David ColinThom PowerPoint PPT Presentation
1 / 24
Title: David ColinThom
1
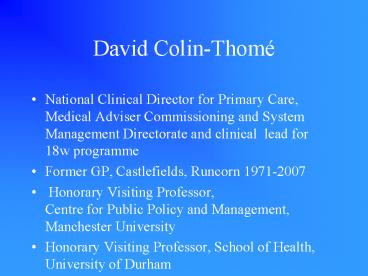
David Colin-Thomé
- National Clinical Director for Primary Care,
Medical Adviser Commissioning and System
Management Directorate and clinical lead for 18w
programme - Former GP, Castlefields, Runcorn 1971-2007
- Honorary Visiting Professor,Centre for Public
Policy and Management, Manchester University - Honorary Visiting Professor, School of Health,
University of Durham
2
Health Gain
- it is estimated that about five years of the
30-year increase in life expectancy in the 20th
century can be attributed to the provision of
health care (Bunker et al., 1994). The most
significant reason for this gain is the diagnosis
and treatment of coronary heart disease which
contributes one to two years of these additional
years of life.
3
CHD
- healthcare is delivering an increasing share of
improvements in life expectancy. For example,
42 of the decrease in coronary heart disease
(CHD) mortality between 1981 and 2000 is
attributable to healthcare (1)
1 Unal B, Critchley JA, Capewell S. Explaining
the decline in coronary heart disease mortality
in England and Wales between 1981 and 2000.
Circulation 2004 109 1101-07.
4
- Personal health services have a relatively
greater impact on severity (including death) than
on incidence. As inequities in severity of health
problems (including disability, death, and
co-morbidity) are even greater than are
inequities in incidence of health problems,
appropriate health services have a major role to
play in reducing inequities in health.
Starfield 12/03 03-385
5
Chronic Disease definition epidemiology
- This places new long term demands on health
care systems. Not only will chronic conditions
be the leading cause of disability throughout the
world by 2020 if not successfully managed they
will become the most expensive problems faced by
our health care system. WHO, 2002 1
6
The New Clinical Paradigm
- While the global disease burden has been
shifting towards chronic conditions, health
systems have not evolved to meet this changing
demand. Care is fragmented, focused on acute and
emergent symptoms, and often provided without the
benefit of complete medical information WHO
(2002) 1
7
LTC
- 50 of people with LTCs have not been told about
treatment options - 25 do not have care plan
- 50 do not have a self care plan
- 50 medicines are not taken as intended.
8
(No Transcript)
9
Public Service Agreement
10
LTC updates
- Hospital Episodes Statistics (HES) 2005/06 data
on emergency bed days on December 06 is showing
a 5.4reduction in emergency bed days in PSA
2003/04 target baseline (some 1.7million bed
days) despite a 5 increase in emergency
admissions in 05-06 - Official launch of the Combined Predictive Model,
the final tool delivered by the Kings Fund.
This tool combines both hospital and GP data to
not only increase positive power of prediction
but predict people who have never had a hospital
admission.
11
Choice
- Choice embraces three key components designed to
improve peoples overall experience by providing
them with more - Power to shape their pathway through services and
keep control over their lives - Preferences to choose how, when, where and what
treatments they receive - Personalised services organised around their
lifestyles
12
Primary Care Reform
- GP contracts
- Fairness in PC
- Quality and Outcomes Framework
- Pharmacists contract
- Nurse leadership (other clinicians)
- Practitioners with Special (clinical) Interests
- Practice Based Commissioning
- Capital into primary care
- Primary care services as social capital
13
Our health, our care ,our say a new direction
for community services (www.tso.co.uk/bookshop)
- Ambition
- Enabling health, independence and well being
- Better access to GP
- Better access to community services
- Support for people with longer term needs
- Care close to home
- Ensuring reforms put people in control
- Making sure change happens
14
Range of White Paper LTC commitments
- Bigger emphasis on self care and integration
- Requirement for multidisciplinary teams/networks
- Universal case management for VHIUs
- Personal Health and Care Plans
- Assistive Technology
- 24/7 single point of contact for people with
complex needs
15
Care Plans
- In addition the White Paper Our Health Our Care
Our Say makes a commitment - By 2008 we would expect everyone with both long
term health and social care needs to have an
integrated care plan if they want one. By 2010
we would expect everyone with a long term
condition to be offered a care plan. We will
issue good practice guidance in early 2007.
16
Benefits of a first contact in primary
care.(Starfield)
- Higher patient satisfaction with health services
- Lower overall HS expenditure
- Better population health indicators
- Fewer drugs prescribed per head of population
- The higher the number of family physicians the
lower the hospitalisation rate.
17
General Practice(Roland and Wilson)
We identify three areas in which British general
practice performs well, leading both
international policy analysts and the public to
their favourable conclusions Equity
Quality Efficiency and three important
characteristics that contribute to this
success Co-ordination Continuity
Comprehensiveness
18
General Practice and Health Inequalities (Roland)
- Practices in affluent and deprived areas
achieving the target of over 80 of eligible
women having received a cervical smear. The
figure shows not only that overall rates are high
and have increased since 1990, but that there has
been progressive narrowing of the difference
between affluent and deprived districts since
1990 . Similar narrowing in the social gradient
for childhood immunisation is seen in this period
. - Early evidence similar in QOF
19
Keeping it Personal
- Build on the best of traditional General Practice
- Primary Health Care more than general practice
- but registered population and 80 of all NHS
clinical consultations - 90 of care solely undertaken in primary care
- Support for self care
- Long term conditions management
- Care Closer to home
- The practice can link the wider publics health
and bio-clinical care
20
Next Stages review-Darzi (1)
- Journey so far. Improvement but.
- World class NHS-
- -fair-SoS announced strategy for reducing health
inequalities, - -personalised now to focus on primary care and
LTC, - -effective-Health Innovations Council
- - safe-Patient Safety Direct to support NPSA AND
reduce rates of Health Care Associated Iinfections
21
Next Stages review-Darzi (1)
- Major hospital change is clinically led and
locally accountable - And also subject to independent clinical and
managerial assessment before out to consultation
22
Next Stages review-Darzi (2)
- Deliver vision across eight areas of care
- -Maternity and newborn
- -Childrens health
- -Planned care
- -Mental health
- -Staying healthy
- -Long term conditions
- -Acute care
- -End of life care
23
Next Stages review-Darzi (2)
- Exploring the introduction of an NHS
constitution-CE to lead - Future strategy on primary and community care
24
Issues
- LA is the public health organisation
- And LTC is ?bulk of adult social care
- My experience is that best outcomes and less need
for hospital is when social care is working
closely with NHS in particular primary care - So given the better funding for the NHS should
NHS not be funding more social care? - NHS is adequately funded if we challenged
inappropriate and ineffective care - Whither personal budgets?
- Is not the pathway the patients/clients?
- Who are the providers?
- Networks/Multi disciplinary accountability?
- Who wants to be the principal provider?
- So leadership locally an issue