Blood: Cells PowerPoint PPT Presentation
1 / 29
Title: Blood: Cells
1
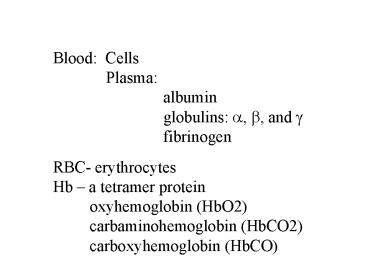
Blood Cells Plasma albumin globulins
?, ?, and ? fibrinogen RBC- erythrocytes
Hb a tetramer protein oxyhemoglobin
(HbO2) carbaminohemoglobin (HbCO2) carboxyhemogl
obin (HbCO)
2
- Factors that determine the binding affinity
- between Hb and O2
- Po2
- 2. pH (Bohr effect)
3
- Abnormality in Hb
- Sickle cell anemia - a genetic defect in Hb
- molecule ...
- The defect Hb crystallizes in low O2
- environment.
- Crystallized Hb bends RBC into sickle shape,
- which is rigid and fragile.
4
- In sickle cell anemia
- The sickled RBC cannot pass small vessels
- easily, which blocks capillary circulation
- and cause tissue ischemia.
- The sickled RBC are brittle
- The defect Hb does not have normal O2
- binding ability.
5
Production and destruction of RBC Erythropoiesis
- formation of red blood cells. Before birth,
RBC are produced in the liver and spleen.
After birth, they are mainly produced by red
bone marrow (sponge bones located in the end of
long bones or hip bones).
6
Erythropoietin (EPO) - a hormone that controls
the rate of RBC production. Kidneys produce
erythropoietin in response to low O2 levels in
blood . Erythropoietin stimulates the
differenciation and maturation of
proerythroblasts and erythroblasts Fig. 13.4
7
proerythroblasts
erythroblasts
8
Erythropoietin can be used to treat anemia.
When used on a healthy person, hematocrit can
reach to 65. Side effect high hematocret can
increase the burden to the heart and cause heart
damage or heart failure.
9
Vit. B12 and iron are also necessary for RBC
production. Vitamin B12 is absorbed in the
stomach in the presence of intrinsic factor.
Anemia caused by poor absorption of Vit. B12
is called pernicious anemia.
10
Aplastic Anemia Anemia due to destruction of
bone marrow, which may be caused by chemicals or
radiation. Treatment bone marrow
transplantation.
11
Destruction of RBC The average lifetime of RBC
is 120 days. When age, RBC become more
fragile. They can break by simply passing
through capillary vessels - hemolysis. Old
RBC can also be destroyed by macro- phages in the
liver (Kupffer cells) and spleen.
12
(No Transcript)
13
Hb in RBC are dissembled into different
components. Most Fe ions will be recycled to
bone marrow for erythropoiesis. Heme will be
changed into bilirubin (a pigment) and excreted
in bile juice into small intestines.
14
2), White Blood Cells (WBC) Granular
neutrophils eosinophils Leukocytes
basophils Agranular leukocytes.
Based on the lab staining, granular leukocytes
are divided into
15
- Neutrophils are the majority of WBC (60).
- Have lobed nucleus
- Phagocytic.
- Often be killed when digesting and killing
- bacteria - form puss.
- Their number usually increases during
- acute infection.
16
Eosinophiles, stained by acidic dye (red)
involved in parasites infection and allergy
reaction. Basophils, stained by basic dye
(blue) can release histamine, which is
responsible for inflammation.
17
- Agranular leukocytes
- Monocytes (or macrophages when enter tissues)
- Large phagocytic cells that can engulf large
- particles such as injured or infected body cells
- and digest them.
18
- Lymphocytes
- B-lymphocytes B cells (first found in chicken
bursa) - - B cells are produced and differentiated
- in bone marrow.
- - Responsible for antibody production
- T-lymphocytes T cells
- Thymus dependent cells, originated from
- thymus.
19
T-cells can be further divided into a. T
cytotoxic cell (TC) Kill infected body and
injured body cells, including tumor
cells b. T helper cells (TH) TH cells
stimulate functions of other T- and B-
lymphocytes. c. T suppressor cells (Ts) Ts
cell calms down immune response by
down-regulating Ts cells and B cell activity.
20
3), Platelets These are cell fragments of
megakaryocytes that exist in bone
marrow. Megakaryocytes manufacture proteins and
enzymes.
During their development, their cytoplasm shed
to produce little fragments - platelets.
One megakaryocyte ? 4000 platelets.
21
Functions of platelets a. transport
chemicals necessary for blood clotting, b.
form temporary patch on damaged vessel
wall c. secrete serotonin, which causes
vaso- constriction d. secrete platelet
derived growth factor (PDGF) to stimulate
growth of endothelial cells.
22
- Hemostasis - blood clotting, process of stop
- bleeding (p374-377).
- In the absence of vessel damage, plates are
- repelled from each other, and from the vessel
- wall - one of the mechanisms to prevent
- inappropriate blood clotting.
- Damage in endothelium of the vessel wall
- causes the exposure of collagen, which will
- stimulate the activation of platelets.
23
The activated platelets secrete serotonin that
causes vasoconstriction to decrease the blood
flow in the injured vessel.
24
The activated platelets also secrete clotting
factors for clotting reactions. There are 12
clotting factor (procoagulants) Ca (IV) and 11
proteins. Table 13.4. Platelets Factors III,
IV, V, VIII, and XIII. Liver factors I, II, V,
VII, XI, XII, and XIII
25
The process of hemostasis is formed by a
cascade of four stages 1). Vasoconstriction
(vascular phase) Spasm of the injured vessel - A
mechanism to minimize bleeding, lasts for 30
minutes.
26
- 2). Platelet plug formation (platelet phase)
- Platelets stick to the rough surface of a broken
- vessel (collagen) and also adhere to each other
- platelet aggregation.
- This platelet plug is enough to stop small
- bleeding but not enough for large wound.
27
3). Blood coagulation - The process of blood
clotting. The vascular and platelet phases
of hemostasis occur rapidly (a few seconds after
injury). The coagulation phase occurs 30
seconds later. It involves a cascade of
activation of a series of enzymes (clotting
factors).
28
Most of the 12 clotting factors are proenzymes,
which are activated one after another during
the coagulation phase. This cascade will lead
to the formation of fibrin network, which traps
more platelets and blood cells to form a big
clot...
29
Clotting factors are being activated