Mechanisms of Action Antifungal Drugs - PowerPoint PPT Presentation
1 / 26
Title:
Mechanisms of Action Antifungal Drugs
Description:
Attaches to ergosterol disrupts cell membrane cell lysis ... Big pharmaceutical companies. Smaller ($) market for anti-infectives ... – PowerPoint PPT presentation
Number of Views:2052
Avg rating:3.0/5.0
Title: Mechanisms of Action Antifungal Drugs
1
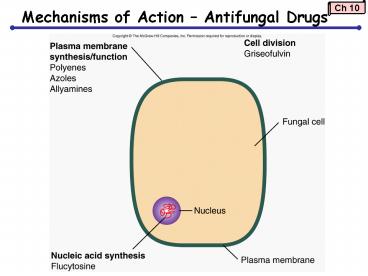
Mechanisms of Action Antifungal Drugs
2
Interference with Membrane Integrity
- Polyenes
- Attaches to ergosterol ? disrupts cell membrane ?
cell lysis - Some toxicity to humans due to binding of
cholesterol - ex amphotericin B
- Azoles
- Inhibition of ergosterol synthesis ? disrupts
cell membrane ? cell lysis - ex miconazole, ketoconazole
3
Disruption of Cytoplasmic Membranes
Figure 10.5
4
Mechanisms of Action Antiparasitic Drugs
- Antiparasitic drugs often very specific ? ID
organism - Antiprotozoan drugs
- interfere with biosynthetic pathways
sulfonamides, trimethoprim - Heavy metals, quinines, azoles
- Antihelminthic drugs
- interfere with neuromuscular function
praziquantel - Niclosamide, azoles
- Most diseases are in developing world - need more
!
5
Spectrum of Action
Figure 10.8
6
Antimicrobial Efficacy
- Tests used to determine susceptibility of a
bacterial strain to a specific antibiotic - MIC
- MBC
- Antibiotic discs
7
Minimum inhibitory concentration (MIC)
- Serial dilutions of concentrations of drug
- Add known concentration of organisms
- Incubate gt16 hrs
- Examine for turbidity
- Minimum bacteriocidal concentration (MBC)
lowest concentration of a specific antimicrobial
drug that kills 99.9 of a given strain of
bacteria - Must assay for live organisms from MIC test
- MIC and MBC precise but labor-intensive and
expensive
8
Minimum inhibitory concentration lowest
concentration that inhibits growth
Figure 10.10
9
Minimum Bactericidal Concentration (MBC) Test
Figure 10.12
10
Kirby-Bauer Test Antibiotic Disc Diffusion
- Bacterial lawn plated on agar
- Filter paper discs with specific concentration of
drug on bacterial surface - Clear area surrounding disc zone of inhibition
around disc
11
Etest
Figure 10.11
12
Resistance to Antimicrobial Drugs
- How does resistance arise?
- How does resistance spread?
13
Antimicrobial Resistance
- Innate/ intrinsic resistance inherent
resistance - Acquired resistance previously sensitive
organisms develop resistance
14
Mechanisms of Resistance
Non-Resistant Cell
- Antibiotic Resistance
- Drug-inactivating enzymes
- Alteration in target molecule
- Decreased drug uptake
- Increased drug elimination
Resistant Cell
15
Drug-Inactivating Enzymes
- ?-lactamase (penicillinase) renders penicillin
inactive
16
Alteration in the Target Molecule
- Alteration in the ribosome ? inhibits binding of
erythromycin
17
Decreased Drug Uptake
- Some cells have mutated to decrease uptake of
tetracycline
18
Increased Drug Elimination
- Efflux pumps proteins present in cell membrane
that expels substances out of the cell - E. coli resistance to triclosan
19
Antimicrobial Resistance!
R plasmids resistance plasmids Multiple
Resistance R plasmids can carry resistance to
multiple antimicrobials Superbugs resistance to
most antimicrobial agents Cross resistance
resistance to one antimicrobial confers
resistance to another
- Horizontal evolution through gene transfer
20
Emerging Antimicrobial Resistance
- Staphylococcus aureus
- Common, nosocomial infections
- Most strains contain penicillinase
- MRSA methicillin-resistant S. aureus
- Enterococcus (faecium or faecalis)
- Common, nosocomial infections
- VRE vancomycin-resistance enterococcus
- Mycobacterium tuberculosis
- Slow growth ? treatment is long
- High number of organisms in active infection ?
high probability of spontaneous mutation ?
complicated treatment - MDR-TB multi-drug resistant tuberculosis
21
CDC Campaign to Prevent Resistance in
Healthcare Settings
- http//www.cdc.gov/drugresistance/healthcare/defau
lt.htm
- Limiting Antibiotic Resistance
- Completing the entire course of antibiotics
- Use antibiotics in combination
- Limit use to necessary cases
- Develope new variants of existing drugs
22
Strategies for New Antibiotics
- Modifying current antibiotics
- Utilizing mechanisms of resistance when modifying
current antibiotics - Identifying/ inhibiting new antibiotic targets
- Bacteriophage viruses that only infect bacteria
- Use enzymes from phage
- 5. Strengthen/ imitate normal immune system
funciton - 6. Exploration of environmental sources (marine,
soil)
23
Some New Antibiotics
- Quinupristin-Dalfopristin FDA approved 1999
- Useful against Gram()
- Class streptogramins (lincosamidemacrolide)
- Linezolid FDA approved 2000
- Useful against Gram() and Gram(-)
- Class oxazolidinones
- Daptomycin FDA approved 2003
- Useful against Gram() only
- Causes depolarization of cell membrane
- New class of antibiotics
- Telithromycin FDA approved 2004
- Useful against Gram() only
- Inhibits activity of large ribosomal subunit
- Class ketolides / macrolides
24
Why isnt there more development?
- Big pharmaceutical companies
- Smaller () market for anti-infectives
- Combinatorial chemistry and genomics have not
delivered easy drugs/ drug targets - Years to complete process
25
(No Transcript)
26
(No Transcript)