CASE I PowerPoint PPT Presentation
1 / 23
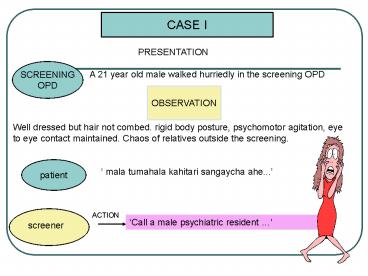
Title: CASE I
1
CASE I
PRESENTATION
SCREENING OPD
A 21 year old male walked hurriedly in the
screening OPD
OBSERVATION
Well dressed but hair not combed. rigid body
posture, psychomotor agitation, eye to eye
contact maintained. Chaos of relatives outside
the screening.
patient
mala tumahala kahitari sangaycha ahe...
ACTION
Call a male psychiatric resident
screener
2
HISTORY NOTED
- Irrelevant talking.3
- Desire to run away from home.2
- Catatonic hyperactivity, tightening of muscles.2
- Delusions 3
- 1. of God has given him power to protect
the world, he has sustain the suns severe heat
light, he can control every thing, he will
destroy the Evil powers...etc (grandiosity) - 2. of being poisoned by family members.
- 3. Evils are following him.(persecution).
- Dancing NAKED in fields, not responding to any
one.3 - Singing songs of MARRIAGE of ma, fa, sis, with
exaggerated MOOD, LAUGHING.3 - Olfactory Hallucination only in presence of
Parents.2 - Auditory Hallucination God talking to him to Save
India from Evil sprits.2
3
MENTAL STATUS EXAMINATION
- APPEARANCE- Well dressed, rigid body posture,
anxious look, occ staring - BEHAVIOR- Agitated but co-operative,
various furious gestures. - SENSORIUM- Oriented to T/P/P
- SPEECH- Talkative, tangential,
incoherent, pressured speech, singing- rhythmic - MOOD - Fluctuating- low, expansive,
euphoric - AFFECT- In congruent with mood
- THOUGHT- Flight of ideas, tangential,
delusions of grandiosity, persecution, - erotomania, thought
insertion, obsessions- - romantic ideas
- PERCEPTION- Auditory olfactory hallucinations
- MEMORY- Intact for both recent and past
events - JUDJEMENT- Poor
- INSIGHT- POOR, co-relation cause and
affect missing
PHYSICAL EXAMINATION- P- 80/ MIN, BP- 120/ 80
mm/hg, RS- CLEAR AEBE, CVS- NAD.
4
What is your clinical assessment? What is the
problem of this person? How do you like to
handle this problem? Which Homoeopathic medicine
you would like to prescribe for him?
5
ASSESSMENT REQUIRED
- CLINICAL DIAGNOSIS (differentials)
- STATE OF RELATIVES
- RISKS DANGERS INVOLVED IN MX OF VIOLENT PTS
- ACCEPTANCE OF THE CASE
- NEED FOR ISOLATION
- LENGTH OF STAY
6
Repertorizatn sheet
7
LEARNING
- IMPORTANCE OF INFRASTRUCTURE IN THE MANAGEMENT
OF PSYCHIATRIC PTS.
- IMPORTANCE OF THE JUDGEMENT OF CLINICIAN
- CLINICAL CONDITION
- AVAILABLE RESOURCES
- ANTICIPATION OF DANGERS
8
ACTION
Hyoscyamus 1M 2 hrly 4pills/ 1d
LEARNING
NO ADMISSSION Asked them to report on an OPD
basis. Limitations General hospital
Requirements for a mental hospital
Infrastructure Medical and non medical
staff
9
Scene II
MSE
APPEARANCE- Well-groomed, hairs not combed,
constant eye to eye contact, appearing calm
then yesterday. BEHAVIOR - Sitting
comfortably in chair, answering properly to all
questions, decreased agitation. SENSORIUM-
Oriented to T/P/P SPEECH- Tangential,
incoherent, continuous, occasionally loud
pressured MOOD AFFECT- Appropriate to time
circumstance. PERCEPTION- Auditory
hallucinations, olfactory hallucination
(decomposed meat) only in presence of
parents THOUGHT- Delusion of being
poisoned, delusion of persecution, delusion of
grandiosity, thought insertion
MEMORY- Intact for both recent and past
events JUDJEMENT- Poor INSIGHT-
Poor.
10
- Assessment of current status?
- Change from the previous state?
- Assessment of susceptibility?
- Reflect the same in the posology?
11
ACTION
Tub 1m single dose stat Hyoscyamus 10M 2 hrly
4pills Follow after 2 days on 13/02/09.
SCENE III
- According to the attendants
- c/o mainly in the early morning in afternoon.
- Better at level of aggression, lewd behavior,
irrelevant talking. - No lascivious mania. Singing dancing cont, but
intensity frequency reduced.
ACTION ????
12
ACTION
ADMISSION ORIENTATION TO PATIENT
RELATIVES DECISION TO ADMIT UNDER ISOLATION FOR
OBSERVATION
ORIENTATION
- Relative
- About clinical condition
- About the duration of stay
- About treatment modality in our setup and our
limitations. - Need for reference to a higher institute if
required.
WARD
OBSERVATION JUDGEMENT - ACTION CASE DEFINITION
13
THE LEARNING
THE LEARNING
KNOWLEDGE SKILLS Assessment- data collection?
diagnosis? assessing the clinical
State Management- mx patient relatives,
orientation, indication for admission Definition-
Elucidation of the problem in all
dimensions Treatment Indicated Acute Remedy,
assessment of susceptibility, potency selection
and repetition. Administration admission
process mechanism, procedure, responsibility
etc, accountability of pt. management role
distribution USE OF IPD- CONFIRMATION OF
DIAGNOSIS HOMOEOPATHIC CASE DEFINITION
REMEDY DIFFERENTIATION USING OBSERVED
FACTS OTHER THERAPEUTIC MANAGEMENT
14
IPD SCENE IV
200 am - pt was awake, lying quietly on bed,
eyes wide open. Fear of dark LIGHTS ON No
self talking, singing, lewd behavior. 500 am
lying quietly in the bed, covering his head. NO
sound of talking, singing. 700 am -restless3,
constantly clicking fingers. According to pt he
slept well at night without disturbance. No
olfactory hallucination, auditory
hallucination. No delusions, No irrelevant
talking, No singing dancing. 1030am - started
dancing2, singing2, clapping2. video
MSE
Appearance Behavior removed the t- shirt,
hair not combed, no eye to eye contact, singing
dancing, agitated impulsive, cont,making
jesters with hands restlessness. Attitude
Uncooperative. Memory Recent Remote
intact. Orientation- Impaired to T/P/P. Speech
Tangential, very fast incoherent, continuous,
loud pressured Thought delusion of
grandiosity3, thought insertion, sexual
fantasies2. Perception auditory
hallucination, olfactory hallucination gt2
15
- Totality
- Fear of dark2 at night.
- want light3
- delusion of grandiosity3
- sexual fantacies2
- Rx Stramonium 1M 1 DOSE STAT
11 20am On request of relatives Pt was send
for CT scan of brain. No dancing, clapping. No
irrelevant talking. Singing song in low voice.
Orientation to T/P/P intact Pt was quite
compliant while the traveling. 200 pm - Pt
lying quietly on bed. No irrelevant talking,
singing, dancing. 630 pm - Irrelevant talking,
singing, dancing started since 15min.
MSE Attitude and behavior- Non- cooperative,
aggressive, Exited , doing Karate. No singing,
dancing. Mood Affect Euphoric mood Speech
tangential, incoherent, occasionally loud
pressured. Thought delusion of being
poisoned2, delusion of persecution2, delusion
of grandiosity2
16
Rx Stramonium 1M 4Pills stat dose. (2nd
Dose) 1000 pm Continuous dancing3, singing
loudly3 since 1hour. Irrelevant talking 3.
Restless 3. Not responding to anybody. Opened
the tap of bathroom had bath completely wet
with clothes. Rx Stramonium 1M 4Pills stat dose.
(3rd Dose) 1100 pm Pt was very vigorous in
physical activity. On. Singing
dancing. Uncontrollable, very much
exiatable3. Rx Inj Serenace 1 amp IM stat.
video Slept with in 20 min. 700 am Con.
Roaming in room, restless, singing dancing,
clapping Want to take bath go to college. 800
am Pt lying quietly on bed. No irrelevant talk,
dancing, singing. No delusions, no
hallucinations. No thought insertion. 1215 pm
Occupational therapist Opinion taken. Adv.
Small task for reading of own interest, news
paper. Small problem solving task like
Su-dokoo. Walk in garden at evening for ½
hour. 345 pm responding well to commands. No
irrelevant talk, dancing, singing. No delusions,
no hallucinations.
17
1000 pm Started moving in room, irrelevant
talk No dancing, singing. No delusions, no
hallucinations. No thought insertion. 1100 pm
Rx Stramonium 1M 4Pills stat dose. (4th dose)
- CASE TAKING DAY 5
- TOTALITY-
- Anger suppressed3
- Sensitive to criticism3
- 3. Brooding tendency2
- 4. Extrovert2
- 5. C3H2
- Cr- milk2
- Hunger lt2
- Perspiration palms 2
- D/D- Nat mur, nat phos, staph,
Imp- Nat phos 200 1P HS on discharge
video
18
MANAGEMENT OF THE VIOLENT AND AGITATED PATIENT
19
SECLUSION AND RESTRAIN
INDICATIONS FOR HOSPITALIZATION-
- Prevention of imminent harm to the patient or
others when other means are - ineffective.
- Prevention of substantial damage to the physical
environment. - Prevention of serious disruption of the treatment
programme. - As a contingency of in the behavioral therapy of
dangerous pts. - Decreasing stimulation for an agitated pts.
Contradictions-
- 1.For the convenience or comfort of the staff or
to punish the patient. - 2.To accommodate a patients maladaptive request.
- For seclusion-
- The acutely suicidal,
- Self mutilating,
- Mentally retarded,
- Delirious,
- Demented,
- Acute Psychotic,
- Pt with seizure disorder,
- Pts with drug overdose.
20
PROCEDURE
- TAKE DOWN- Team of 5 adequately trained
professionals required. - Adequate rehearsals should be done to minimize
injury to anyone. - One member of the team assigned each limb,
another to protect pts head. - He would serve as the team leader and he would
instruct others throughout the procedure. He must
carry a mask or a soft cloth to cover the pts
mouth, in the event that biting or spitting
occurs. - Before approaching the pt clear the environment
of extraneous people and other physical hazards. - Bed with suitable mechanical restraints
injectable medications should be ready - Tie, scarves, long necklaces, dangling ear rings,
should be removed. - Team should be calm confident, yet be caring,
non threatening, non provocative - Pt should be carefully bought down on the ground
in supine position. - Head should be controlled in order to avoid
skull, neck or any facial injuries. - Head, trunk, extended legs are to be lifted
simultaneously with pts arms held close to the
side. - Pt should be transferred to the seclusion room
and restraints may be applied. - IM medication if indicated.
- If pt is not retrained team members should
release the limbs and walk out backward in a
sequential manner. - Documentation of the procedure with debriefing
session which will include a critique of the
procedure. - Care should be taken while dealing with elderly,
pregnant, MR, children etc.
21
QUESTIONS-
- Nature of agitation/ violence? actively violent/
verbally threatening?? - Duration?
- Medical history
- How did the pt arrive at the hospital?
- What are the medications / alcohol/ drugs?
ORDERS-
- Actively violent? call for help / security
- Physical restraints ? threat to himself or
others - Seclusion if necessary
- Order observation of vital signs, preliminary
medical tests if cooperative - Order medications only if needed.
THREAT TO SAFETY-
Do not approach without a plan ? potential
threat to safety and life of staff and self
22
QUICK LOOK-
- Evaluate mental status
- Posture tense, restless, ataxic
- Manner responding to stimuli,
threatening, demanding - Speech loud, cursing, slurred
- Motor activity gestures, destroying property
- Thought processes logical, illogical,
disorganized - Thought Content Paranoid ideation, delusional
- Perceptions illusions, auditory, visual,
tactile, olfactory hallucinations - Evaluate safety of the environment
- Vitals
- Selective history
MANAGEMENT- GOLDEN RULES
- Sufficiently trained staff.
- Avoid wearing hanging clothes, jewelry or loose
hair. - Assess the environment for dangerous objects.
- Avoid getting too close to the patient.
- Use clear and direct language.
- Avoid threatening behavior and remain calm in
voice. - g. DO NOT TRY TO BE A HERO!!!
23
MANAGEMENT contd.
- Verbally redirect the pt by talking to him/ her
and setting firm limits. - Offer oral medication
- If refused? seclusion, restraint, IM medications.
- Review the current, past medical psychiatric
histories. Follow up with - investigations to R/O or facilitate the
treatment of the underlying medical - Condition-
- Discontinuation or tapering of doses if agitation
due to medication. - Medicating the patient Lorezepam,
Haloperidol - Inform the police in case pt has threatened to
kill somebody, or in case - of anti social behavior.
- STAY IN WARD TILL THE AGITATION HAS BEEN RESOLVED
IN - ORDER TO OBSERVE THE MSE LATER..
- Once the patient is calm ? assess the cause and
treat appropriately.
Pt medically stable, not imminently dangerous,
not intoxicated, developed good impulse control,
would not benefit from further psychiatric
hospitalization
Discharge