THE ENEMIES PowerPoint PPT Presentation
1 / 61
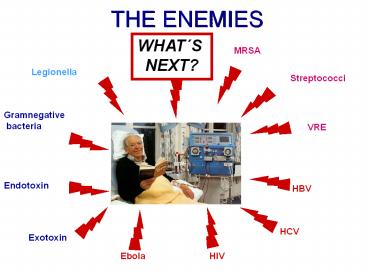
Title: THE ENEMIES
1
THE ENEMIES
WHATS NEXT?
MRSA
Legionella
Streptococci
Gramnegative bacteria
VRE
Endotoxin
HBV
HCV
Exotoxin
HIV
Ebola
2
RISK FOR INFECTION
1. Patient skin borne organisms at puncture by
start 2. Personnel transmitted organisms at
start 3. Patient skin borne organisms during
session 4. Equipment (by non proper disinfection
or reuse) 5. Water during session (back
filtration) 6. Personnel transmitted organisms
at termination 7. Patient skin borne organisms
at termination
3
THE CLINIC - A SYSTEMDISINFECTION WHAT IS
DIFFICULT - WHAT IS EASY?
Clinic
Bed
Dialysis machine fluid path
4
DISINFECTION
Is the stuff dangerous to inhale?
HRRMM It smells
Oh, Oh The surface looks funny
The guy who invented this has he ever used it
himself...
What about my hands
5
VIRUSHIV HBV
HBsAg
Glycoprotein 120
HBcAg
Phospholipid membrane
Capsid proteins
DNA
Reverse transcriptase
? 42 nm
RNA
Dane particle
Glycoprotein 41
Internal envelope proteine 17
? 100 - 140 nm
6
HYGIENE - DISINFECTION
I
N
C C C C C C
I
L
Z
D
O
C
C
E
N
B
E
Dialysis machine Surface
Dialysis machine Fluid pathway
7
HBV
1. HBsAg surface antigen 2. HBcAg core
antigen 3. DNA
The virus is not fully inactivated until the DNA
structure is destroyed
8
EBOLA
EBOLA VIRUS Filamentous virus Causes hemorrhagic
fever Multi organ disease Body fluids Sensitive
to heat
9
MRSA METHILLICIN RESISTANT STAPHYLOCOCCUS AUREUS
1975 First isolated at Royal Hospital,
Brisbane Australia 1975 1 case 1987 720cases
Sweden 2001 320 cases
Patients often moved to infection clinics
Resistant to all ?-lactam antibiotics including
methillicin
10
VREVANCOMYCIN RESISTANT ENTEROCOCCUS
Vancomycin is an antibiotic without
?-lactam Vancomycin is somewhat the last line
of defense Patients often moved to infection
clinics?
11
LEGIONELLA
FEATURE Air borne pathogen
Not transmitted from person to person
Inhaling of aerosol (shower, air
condition) Causes pneumonia
and Pontiac fever ACTION Chlorination of
water High temperature in hot
water plumbing RISK Immune depressed
patients
12
PRIONS INACTIVATION
- METHOD PROCESS REMARK
- Autoclaving 18 minutes 134 - 138 C
England - Autoclaving 30 minutes 134 C
France - Dry heat gt 12 hours 160 C
Not effective - Dry heat 1 hour 360 C
Not effective - Irradiation 100 kGy
Effective - Ethylene oxide
Not effective - Disinfection 1 hour 1 M NaOH
Effective - Disinfection 1 hour NaOCl (2.5 Cl)
Effective
13
MICRO-ORGANISMS
VIRUS Hepatitis B Hepatitis C HIV Ebola
WHAT DO THESE HAVE IN COMMON ??
We are today not able to handle and cure these
infections
BACTERIA MRSAVRE
14
HYGIENE
PATIENT personnel hygiene must not be
forgotten and it starts at home
- DIALYSIS SESSION
- Everything comes together
- Patient,
- Personnel
- Dialysis ward
- Dialysis machine
- Water
CATHETER The personal hygiene influences the
lifetime of catheters as well as conditions
during use
15
CATETHER INFECTIONS (vascular
catether related bloodstream infections)
USA
- Number of catheters purchased 150 000 000
- Estimated number of episodes 400 000
- Cost per episode (USD) 8 000 - 28
000 - Total cost (USD) 3.2 - 11.2
billions
16
CLEANING EQUIPMENT
The cleaning equipment must be maintained Cleanin
g personnel must be trained
17
DISINFECTANTS
- GROUP EXAMPLE ACTION
- Chlor Bleach
Oxidizing - Iodine Povidine iodine
Oxidizing - Alcohol Ethanol, iso-propanol
Protein denaturation - Detergents Cetylpyrinium chloride
Membrane - Phenol Phenol, hexachlorophen
Protein denaturation - Peroxide H2O2, peracetic acid
Oxidizing - Aldehydes HCHO, Glutaraldehyde Protein
denaturation - Heavy metals Silver
Protein denaturation
18
DISINFECTANTS
- What is the hygienic limits in air?
- Is the disinfectant dangerous to get on skin or
in the - eyes?
- Is the disinfectant compatible with materials to
be - disinfected?
- Can the disinfectant cause allergic reactions?
- Does the disinfectant has an odor?
- Is the disinfectant flammable? Explosive with
air? - What about build up on surfaces
19
HAND HYGIENE
Hand disinfection 60 Iso-propanol Let hands dry
Hand washing Mild soap Dry
20
DISINFECTANTS RELATIVE EFFECT
100
Soap and water
80
Zephiran 11000 (Quaternary NH4)
60
bacteria surviving
40
20
70 ethanol
1 chlorhexidine in 61 ethanol
10
0 20 40 60 80 100
120 Time (seconds)
21
DISINFECTION OF ARM
Chlorhexidine
22
SKIN DISINFECTANTS
Chlorhexidine gluconate 4 Chlorhexidine
gluconate
Chlorhexidine gluconate 1 Chlorhexidine
gluconate 61 Ethanol
FREKADERM 80 g Ethanol 0.1 g
Bensalkonium chloride 0.025 g 2- biphenylol 0.025
g 2-bensyl-4-chlorphenol Water to 100 g
SOFTASEPTN 74.1 g Ethanol 10.0 g
Isopropanol Water to 100 g
Exposure time 15 sec HBV 5 min
23
PUNCTATION
Face protection
Gloves
Protective clothing
24
FOOD IN THE CLINIC
25
PRESSURE TRANSDUCER
- Arterial and venous pressure transducers
0,2?m filter - 0,2?m filter in machine
- Extra filters can be used
- Blood coming through the filter in contact
with filter in blood line - Maintenance recommendations for machine 0,2?m
filter
26
TERMINATION
Risk of blood spill
27
DISMANTLED BLOOD LINE SET
Transport
Waste
28
BLOOD
S P L A S H
29
GARBAGE
Dialyser broken
Waste
30
SYRINGES AND CANNULAS
To be handled with care
31
DIALYSIS MACHINE FLUID PATH DISINFECTION
WHY DISINFECT? 1. To prevent microbial growth in
the dialysis machine 2. To inactivate
blood borne infections
WHEN IS DISINFECTION TO BE MADE? After each
session
32
VIRUSES IN BLOOD
- HEPATITIS B
- Concentration in blood 108 - 1011/ml
- Infective dose 1
- HEPATITIS C
- Concentration in blood 104/ml
- Infective dose 1 - 10
- HIV
- Concentration in blood 102 - 103/ml
- Infective dose 1
33
HBVESTIMATED LOAD
- Blood leak detected
- 1ml blood in 500 ml dialysate
- Assume 108 viruses/ml
- 0.1 will not be flushed out 104 viruses 4
log - 4 log must be inactivated
34
HEPATITIS BHEAT INACTIVATION 90C
log number
Minutes
Kobayashi 1984, Shikate 1978, RKI
35
THE WORLD OF VIRUS
- VIRUS
- Size of HBV 42 nm
- Dialyser size 30 cm
- 30 cm 42 nm 7 x 106 viruses
- How much is that??
- 1 virus ? 1 Human being (1.8 meter)
- Translated to human being 12 000 km
36
DIALYSIS MACHINE FLUID PATHRISK OF VIRUS TRANSFER
- Viruses can not multiply inside the fluid path
(host cell) - Viruses have no structures for motility
- Virus must move from position downstream dialyser
to position upstream dialyser. This distance is
translated to human being - Move from India - Sweden but without legs and
arms! - Fluid passes along dialyser membrane (by
filtration membrane rejects gt3 log/cm2 (high
flux) to gt6 log/cm2 (low flux) - Virus is subject to disinfection, damages occurs
- Few organisms remains in fluid path, bulk is
flushed out - The risk of virus transfer by fluid path is very
low!
37
VIRUS SURVIVAL
- Survival on surfaces hours - weeks
- Survival able to infect
- Protection by blood increases survival
- No reproduction outside host cell
- HBV Destruction of HBsAg is generally considered
as loss of infection capacity - (Kobayashi et al 1978)
38
CLEANING THE DIALYSIS MACHINE
NO EASY TASK.
BUT OTHER SURFACES ARE OFTEN WORSE
39
WHAT IS USED FOR DIALYSIS MACHINE SURFACE?
Water with mild detergent
Alcohol
Other
9
90
1
40
DISINFECTION
Lysotol Active component Fenoxy propanol
35 Surface disinfection Concentration
2.5 Exposure time - Disinfection Concentration
5 Exposure time15 minutes
SURFACE DISINFECTION Surface 50 dry after
1 minute Surface 100 dry after
3 minutes
41
DISINFECTION OF SURFACE
SURFACE
SURFACE
Unbroken film during exposure time
42
IS EVERY PART CLEAN?
Pump houses Holders Buttons Recesses Housing Backs
ide
43
DISINFECTION
For a manufaturer of a disinfectant EN 1041
(Bacteria 5 log reduction) EN 1275 (Fungi 4
log reduction) These investigations are made as
suspension tests
- For a user
- The user has a process
- Material to be disinfected
- Structure to be disinfected
- Exposure time
- Temperature of surface
- There is no strict rule for the process
44
ETHANOL
ORGANISM KILLING
TIME (SECONDS)
ETHANOL CONCENTRATION
60
70 80 Staphylococcus
aureus 15 15
10 Staphylococcus epidermis 30
30 - Streptococcus
pyogenes - -
90 Escherichia coli
60 30
30 Serratia marcescens -
10 - Salmonella
typhosa -
10 - Pseudomonas aeruginosa
- 10
- Mycobacterium tuberculosis 60
30 30
45
INACTIVATION OF VIRUS
HEPATITIS B AGENT CONCEN-
EXPOSURE TEMPERATURE
TRATION TIME C Na
hypochlorite 0.525 10 min
20 Iso-propanol 70
10 min 20 Iodophor
1 213 10 min
20 Ethanol 80
2 min 11 Heat
- 2 min
98
HIV AGENT CONCEN- EXPOSURE
TEMPERATURE TRATION
TIME C Na hypochlorite
0.1 2 - 10 min 21 -
25 Iso-propanol 35 2 - 10
min 21 - 25 H2O2
0.3 2 - 10 min 21 - 25 Ethanol
50 2 - 10min
21 - 25 Heat -
10 min 56
46
HBV
CHALLENGE Dried HBV plasma preparation with 108
CID/ml
DISINFECTANT SUBSTANCE CONCENTRATED PRODUCT
DILUTION Na-hypochlorite 500mg free
chlorine/l, pH 9.2
- Glutaraldehyde 2 pH 8.4
- Sporocidin
2 glutaraldehyde 7 phenol 1
16 Iso-propanol 70
- Iodophor
(80mg iodine/l, pH 2)
1 213
RESULT All tested disinfectants inactivated the
challenge solution
Bond et al J Clin Microbiol 18, 535- 538,1983
47
HEPATITIS C
- GERMANY
- 23 cases in 1 clinic (1994-1996)
- No separation of known cases
- CONCLUSION
- No specific cause could be adressed
- Enforced actions for cleaning of beds started
- Enforced surface disinfection
- USA
- Niu (1992,1993)
- CONCLUSION
- No specific cause could be adressed
- Adherance to universal precautions
- Aseptic technique
- Adequate cleaning and disinfection of
environmental surfaces
48
CASE HCV
CLINIC Clinic had 10 cases of HCV Blamed
dialysis machines, only one type
- SITUATION
- Clinic lacked hygiene plan
- Clinic lacked evidence of hygiene education of
the staff - Head nurse witnessed about crowding and stress
- More than one machine type found in use
- No separation of known cases of HCV
- Positioning of machines not in accordance with
- positions of suspected infection
- ACTIONS
- Clinic reorganised, more machines and staff
increased - Hygiene plan and education
RESULT No more cases of HCV
49
HCV
CLINIC Hygiene plan Identified positions, but
not separation PERSONNEL Protective
clothing Hand disinfection Gloves DIALYSIS
MACHINE Dialysis machine may be
dedicated Disinfectant when cleaning machine
external surface Dialysis machine disinfection
after each session PATIENT Screening OTHER Waste
handling
50
HEPATITIS BUSA
- 39 cases of 574 patients in 5 clinics (1994)
- Violations against hygiene rules in all cases
- Handdisinfection missing
- Exchange of gloves missing
- Screening missing
- Immunization missing
- Inconsequent separation of known cases
- CONCLUSION
- The virus can survive on surfaces in the close
environment and can be transfered by hands of
staff. - Not sufficient cleaned and disinfected surfaces
represents a risk situation
51
HEPATITIS BCAUSES
- Lack of knowledge
- Personal hygiene defience
- Insufficient screening of patients
- Insufficient separation of infected and
non-infected patients - Failure to immunize
52
HBV / HIV
CLINIC Hygiene plan Identified positions, mostly
separation PERSONNEL Immunisation Hand
disinfection Personal Gloves, face protection,
protective clothing DIALYSIS MACHINE Dialysis
machine mostly dedicated Disinfectant when
cleaning machine external surface Dialysis
machine disinfection after each
session PATIENT Screening Immunisation OTHER Was
te handling
53
VIRUS TRANSFER
?
Patient B No infection Virus must come in
blood contact
Patient A Virus positive Micro droplets comes on
hands or clothes or equipment
The transfer of viruses can be done by
personnel when they move from position to
position. These movements are generally
impossible to trace retrospective
54
INFECTED DIALYSIS MACHINE
Every session is a risk as reliable test results
are available at a later time
The normal dialysis machine disinfection process
is performed Cleaning as described in actual
Hygiene plan
55
DISPOSAL OF SALINE BAGS
ACTION Used saline bags are drained in the
wash-basin RISK Blood may occur which means risk
for blood borne infections PRECAUTION Let the
fluid be drained slowly Flush with low flow of
water, avoid aerosol Be observant and careful
with skin leisons when handling bags
56
ON LINE PREPARATION OF SUBSTITUTION FLUID FOR
HDF / HF
Filters responsible for cleaning of water
and concentrates
Filter responsible for sterility of substituion
fluid
The machine system must be able to deliver a
sterile fluid! Sterility can only achieved by
combination of use of a sterile filter with
sterilising capacity! Water and concentrates may
in some countries be considered as raw material
for drug production Remember that the patient
is given 3120 - 23400 litres/year!
57
WATER
Water system with preventive disinfection CFU/ml
at Qualification 0.01 - 0.08 (1000ml
filtered) Hosptital analysis CFU/ml
40 -120and 5 -10 fungi
(0.1 ml
analysed) Growth mainly Grampositive
cocci Second sampling confirmed original
qualification The hospital technique had
required 10 000 agar plates
58
CONCENTRATE
Acid concentrate There is nothing like
autosterile Bicarbonate Growth of specialised
microflora
59
SUMMARY
- Be aware that every session is a potential risk
- Cleaning of the environment
- High hygiene by terminating and start of session
- Hygiene plan must be established and implemented
- Screening of patients (HBV, HCV, HIV)
- Immunisation of patients and personnel (HBV)
- Separation of known cases
- Disinfection / cleaning of dialysis machine fluid
path - Education and transfer of knowledge
- Hygiene audits and HACCP
- (Hazard Analysis Critical Control Points)
60
(No Transcript)
61
INFECTION CONTROL IN A DIALYSIS UNIT
- 1st Asian Dialysis Course
- Dalian, China 3 - 7 June 2002
- Dr Rolf Nystrand