Program outline PowerPoint PPT Presentation
1 / 38
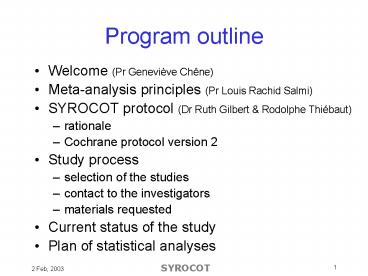
Title: Program outline
1
Program outline
- Welcome (Pr Geneviève Chêne)
- Meta-analysis principles (Pr Louis Rachid Salmi)
- SYROCOT protocol (Dr Ruth Gilbert Rodolphe
Thiébaut) - rationale
- Cochrane protocol version 2
- Study process
- selection of the studies
- contact to the investigators
- materials requested
- Current status of the study
- Plan of statistical analyses
2
SYstematic Review Of the effect of timing and
type of prenatal treatment on COngenital
Toxoplasmosis
- SYROCOT
www.isped.u-bordeaux2.fr/ISPED/RECHERCHE/SYROCOT/F
R-ISPED-SYROCOT.htm
3
Cochrane protocol version 2published in Issue 1,
2003
- Systematic Review on Congenital Toxoplasmosis
4
Rationale
- Question What is the effect of prenatal
treatment - On transmission from the mother to the child
- On clinical signs in the child
- Answer ?
- No randomised clinical trial
- Results from observational studies
- Discrepancies
- Methodological issues
5
Rationale
- What are the main methodological issues?
- Bias
- Systematic error
- Several kind of bias
- Heterogeneity
- Uncertainty
6
Rationale
S/C -
Serology
Transmission -
S/C
Clinical signs -
S or PS
Transmission
S and PS
Clinical signs
S and PS
Selection biasSerologyif suspicion
Indication biasPS if transmission
Confusion bias gestation at SC
Measurement and attrition bias(followed if
treated)
7
Rationale
- Selection bias
- Some women are referred for a serological
diagnosis because of a suspicion of signs in
fetus - Diagnosis of S/C and transmission at the same
time - No time lag to be treated
- Increased risk of transmission in untreated
patients
8
Rationale
- Confusion bias
Treatment
Transmission
Gestational age at seroconversion
9
Rationale
- Indication bias
- Women are treated because of a high risk of
infection in fetus - To be untreated seems to be protector
- Attrition bias
- Children with poorest prognostic are more likely
- followed (increase probability of finding signs)
- treated
- To be untreated seems to be protector because
signs are not diagnosed in this group
10
Rationale
- What are the main methodological issues?
- Bias
- Heterogeneity
- Due to type of screening, lab assays, treatment,
local epidemiology - Consequences
- A noise with few data
- An information with enough data
- Is there any factor that modifies the prenatal
treatment effect ? - Uncertainty
11
Rationale
- What are the main methodological issues?
- Bias
- Heterogeneity
- Uncertainty
- In evaluation of gestation at seroconversion
- Increase variability if taken into account
12
Rationale
- Arguments for a systematic review
- discrepancies in published results
- explore heterogeneity
- Arguments for an IPD analysis
- methods for taking into account the strong effect
of gestational age at maternal seroconversion
were often not consistent - differences in handling of potential biases
- lack of variability of treatment measure and / or
limited applicability
13
Objectives
- The study aims to explore the effect of the
timing and type of prenatal treatment on - a) mother to child transmission of T.gondii
- b) clinical manifestations in children with
congenital toxoplasmosis - With a special interest on the factors associated
with a variation of this effect (heterogeneity)
14
Structure
- The systematic is composed by two studies
- Mother to child transmission study
- Clinical manifestations study
- Three level of information are distinguished
- Study
- Centre
- Patient
15
Inclusion criteria for studies
- Transmission study
- Cohort studies identifying seroconverting women
by prenatal screening - Required data collected
- Dates of last negative / first positive test
- Prenatal treatment starting date
- Date of birth
- Congenital infection status based on serologic
status at 12 months postnatal age
16
Inclusion criteria for studies
- Clinical signs
- Cohort studies of children with congenital
toxoplasmosis identified by prenatal or neonatal
screening for maternal toxo - Required data collected
- Prenatal treatment starting date
- Date of birth
- Congenital infection status based on serologic
status at 12 months postnatal age - Results of at least one ophtalmoscopy or
intracranial imaging examination
17
Inclusion criteria for participants(primary
analyses)
- Transmission study
- delivery after 1979
- whatever the outcome of pregnancy
- infected women without a negative test during
pregnancy excluded - mother-child pairs suspected to have been
referred for testing due to problems excluded
18
Inclusion criteria for participants(primary
analyses)
- Signs study
- live born children with confirmed congenital
toxoplasmosis - mother-child pairs suspected to have been
referred for testing due to problems excluded
19
Types of outcome measure
- For transmission congenital infection
- Persistence of IgG beyond 12 months of age or in
fetal losses or postnatal death, a positive
culture or PCR result other criteria (PCR,) - Absence of congenital infection undetectable
specific IgG gt 2 mo of age - For signs clinical manifestations
- Retinochoroiditis
- Intracranial lesions
20
Search strategy
- Electronic search undertaken using
- MEDLINE (1980-2002)
- EMBASE (1980-2002)
- PASCAL (1987-2002)
- No language restriction
- Contact with experts and investigators
21
Methods of the review
- Abstracts scanned by two reviewers (RT RG)
- Eligible studies retrieved in hard copy
- If agree or at least one reviewer need
- Eligible studies assessed by two reviewers
against the inclusion criteria using a standard
checklist
22
Methods of the review
- Quality of observational studies
- Prospective or retrospective
- Available information
- Dates of first positive test, treatment starting
date, prenatal diagnosis - Congenital infection status based on IgG beyond
11 months - Results for ophtalmoscopy or intracranial imaging
examination
23
Study process
- Systematic Review on Congenital Toxoplasmosis
24
Study process
- Studies selection (see doc 1)
- Contact to investigator (see doc 2)
- Ask for eligibility, feasibility
- Ask for other potential eligible studies
- Sign agreement (see doc 3)
- Send datasets
- Data extraction (see doc 4)
25
Current status of the study
- Systematic Review on Congenital Toxoplasmosis
26
Current status (1)
27
Current status (2)
28
Current status
- Embase research
- N12 new papers
- N2 new studies
- N1 new cohort
- Pascal research
- Agreements
- 4/13 studies other than EMSCOT
- 8/13 centres from EMSCOT
29
Plan of statistical analyses
- Systematic Review on Congenital Toxoplasmosis
30
Principles
- Two analyses transmission and signs
- Main analyses dealing with issues as simply as
possible - Other analyses
- Secondary analyses
- Sensitivity analyses
31
Outcome
- For transmission congenital infection
- Persistence of IgG beyond 12 months of age or in
fetal losses or postnatal death, a positive
culture or PCR result - Absence of congenital infection undetectable
specific IgG gt 2 months of age - Other definitions
- IgM, IgA before 6 months
- PCR or culture of amniotic fluid or fetal
products - Clinician opinion
32
Outcome
- For signs clinical manifestations
- Signs in the first year of age
- Ocular and intracranial lesions are investigated
separately - Retinochoroiditis by ophtalmoscopy on at least
one examination - Intracranial lesions
- calcifications, hydrocephalus, ventricular
dilatation - analyses grouped by type of examination
33
Type of intervention
- Type of first prenatal treatment
- (Spiramycine, pyrimethamine-sulphonamide, none)
- Prenatal treatment delay
- the interval between seroconversion and start of
treatment (or delivery for untreated women) - as a continuous variable if the effect is linear
34
Covariates
- Patient level
- gestation at seronconversion
- postnatal treatment
- maternal age, year of birth, parity, length of
gestation - Centre level
- geographic situation
- test schedule
- (postnatal treatment)
- Study level
- Prospective / retrospective
- Quality score based on completeness
35
Main analysis
- Hierarchical model accounting for levels
(patient, centre, study) - Adjustment for potential confounders(gestation
at seroconversion) - Interaction of covariates with treatment effect
to study heterogeneity
36
Secondary analyses
- Effect of treatment throughout pregnancy
- Spir, Spir changed to PS, PS only, none
- Excluding women who underwent a prenatal
diagnosis for transmission analysis - Sub-group analysis on women who seroconverted
during late pregnancy for transmission analysis - Analysis including additional covariates
- type of delivery
- birth weight
- breastfeeding
37
Sensitivity analyses
- Handling of uncertainty of gestation at
seroconversion - Assess accuracy of outcome definition
- Effect of congenital infection definition
- Signs detected beyond 1 year
- Assessment of bias
- Publication bias (funnel plot)
- Selection bias (referred cases initially
excluded) - and any suggestions by investigators
38
Report of the results
- Based on MOOSE (Meta-analysis Of Observational
Studies in Epidemiology)Donna Stroup et al. JAMA
2000, 283 2008-12 - With a particular emphasis on
- heterogeneity assessment
- sensitivity testing