General Surgeon In Pune - Laparoscopy Surgeon In Pune - PowerPoint PPT Presentation
Title:
General Surgeon In Pune - Laparoscopy Surgeon In Pune
Description:
Dr. Sanjay Kolte, a general surgeon based in India who specializes in laparoscopic,Thoracoscopic,gastrointestinal, Emergency and General surgery. – PowerPoint PPT presentation
Number of Views:279
Title: General Surgeon In Pune - Laparoscopy Surgeon In Pune
1
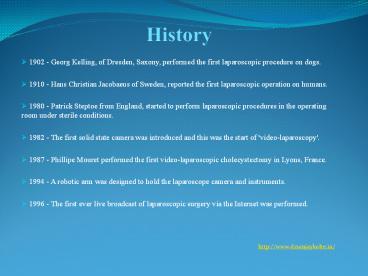
History
- 1902 - Georg Kelling, of Dresden, Saxony,
performed the first laparoscopic procedure on
dogs. - 1910 - Hans Christian Jacobaeus of Sweden,
reported the first laparoscopic operation on
humans. - 1980 - Patrick Steptoe from England, started to
perform laparoscopic procedures in the operating
room under sterile conditions. - 1982 - The first solid state camera was
introduced and this was the start of
'video-laparoscopy'. - 1987 - Phillipe Mouret performed the first
video-laparoscopic cholecystectomy in Lyons,
France. - 1994 - A robotic arm was designed to hold the
laparoscope camera and instruments. - 1996 - The first ever live broadcast of
laparoscopic surgery via the Internet was
performed. - http//www.drsanjaykolte.in/
2
What is Laparoscopic Surgery?
- Laparoscopic surgery, also known as minimally
invasive surgery (MIS) or keyhole surgery is a
modern surgical technique for carrying out
operations in the abdomen through cannulae (also
known as ports) which are channels into the body
through small incisions. - Using a video camera the surgeon is able to view
the operative field without invasive surgery. The
abdomen is usually insufflated with carbon
dioxide gas. - By inflating the abdomen, the abdominal wall is
elevated above the internal organs to create a
working and viewing space for the surgeons. - http//www.drsanjaykolte.in/
3
Why Laparoscopy?
- There are a number of advantages to operating on
the patient with laparoscopic surgery versus open
surgery. Some of these are - Less post-operative scarring
- Reduced pain
- Shorter recovery time
- Less time spent in hospital to recover
- Reduced hemorrhaging
- Reduced risk of exposing internal organs to
external contaminants - Quicker return to normal activities
- Quicker return to work
4
- The Rise of Bariatric Surgery
- One of the most common types of laparoscopic
surgery is bariatric (obesity). Over the last
decade there have been more advancements in
bariatric surgery than there had been in the
previous 50 years, fuelled largely by the growing
obesity epidemic which began in the 1970s. The
epidemic created the need for effective treatment
of severe obesity and its co morbidities leading
to the development of procedures such as gastric
banding, gastric bypass and duodenal switch over
the past decade. More recently, the advent of
minimally invasive surgery in the mid-1990s
accounted for the second wave of advances. - Before Laparoscopic Surgery
- Before laparoscopy was practiced, surgeons
operated using open/invasive surgery. This means
cutting skin and tissues so that the surgeon has
direct access to structures and organs. This
involves more direct access than in minimally
invasive procedures as the openings are bigger so
the internal organs are openly exposed. - http//www.drsanjaykolte.in/
5
Laparoscopic Surgery
- Cholecystectomy, Appendectomy Colectomy
- Vagotomy
- Hiatal, Inguinal Diaphragmatic hernia
repair - Urological- Nephrectomy, Adrenelectomy
Prostatectomy. - OBG-Tubal surgeries,cystectomies,hystrectomie
s various ablations (endometriosis) - Thoracoscopies
- Neurosurgeries
- Lumbar discectomies
- Diagnostic procedures
- http//www.drsanjaykolte.in/
6
Advantages and Disadvantages
- Advantages
- Minimal pain illeus
- Improved cosmesis
- Shorter hospital stay , faster recovery rapid
return to work - Non muscle splinting incision less blood loss
- Post op respiratory muscle function returns to
normal more quickly - Wound complications i.e. infection dehiscence
are less - Lap surgery can be done as day care surgery
- Disadvantages
- Longer duration of surgery
- Loss of 3D view, impaired touch sensation
- poor dexterity, fulcrum effect, risk of visceral
/ vsl. Injury (may go unrecognised) - Long learning curve for surgeons
- http//www.drsanjaykolte.in/
7
Fig. Demonstarting surgical incision Sites in lap
cholecystectomy
8
INSUFFLATING GAS OF CHOICE FOR LAPROSCOPY
- Ideal insufflating gas of choice
- Colorless, non toxic, nonflammable, easily
available, inexpensive, inert, readily soluble in
blood and easily ventilated out of lungs - Why CO2 is the gas of choice for laparoscopy?
- Nonflammable does not support combustion
- Highly soluble in blood because of rapid
buffering in blood so risk of embolisation is
small - Rapidly diffusible through membranes so
easily removed by lungs - CO2 levels in blood expired air can be
easily measured its elimination is augmented by
increasing ventilation - CO2 is readily available is inexpensive
- http//www.drsanjaykolte.in/
9
PROPERTIES OF OTHER GASES USED
Gas Oswalds BG solubility coef. complications
Air 0.017 Supports combustion, Gas embolism
Oxygen 0.036 do
Nitrogen Gas embolism
N2O 0.042 Supports combustion (if mixed with methane from bowel), Bowel distension, PONV, Explosion with cautery
CO2 0.49 Hypercarbia, Pain abdomen ,Shoulder tip pain, Arrythmia, Promotion of port site tumour growth, peritoneal irritant
He 0.00098 Embolism, diffusible, expensive
Argon Embolism, expensive
- http//www.drsanjaykolte.in/
10
PHYSIOLOGICAL CHANGES
- Physiologic effects seen with CO2 insufflations
are transient and derive from the body's reaction
to increases in intra abdominal pressure and CO2
absorption as it tries to achieve a new state of
homeostasis. People who are otherwise healthy
will tolerate laparoscopy well, while individuals
with underlying cardiopulmonary or renal diseases
may not tolerate prolonged CO2 insufflations.
Additionally, patient positioning, for example
steep Trendelenburg in prostatectomy, can
exacerbate cardiovascular alterations in
laparoscopy. - http//www.drsanjaykolte.in/
11
CARDIOVASCULAR RESPONSE
- Cardiovascular changes vary with intra abdominal
pressure, with higher pressures associated with
more significant changes than lower pressures. In
any other case healthy patients undergoing
laparoscopy, the threshold intra abdominal
pressure that led to hemodynamic changes was 12
mm Hg. Those with underlying cardiac disease will
likely have a lower intra abdominal pressure
threshold. - Heart rate may rise transiently in response to
increases in SVR and arterial blood pressure
level to maintain cardiac output, but most
studies have reported no significant long-term
changes in heartbeat with laparoscopy. In a tiny
subset (0.5) of otherwise healthy patients,
however, bradycardia and asystole can occur
during CO2 insufflation and pneumoperitoneum. - http//www.drsanjaykolte.in/
12
RESPIRATORY RESPONSE
- CO2 may be the gas of choice for laparoscopic
surgeries because it is noncombustible, extremely
soluble, and readily eliminated with the lungs. - Despite the proven effectiveness and protection
of CO2 for insufflation in laparoscopy, the
respiratory response to mechanical improves in
intra abdominal pressure as well as hypercapnia
from absorption should be considered. - With CO2 insufflation and increases in intra
abdominal pressure, the dintra abdominal
pressurehragm is pushed cephalad into the
thoracic cavity, constraining downward dintra
abdominal pressurehragmatic excursion with
respiration. All round functional respiratory
capacity, vital capacity, and pulmonary
compliance drop with boosts in intra abdominal
pressure, and peak airway and plateau pressures
can enhance up to 50 and 81, respectively. - http//www.drsanjaykolte.in/
13
RENAL RESPONSE
- Mechanistically, as intra abdominal pressure
increases, its compressive effects on the renal
vasculature, the renal parenchyma, and the IVC
will reduce effective renal blood circulation
(ERBF), cortical and medullary perfusion, and
renal venous outflow. - The renal effects are mild to negligible once the
intra abdominal pressure is under 10 mm Hg, but
as intra abdominal pressure reaches and exceeds
15 mm Hg, there's a pressure-dependent decrease
in the glomerular filtration rate (GFR), ERBF,
creatinine clearance, sodium excretion, and
urinary output. In a typical intra abdominal
pressure of 15 mm Hg, urinary output decreases by
as much as 63 to 64, GFR by 21, and ERBF by
26. Despite this drop, however, there are no
long-term renal squeal, even in patients with
pre-existing renal disease, and
pneumoperitoneum-induced renal failure does not
occur. - http//www.drsanjaykolte.in/
14
METABOLIC RESPONSE
- Metabolic acidosis from CO2 absorption is the
primary derangement with laparoscopy. Systemic
CO2 absorption and resultant metabolic
consequences differ depending on the patient's
underlying respiratory status since the lung
eliminates absorbed CO2 buffered by the blood. In
otherwise healthy patients, an increase in minute
ventilation is enough, but for individuals with
COPD, removal of CO2 is less capable, causing
them to are afflicted by more major and extended
derangements in acid-base balance. As stated
earlier, desufflation might be necessary during a
long laparoscopic procedure in patients with COPD
or interstitial lung condition. - http//www.drsanjaykolte.in/
15
Causes for Paco2 during Laparoscopy
- Absorption of carbon dioxide (CO2) from the
peritoneal cavity - VA/Q mismatch
- Increased physiologic dead space
- Abdominal Distention
- Position of the patient (e.g., steep tilt)
- Controlled mechanical ventilation
- Reduced cardiac output
- These mechanisms are accentuated in sick patients
- Increased metabolism (e.g., insufficient plane of
anesthesia) - Depression of ventilation by anesthetics (e.g.,
spontaneous breathing) - Accidental events
- CO2 emphysema (i.e., subcutaneous or body
cavities) - Capnothorax
- CO2 embolism (Selective bronchial intubation)
16
ANAESTHESIA
- PAC
- Done in usual manner with special attention to
cardiac pulmonary system - Investigations
- Complete hemogram
- RBS
- Na, K
- BUN, Creatinine
- Coagulation profile
- CXR, ECG
- BG, CM
- Special investigations
- ECHO
- PFT
- http//www.drsanjaykolte.in/
17
PREMEDICATION
- NPO
- Complete bowel preparation
- Antibiotics as per surgical team
- Awareness about post op shoulder tip pain
- Written informed consent for laparotomy
- Anxiolytics/antiemetics/H2 receptor
antagonist/analgesic - Antisialagogue (glyco-P) and vagolytic may be
administered at induction of anaes. - DVT prophylaxis (rTn, pelvic Sx, long
duration, malignancy, obesity) - Clonidine/ dexmetetomidine to decrease stress
response - http//www.drsanjaykolte.in/
18
MONITORING
- HR
- NIBP
- Continous ECG
- Pulse oximetry
- Capnography
- Temperature
- Airway pressure
- IAP
- If required, ABG, precordial doppler,TEE may
be instituted. - http//www.drsanjaykolte.in/
19
CO2 s/c emphysema
- Cause
- accidental extraperit insufflation
(malpositioned verris needle) - deliberate extraperit insufflations-
retroperit surg,TEPP,fundoplication, pelvic
lymphadenectomy - Diagnosis
- ETCO2 -cannot be corrected by adjusting
ventilation even after plateau reached - ABG, Palpation
- Treatment
- Stop CO2 insufflation, interrupt lap
temporarily - CMV continued till hypercapnia resolves
- Resume lap at low insufflation P thereafter
- http//www.drsanjaykolte.in/
20
Pneumothorax / pneumomediastinum
- Cause
- pleuroperitoneal communications (RgtL)
- Diaph defects( aortic, esophageal, GE jn surg)
- Rupture of preexisting bullae
- Perf falciform ligament
- Diagnosis
- airway P, sudden ?Sp O2 , sudden ?/ ? ETco2,
- Abnormal motion of hemidiaph by laparoscopist
- PNEUMOTHORAX
CAPNOTHORAX ? ET CO2 (may fall later) ? V CO2, ? PaCO2, AIR PNEUMOTHORAX ?ET CO2 (due to ?CO)
Stop N2O 100 O2 IAP PEEP Thoracocentesis not needed Inform surgeon Do not apply PEEP Mandatory
21
CO2 embolism (rare but potentially fatal)
- Risk factors
- hysteroscopies, previous abd surg, needle/Trocar
in vsl - Consequences-
- GAS LOCK in vena cava ,RA ? ? VR ? collapse -
Ac RV HTN ? opens foramen ovale ? paradoxical gas
embolism - Diagnosis
- HR, ?BP, ? CVP, hypoxia, cyanosis, ET CO2
biphasic change, ?a ETco2 ECG- Rt heart strain,
TEE, pulm art. Aspiration of gas/ foamy bld from
CVP line - Treatment
- Release source (stop co2 release pneumoperit)
- position steep head low durant position
- stop N2O 100O2
- Hyperventilation
- CVP/PA catheter to aspirate CO2
- Cardiac massage may break embolus- rapid
absorption - Hyperbaric o2 - cerebral embolism
- http//www.drsanjaykolte.in/
22
Endobronchial intubation
- Due to cephalad movement of diaph with head
down tilt and ? IAP - Diagnosis - Sp O2 ? airway P
- Treatment Repositioning of ETT
- http//www.drsanjaykolte.in/
23
Aspiration
- Mendelson syndrome
- At IAPgt20 mmHg
- Changes in LES due to IAP that maintain
transsphincteric P gradient head down position
protect against entry of gastric content in
airways - http//www.drsanjaykolte.in/
24
Nerve injuries
- Prevented by
- avoid overextension of arms
- padding at P points
- http//www.drsanjaykolte.in/
25
Laparoscopy in children
- Physiological changes adults
- Paco2 ETco2 increase but ETco2 overestimates
Paco2 - Co2 abs more rapid and intense due to larger
peritoneal SA / body wt. - More chances of trauma to liver during trocar
insertion - More chances of bradycardia , maintain IAP to as
low as possible - http//www.drsanjaykolte.in/
26
Laparoscopy in pregnancy
- Indications-
- appendicectomy
- cholecystectomy
- Risk preterm labour, miscarriage, fetal
acidosis - Timing II trimester (lt 23 wk)
- Lap technique HASSANS tech
- Special considerations
- prophylactic- antithrombolytic measures
tocolytics - operating time to be minimised
- IAP as low as possible
- Continous fetal monitoring (TVS)
- Lead shield to protect foetus if intraop
cholangiography needed - http//www.drsanjaykolte.in/