Case Presentation PowerPoint PPT Presentation
1 / 21
Title: Case Presentation
1
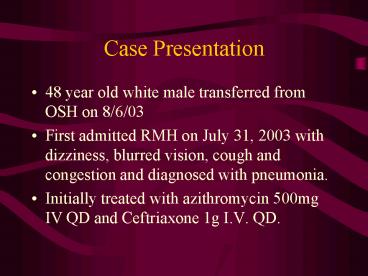
Case Presentation
- 48 year old white male transferred from OSH on
8/6/03 - First admitted RMH on July 31, 2003 with
dizziness, blurred vision, cough and congestion
and diagnosed with pneumonia. - Initially treated with azithromycin 500mg IV QD
and Ceftriaxone 1g I.V. QD.
2
History
- Initially did well, but then became progressively
dyspneic, and was readmitted on 8/3/03. - Subsequently intubated on 8/5/03 after developing
an ARDS like picture. - Vancomycin 1 g IV QD was added to his regimen and
he was transferred here.
3
Past Medical History
- Colon cancer in 1994
- Splenectomy in 1998
- Has a history of recurring folliculitis
- Treated for bronchitis with Gatifloxacin 2 to 3
weeks ago.
4
History Contd.
- Following this, he cut himself on his arm while
working in the yard. This required stitches and
he was also placed on Keflex. - Two days later he developed his current illness
and was admitted. - Soc Hx smokes 1 PPD No history of alcohol use.
Worked as a financial officer - Allergies Vancomycin causes itching.
5
Physical Exam
- Temp 99.7, BP 117/46 on dopamine at 6mcg/kg/min,
pulse 104, O2 Sats 100 on FIO2 of 80 - Alert and able to understand commands at
presentation. - Skin 3cm healed lesion on Left forearm with
sutures in place
6
Physical Exam
- HEENT Pupils equal, round and reactive to light.
No oropharyngeal erythema. - Lungs Coarse breath sounds with good air entry.
No Crackles - CVS Heart sounds were S1 and S2 only
- Abd Soft, non tender, bowel sounds positive
7
Physical Exam Contd.
- Neuro He was relatively alert. No focal
neurological deficits - Extremities 1 bilateral pedal edema. Dorsalis
pedis pulse was palpable on both sides. - Labs Na 142, K 3.7, BUN 22, Cr 1.7
- Lactate 7.0 WBC 32,500
8
Labs
- CXR shows bilateral patchy infiltrates
- Blood cultures from Richmond Memorial Hospital
drawn on 8/3/03 - One out of two cultures
9
Clostridium perfringens
- Gram positive, spore forming bacilli.
- All are obligate anaerobes, but C. perfringens is
relatively aerotolerant. - Histotoxic perfringens, ramosum, novyi,
septicum, bifermentans, sordellii - Enterotoxigenic perfringens and difficile
- Neurotoxic tetani and botulinum
10
Clostridium perfringens
11
Spectrum of Disease
- Traumatic setting surface contamination,
clostridial myonecrosis, uterine infection
(septic abortion), brain abscess. - Non-traumatic setting Post operative (bowel
surgery), septicemia, spontaneous. - Gastroenteritis C.perfringens food poisoning
12
Literature Review
- Rechner et al did a review in CID 200133349-353
- Reviewed clinical features of Clostridial
bacteremia in two hospitals in La Crosse,
Wisconsin. - City of 50,000, with a large surrounding rural
population
13
Methods
- Retrospective study that reviewed all positive
blood cultures for Clostridium species from
1-1-90 to 12-31-97. - Exhaustive review of the charts was done in whom
bacteremia or septicemia was determined to have
occurred
14
Results
- Of 63,296 samples, 74 were positive for
Clostridium species (0.12). - Samples obtained from 46 patients out of a total
of 164,304 hospitalizations for an incidence of
0.03. - Most common was C. Perfringens, followed by C.
septicum.
15
Results 2
- 102 isolates of C.Perfringens that were recovered
were 100 susceptible to penicillin. - Intestinal tract was the major source of
Clostridial bacteremia. - No cases of clostridial myonecrosis developed.
16
Results 3
- Only one patient had an infection related to farm
trauma. This was due to a rectal leak following a
pelvic fracture. - One patient developed severe hemolysis from
overwhelming C. Perfringens septicemia.
Hemoglobin was 11 mg/dl, and hematocrit 2. She
died of septic shock and multi-organ failure.
17
Results 4
- Overall mortality was 48.
- Reflects poor general condition of patients.
- Clostridial virulence less of a problem
- Conclude that it is a potentially serious
clinical marker because of severity of associated
illness in elderly and immunocompromised
patients.
18
Urban hospital
- Gregory Meyers et al Surg, Gyn Obst, April
1992, Vol 174 291-296 - 56 patients at the New York Hospital with
positive clostridial blood cultures. - 22 were immunosuppressed, 28 had a malignancy
usually gastrointestinal - GI source of Clostridia presumed in 43 of 56
patients
19
Urban hospital 2
- C. perfringens was the most common, but
C.septicum had the highest mortality. - Mortality was highest in immunosuppressed
patients. - Recommend a thorough search of a GI source in
such patients.
20
Our Patient
- Has a history of colon cancer, although
colonoscopy was unremarkable. - Remains intubated in ICU in a critical condition.
- Was treated with high dose penicillin.
- Arm wound does not appear to be a source of the
Clostridium.
21
Conclusion
- C. perfringens sepsis is an infrequent finding.
- Most common in immunosuppressed.
- GI source most likely, with a high association
with GI malignancy. - Mortality is high, more due to underlying
conditions, rather than the virulence of
C.perfringens