Case study 1 PowerPoint PPT Presentation
1 / 20
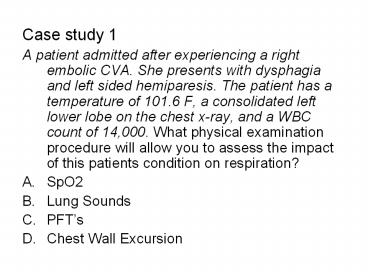
Title: Case study 1
1
- Case study 1
- A patient admitted after experiencing a right
embolic CVA. She presents with dysphagia and left
sided hemiparesis. The patient has a temperature
of 101.6 F, a consolidated left lower lobe on the
chest x-ray, and a WBC count of 14,000. What
physical examination procedure will allow you to
assess the impact of this patients condition on
respiration? - SpO2
- Lung Sounds
- PFTs
- Chest Wall Excursion
2
- Case study 1
- A patient admitted after experiencing a right
embolic CVA. She presents with dysphagia and left
sided hemiparesis. The patient has a temperature
of 101.6 F, a consolidated left lower lobe on the
chest x-ray, and a WBC count of 14,000. What will
be the goal of the first intervention for
improving airway clearance? - Strengthen expiratory muscles
- Improve inspiration
- Improve expiratory flow
- Position for bronchial drainage
3
- Case Study 2
- A patient with severe COPD presents to your
clinic with dyspnea, a barreled chest, digital
clubbing, and poor functional capacity. What is
the first physical examination you will perform? - Hoovers sign
- Chest wall excursion
- SpO2
- Blood Pressure
4
- Case Study 2
- A patient with severe COPD presents to your
clinic with dyspnea, a barreled chest, digital
clubbing, and poor functional capacity. There is
a positive Hoovers sign, so your next step is - Teach PLB and test again
- Teach diaphragmatic breathing and test again
- Test MIP and MEP
- Test chest wall excursion
5
- Case Study 3
- A patient with oxygen and steroid dependent COPD
is experiencing shortness or breath, RR 26, and
using accessory muscles. The patient is lying in
bed with HOB 45 degrees and being provided 4L of
oxygen by nasal cannula. What is the most likely
reason for this patients symptoms of respiratory
distress while lying in bed at rest? - Dynamic hyperinflation
- Poor use of accessory muscles
- Hypoxia
- Anxiety
6
- Case Study 3
- A patient with oxygen and steroid dependent COPD
is experiencing shortness or breath, RR 26, and
using accessory muscles. The patient is lying in
bed with HOB 45 degrees and being provided 4L of
oxygen by nasal cannula. How would you intervene? - Move to sitting, forward leaning with UEs
supported on a bedside table - Move to supine, UEs over head
- Move to prone, UEs out to side
- Move to standing, forward leaning
7
- Case Study 6
- A patient is admitted to the hospital with a
medical diagnosis of an acute exacerbation of
chronic bronchitis. What medical test will best
indicate to you how severe this condition is now
compared to baseline? - PFTs
- ABGs
- Pulsed Oximetry
- Chest X ray
8
- Case Study 6
- A patient is admitted to the hospital with a
medical diagnosis of an acute exacerbation of
chronic bronchitis. The first intervention for
improving the effectiveness of this patients
cough would be - Pursed lip breathing
- Huffing
- Expiratory muscle training
- Incentive spirometry
9
- Case Study 7
- A patient with severe COPD, polycythemia and an
increase in pulmonary artery (PA) pressure has a
primary complaint of dyspnea at rest with
occasional productive cough of white secretions.
The chest x-ray reveals bilateral hyperinflated
lungs with a flattened diaphragm. To determine
whether it is safe to proceed your first priority
should be to - Test whether SpO2 is less than 90
- Assess social status
- Assess smoking history
- Test whether there is a reversible component to
the hyperinflation
10
- Case Study 7
- A patient with severe COPD, polycythemia and an
increase in pulmonary artery (PA) pressure has a
primary complaint of dyspnea at rest with
occasional productive cough of white secretions.
The chest x-ray reveals bilateral hyperinflated
lungs with a flattened diaphragm. To determine
the degree to which PT will help this patient
your first priority should be to - Test whether SpO2 is less than 90
- Assess social status
- Assess smoking history
- Test whether there is a reversible component to
the hyperinflation
11
- Case study 14
- A 75 year-old male is admitted to the ER with
acute onset of chest pain and diaphoresis. He was
diagnosed with a NQMI and admitted to the floor
in a stable condition on a heparin drip, atenolol
(a beta blocker), and NTG as needed. The best
medical test to look for in determining whether
this patient will have limitations due to left
ventricular dysfunction is - Chest x ray
- Exercise stress test
- Dobutamine stress echo
- Angiogram
12
- Case study 14
- A 75 year-old male is admitted to the ER with
acute onset of chest pain and diaphoresis. He was
diagnosed with a NQMI and admitted to the floor
in a stable condition on a heparin drip, atenolol
(a beta blocker), and NTG as needed. The best PT
clinical assessment to determine whether
functional mobility is limited due to left
ventricular dysfunction is - Presence of Shortness of breath
- Blood pressure response to activity
- Heart rate response to activity
- Oximetry response to activity
13
- Case Study 15
- A patient admitted with an STEMI s/p CABG 2 2
days ago medications include atenolol, digoxin,
captopril and lasix is referred for PT. Blood
pressure is hypo responsive with ambulation and
HR becomes bradycardic. After rest the patient
recovers and stabilizes. For the next walk you
should examine - ECG
- SpO2
- Heart sounds
- Lung sounds
14
- Case Study 15
- A patient admitted with an STEMI s/p CABG 2 - 2
days ago medications include atenolol, digoxin,
captopril and lasix is referred for PT.
Recurrent ischemia would best be identified with - ECG
- SpO2
- Blood pressure
- Heart rate and rhythm
15
- Case Study 15
- A patient admitted with an STEMI s/p CABG 2 - 2
days ago medications include atenolol, digoxin,
captopril and lasix is referred for PT. This
patient should start exercising at - 65-85 of Max HR
- 50-60 of Max HR
- 16 18 RPE
- 10 12 RPE
16
- You are consulted to treat an 80 year old female
with past medical history significant for
coronary artery disease, LVH and diabetes, now
admitted to your facility with a medical
diagnosis of worsening left sided heart failure
and EF of 38. The best indication that this
patient is in CHF with activity would be - Shortness of breath
- Poor HR response
- Bilateral Pulmonary crackles
- S4 heart sound
17
- Case Study 17
- A 72 year-old patient has undergone a total knee
replacement 2 days ago, PMH includes CAD, IDDM,
and left sided systolic CHF with an EF 35.
Post operative HcT is 30. The best way to test
for signs of cardiac limitations associated with
the low oxygen carrying capacity would be to
examine ______ during activity. - SpO2
- Lung sounds
- ECG
- Blood pressure
18
- Case Study 20
- You are consulted to treat an individual with
dilated cardiomyopathy, LVEF 25 and BNP 900.
The patient presents with dyspnea and has poor
exercise tolerance. The best approach to examine
this patients response to activity - SpO2
- HR and Rhythm
- Blood Pressure
- ECG
19
- Case Study 20
- You are consulted to treat an individual with
dilated cardiomyopathy, LVEF 25 and BNP 1000.
The patient presents with dyspnea at rest and has
poor exercise tolerance. Since the patient is in
CHF you can expect - An S3 heart sound
- Tachycardia
- PVCs
- ST depression
20
- Case Study 23
- During the initial physical therapy evaluation of
your patient admitted with CHF in the skilled
nursing facility, you observe the patients
systolic blood pressure to drop 20 mm Hg below
resting levels with ambulation of 20 feet in 30
seconds. If medical management cannot be adjusted
for this patient, do you anticipate that this
patient will increase maximal aerobic capacity to
5 METs? - Yes
- No