
- Sealants
- Smooth Surface Caries
- Education
- Dietary counseling
- Fluoride dentifrice
- Fluoride mouthrinse
- Professional topical fluoride (3-6 months)
- Three to six month recall
- Monitoring of mutans Streptococci
- Antimicrobial agents (Chlorohexidene)
- Fluoride supplements ( depending on age of child
and presence of water fluoridation
7
PREVENTION V
- DENTAL (PIT AND FISSURE) SEALANTS
8
HISTORY
- The concept of sealing the fissures of teeth is
over 100 years old. In 1895, Wilson, described in
Dental Digest the use of oxyphosphate cement to
seal fissures. - Contemporary pit and fissure sealants were
introduced into clinical dentistry in 1967 by
Michael Buonocore of the Eastman Dental Center,
Rochester. - Dr. Buonocore is credited with developing the
field of adhesive dentistry through his
introduction of the concept of acid etching of
tooth enamel, and his documentation of the
ability of resin materials to adhere to such
etched enamel surfaces. - The effectiveness of pit and fissure sealants as
a preventive tool was recognized with provisional
approval by the American Dental Association
Council on Dental Therapeutics in 1971 full
approval came in 1976. - Since then the use of pit and fissure sealants,
now generally referred to as dental sealants, has
increased steadily.
9
SEALANT USAGE
- Surveys show an increase in sealant use among
dentists from 38 in 1974 to as high as 90-95 of
dentists in recent surveys. - The U.S. Public Health Services goal for Healthy
People-2000 called for at least 50 of children
8-14 to have sealants placed. - Although no studies of sealant prevalence have
been completed this year, it is thought that the
prevalence of use will fall far below this goal. - The prevalence of sealant usage in eight year
olds grew from 7 to 15 from 1986 to the early
90s during the same time period the percentage
of fourteen year olds with sealants grew from 8
to 35. When all school aged children are
included, 18.5 had one or more sealed teeth in
1991.
10
CARIES PREVALENCE
- As we have discussed, there has been a
significant decline in caries prevalence among
school aged children in the past 20-30 years. - Recall that the mean DMFS for school children in
1980 was 4.77, and had declined to 3.07 in 1986
a 36 reduction. - 50 of school children were caries free in 1986,
versus 37 in 1980.
11
COMPARISON OF AGE-SPECIFIC MEAN DMFS SCORES
1980,1987
12
COMPARISON OF AGE-SPECIFIC PERCENT OF CARIES FREE
CHILDREN 1980,1987
13
RELATIVE DISTRIBUTION OF CARIES
- Not only has there been a change in the number of
tooth surfaces affected by dental caries, but
there has been a change in the relative
distribution, or pattern, of caries on different
tooth surfaces. - There has been a greater percentage reduction for
smooth surface caries (mesial and distal
surfaces) compared to pit and fissure caries. - According to the latest survey, 58 of the
caries observed on school childrens teeth is
observed on the occlusal surfaces. - Overall, 88 of the caries in school children
occurs in pits and fissures, and only 12 on the
proximal surfaces. - This differential is related to the more
significant impact of fluorides on smooth
surfaces in reducing enamel solubility and
serves to underscore the imperative of dental
sealants in a comprehensive program of prevention.
14
DISTRIBUTION OF DENTAL CARIES BY TOOTH SURFACE
TYPE OF CHILDREN
15
TOOTH SURFACE ATTACK RATES IN PERMANENT TEETH BY
SURFACE
16
PRINCIPLES UNDERLYING SEALANT USE
- Prevention of dental caries is preferable to
treatment sound, nondiseased teeth are to be
more highly valued than adequately restored
teeth. - For equivalent outcomes, the least invasive
approach, using the simplest intervention for
managing dental caries is preferred. - Minimizing the cost of preventing or controlling
pit and fissure caries is desirable. - Strategies for sealant use may vary between
individual care and community-based programs.
17
SCIENTIFIC FACTS RELATED TO SEALANT USE
- Sealants have been demonstrated to be a safe and
effective long-term method to prevent pit and
fissure caries. - Pit and fissure caries attack begins in childhood
and continues through adolescence and into
adulthood. - In addition to preventing carious lesions,
sealants can arrest caries progression. - Effective sealant use requires meticulous
attention to detail in application technique,
particularly moisture control. Sealant retention
should be checked within one year of application.
18
RISK ASSESSMENT IN TREATMENT PLANNING FOR SEALANTS
- Determination of the need for sealants begins
with an assessment of the individuals risk for
dental caries, as well as an assessment of the
risk of the individual tooth. - Factors contributing to individual risk include
- caries history
- previous dental care
- use of preventive practices
- dietary habits
- Factors to evaluate when considering individual
teeth include - individuals risk for developing caries
- pit and fissure morphology
- caries pattern
- status of the proximal surface of the tooth in
question.
19
TREATMENT DECISION MAKING
- Studies suggest that the first and second
permanent molars are at the greatest risk for pit
and fissure caries premolars are at
significantly less risk. - Primary teeth have an aprismatic layer of enamel
and do not etch in the same manner as permanent
teeth, consequently sealant retention is not as
great on primary teeth. Additionally, the grooves
of primary teeth tend to be well-coalesced in
comparison to permanent teeth. - In general, we do not seal primary teeth.
- The cost-benefit effectiveness is greatest in
sealing first and second permanent molars, and
they should be given preferential treatment to
premolars in application of sealants. - Sealants are not necessarily indicated for
permanent molars with well-coalesced grooves and
no history of dental caries. - Indiscriminate sealing of teeth with low risk of
caries reduces the cost effectiveness of sealants.
20
EFFICACY OF SEALANTS
- Sealants are effective as long as they remain
intact. With complete retention sealed surfaces
are virtually impervious to decay. - Therefore, the effectiveness of sealants in
preventing decay is measured by the retention of
the sealant.
21
VARIABLES AFFECTING SEALANT RETENTION
- Position of the teeth in the mouth
- better sealant retention in mandibular versus
maxillary arch--??? - Skill of operator
- more skillful and experienced operators produce
better sealant retention - Eruption status of the tooth
- the younger the child, the more difficult to
maintain a dry field due to the eruption status
of the teeth partially erupted molars are
difficult to isolate. - Patient Cooperation
- children who present problems with cooperation
make gaining and maintaining a dry field more
difficult.
22
SEALANT RETENTION
- A compilation and summary of over 75 studies of
sealant retention indicates - 94 of sealants were intact after one year
- 83 of sealants were intact two years after
placement. - 67 were intact five years after placement.
- 57 were intact after ten years.
23
UPDATING TECHINQUEMATERIALS
- There is a wide variety of sealant materials from
which to choose. - Sealants are often classified by their method of
polymerization, either autopolymerizing
(chemically cured), or visible light-cured
sealants they are also classified by whether
they are filled resins, or unfilled
resins--though increasingly the market is
dominated by filled resins. - Numerous studies have compared bond strengths and
retention rates between the two and found they
offer comparable results.
24
UPDATING TECHNIQUECLEANING THE FISSURE
- Prior to acid etching the enamel, it is important
to be sure that the tooth surface and fissure
areas are free of gross plaque that might
interfere with the etching process. - Historically, it was recommended that this be
done with a prophylaxis cup or bristle brush and
pumice. - Recent studies have shown that cleaning the tooth
with a pumice prophylaxis does not significantly
increase bond strength. - Current recommendation is to run an explorer
through the fissures and rinse forcefully with
water or, brush the fissures thoroughly with a
tooth brush to remove the gross plaque. - Complete debridement of plaque from the fissure
is viewed to be essentially impossible and not an
imperative for successful etching and sealant
retention.
25
UPDATING TECHNIQUEISOLATION
- Adequate isolation of the tooth is the most
critical aspect of the sealant application
process. - Salivary contamination of a tooth surface during
or after acid etching will have a deleterious
effect on the ultimate bond between the enamel
and resin. - Studies have shown that even a one second
exposure of etched enamel to saliva adversely
affected bond strength and sealant retention. - Several studies have shown that rubber dam
isolation and cotton roll isolation provide
comparable retention rates. - However, it is obvious that rubber dam provides
the best, most controllable isolation. - When sealants are treatment planned for a tooth
in a quadrant where restorative therapy will also
be accomplished, the sealant should be placed
under rubber dam isolation in the context of the
restorative treatment.
26
UPDATING TECHNIQUEETCHING
- The most commonly used etchant is 37
orthophosphoric acid it is available as both a
liquid and a gel. - Etchant should be applied to all of the fissures
and extend 2mm up the the cuspal inclines. - Soft tissue exposure to the etchant is to be
avoided. - Historically, etchant times were 30-60 seconds
however, recent studies have concluded that 15-20
seconds is comparable and adequate. - Rinse time is not important as previously thought
(20 seconds). What is critical is that the
etchant be completely rinsed away. - On thorough drying the enamel should present a
chalky, frosted appearance if it does not, it
must be re-etched..
27
DEMINERALIZATION PATTERNS(SEM X5,000)
- Enamel prism centers mainly involved
28
DEMINERALIZATION PATTERNS(SEM X 5,000)
- Enamel prism peripheries mainly involved.
29
UPDATING TECHNIQUEAPPLYING THE SEALANT
- All susceptible pits and fissures should be
sealed this includes the buccal pit of
mandibular molars, and the lingual groove of
maxillary molars. - Some studies have shown that using a bonding
agent as an intermediate step, prior to placing
the sealant increases sealant retention. Other
studies have not confirmed this. Typically most
recommended techniques, a bonding agent is not
required. However, it may be used if desired. - Care should be taken not to place excess sealant,
which may affect the childs occlusion and
increase the potential for the sealant bond being
fractured.
30
PENETRATION OF MICROSCOPIC SEALANT TAGS
31
OCCLUSAL SEALANT AFTER REMOVAL OF ENAMEL BY
DEMINERALIZATION
32
INNER SURFACE OF SEALANT AFTER REMOVAL OF ENAMEL
BY DEMINERALIZATION
33
POLYMERIZED SEALANT TAGS (SEM X 3,000)
34
UPDATING TECHNIQUEPOLYMERIZATION
- In one study it was found that the longer
sealants were allowed to remain on the tooth
surface before being polymerized, the more
sealant penetrated the microporosities, creating
longer resin tags, which are the critical
dimension for micromechanical retention. - Sealants in which polymerization was not
effected for 20 seconds after application, had
nearly three times longer resin tags than those
of sealants polymerized after 5-10 seconds. - When isolation can be adequately maintained, it
appears to be beneficial to wait for 20 seconds
after sealant application before applying the
light activation.
35
UPDATING TECHNIQUEEVALUATING THE SEALANT
- All sealants should be visibly and tactually
inspected for complete coverage, and the absence
of voids or air bubbles. - Attempts should be made to dislodge the sealant
with an explorer. - An evaluation of the occlusion should be
conducted. Filled resin sealants (which we
utilize) in contrast to unfilled resin sealants,
are not easily abraded and can create occlusal
interferences. They should be adjusted with a
rotary instrument, if determined to be in
hyperocclusion. - The interproximals of the tooth should be
evaluated as well to ensure no sealant has flowed
into the area inadvertently.